Since accurate etiologies remained elusive over the centuries, treatment also continued to remain so. First appendectomy was done by Amyand in 1735, when he was operating for an inguinal hernia [1]. It took another 150 years before early appendectomy was advocated as a treatment for this condition. Various modifications were proposed, accepted and rejected over next several decades, but most noticeable was the advent of laparoscopic approach.Yet, laparoscopic approach was never as well embraced by surgeons as its cholecystectomy counterpart. As patients transcended into clients, further developments were sought, initial step was improving patient satisfaction by reducing size and number of ports. With technological improvements in laparoscopic imaging equipment and instruments this need was first fulfilled by a laparoscopic appendectomy through a single umbilical incision. Progression to ‘scarless’ surgery through natural orifices is the next logical step.
Several studies have compared open and laparoscopic cholecystectomy, while others have compared different laparoscopic approaches. However, there seems to a paucity of literature comprehensively comparing open, conventional laparoscopic and single incision laparoscopic appendectomy in a prospectively conducted RCT providing an evidence of satisfactory quality. This study was done in an attempt to comprehensively address these three approaches to appendectomy, and encourage adoption of laparoscopic approach in this remote part of the country, if found to be superior.
Materials and Methods
The study was designed as a prospective double blinded randomized controlled comparison of three treatment modalities [designated as intervention groups] viz OA, CLA and SPLA. The study was conducted in Sikkim Manipal Institute of Medical Sciences, Gangtok, Sikkim in North East India for a duration of 18 months from January 2014 to June 2015. The study was approved by the research protocol evaluation committee and ethical clearance was obtained from the Institutional Ethical Committee.
All the patients who underwent appendectomy formed the population group. Inclusion criteria into the study group were patients willingness for randomisation, diagnosis of ‘simple’ appendicitis supported by ultrasonography and age between 12 and 50 years. Any contraindication to general anaesthesia, comorbidities other than hypertension and diabetes mellitus, ‘complicated’ appendicitis [perforation, abscess, and lump] and technical glitches leading to ergonomic difficulties were major exclusions.
An audio visual interactive session of 15 minutes about appendicitis, appendectomy and process of randomization was planned with the patients and their relatives to convince them and help them reaching a decision. They were communicated that they could choose procedure of their choice but if consented to be included in the study they would be randomized and might not know about what procedure they had undergone until 24 hours following surgery.
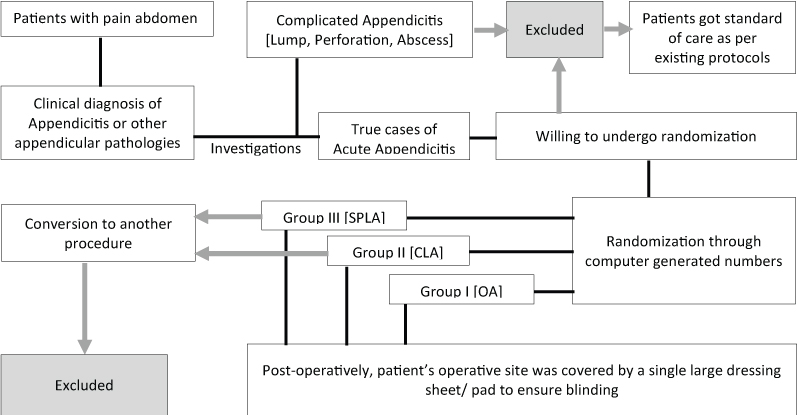
All patients were operated under general anaesthesia and abdomen was covered with a large dressing which was removed only after 24 hours to ensure blinding at patients end. They were also assured that they would get the standard care as per hospital protocol irrespective of their decision for inclusion into the study. Patients were then randomized using computer generated random numbers in to three intervention arms. Blinding was also ensured at investigators end by forming four teams, 1st for counselling and randomization, 2nd for operative intervention, 3rd for recording of data and last for analysis. All three operative interventions were standardized by a team of experts in the department of surgery after careful review of literature. Operative team remained strictly adhered to protocols and sequence of steps during entire study duration. Final outcomes were shared only after the last team analyzed whole data [Table/Fig-1 and 2].
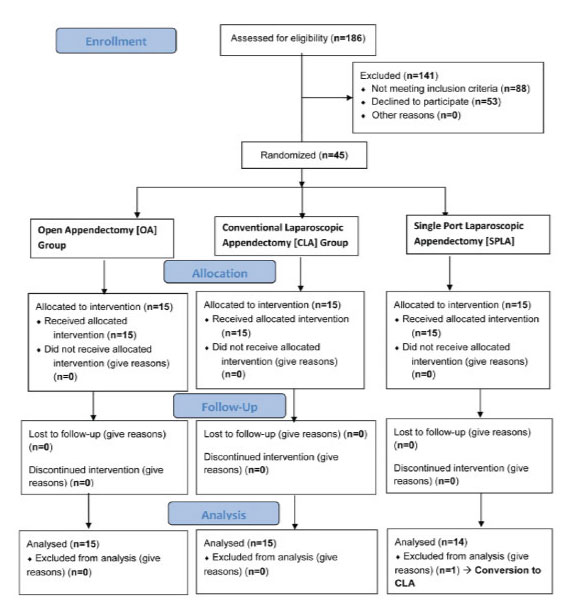
Flowchart showing the scheme of study.
Results
Over a duration of 18 months, 186 appendectomies were performed in our institute. From this population group, 45 patients were selected to form the study group who fulfilled inclusion criteria. Patients were then randomized to undergo one of the three procedures. All treatment arms received equal number of patients but one patient in SPLA group was converted to CLA and excluded from final analysis.
There was no difference in patients characteristics when population, study group and intervention groups were matched for age, sex and BMI [Table/Fig-3].
Patients were matched for their age, sex and BMI.
| Patient Characteristics | N | Gender* | Procedure* |
|---|
| Population | Study | Female | Male | OA | CLA | SPLA |
|---|
| Age | 12-20 | 16 | 2 | 2 | 0 | 0 | 1 | 1 |
| 21-30 | 74 | 26 | 16 | 10 | 9 | 10 | 7 |
| 31-40 | 38 | 15 | 7 | 8 | 5 | 4 | 6 |
| 41-50 | 22 | 1 | 0 | 1 | 1 | 0 | 0 |
| Total | 150** | 44 | 25 | 19 | 15 | 15 | 14 |
| df/p [χ2] | 3/ 0.064 | 3/ 0.296 | 6/ 0.693 |
| Mean | 30.79 | 28.80 | 27.96 | 29.89 | 31.27 | 27.40 | 27.64 |
| df/F/p [ANOVA] | 1,192/ 1.597/ 0.205 | 1,42/ 1.181/ 0.283 | 2,41/ 2.136/ 0.131 |
| Gender | Females | 106 | 25 | -- | 8 | 9 | 8 |
| Males | 80 | 19 | -- | 7 | 6 | 6 |
| Total | 186 | 44 | -- | 15 | 15 | 14 |
| F:M Ratio | 1.32 | 1.31 | -- | 1.14 | 1.5 | 1.33 |
| df/p [χ2] | 1/ 0.930 | -- | 2/ 0.934 |
| BMI | <18.5 | 29 | 5 | 4 | 1 | 2 | 1 | 2 |
| 18.5-25 | 65 | 23 | 13 | 10 | 8 | 8 | 7 |
| >25-30 | 58 | 11 | 5 | 6 | 5 | 4 | 2 |
| >30 | 34 | 5 | 3 | 2 | 0 | 2 | 3 |
| Total | 186 | 44 | 25 | 19 | 15 | 15 | 14 |
| df/p [χ2] | 3/ 0.842 | 3/ 0.638 | 6/ 0.603 |
| Mean | 23.7 | 24.3 | 23.68 | 25.10 | 23.76 | 24.72 | 24.42 |
| df/F/p [ANOVA] | 1,228/ 1.973/ 0.161 | 2,41/ 1.176/ 0.284 | 2,41/ 0.188/ 0.829 |
*Within the study group;
**Patients below 12 years and above 50 years have not been shown.
Duration of pain or presentation, history of previous surgery, initial visualized organ on putting laparoscope, adhesions and locations of appendix were studied and have been shown in [Table/Fig-4].
Clinical Characteristics.
| Characteristics/ Parameters | N | Procedure |
|---|
| OA | CLA | SPLA |
|---|
| Mean duration of pain [days] [p=0.609] | - | 1.7 | 2.07 | 2.0 |
| Comorbidities | Hypertension | 4 | 2 | 1 | 1 |
| Diabetes | 1 | 1 | 0 | 0 |
| Previous operative scarA | 2 | 0 | 1 | 1 |
| Organ first visualizedB [p=0.842] | Appendix | 21 | 7 | 9 | 5 |
| Caecum | 10 | 4 | 3 | 3 |
| Omentum | 5 | 2 | 1 | 2 |
| Small bowel | 8 | 2 | 2 | 4 |
| Patients with adhesionsC | 23 | 8 | 8 | 7 |
| Organ adhered to appendixD [p=0.738]E | Omentum | 13 | 4 | 4 | 5 |
| Small bowel | 16 | 7 | 6 | 3 |
| Anterior abdominal wallF | 4 | 1 | 2 | 1 |
| Transverse colon | 1 | 0 | 1 | 0 |
| Location of appendixG [p=0.202] | Retrocaecal | 4 | 1 | 3 | 0 |
| ParacaecalH | 21 | 6 | 8 | 7 |
| Preileal | 2 | 2 | 0 | 0 |
| PelvicI | 17 | 6 | 4 | 7 |
| Intraoperative complications | Bleeding | 1J | 1 | 0 | 0 |
| Spillage from appendix | 1J | 1 | 0 | 0 |
ABoth female patients, with Pfannenstiel scar; BChances of appendix visualization less with longer pain history [p<0.001], no impact by Gender [p=0.263] and BMI [p=0.932]; CPatients with BMI<25 [p=0.039] and pain ≥3 days [p=0.017] developed adhesions more commonly; DNo adhesions with sigmoid colon and right ovary, so excluded from final analysis; EPresence versus absence of adhesions; FMore common with pain of ≥3 days [p=0.001]; GNo impact on duration of pain [p=0.807]; Common in femalesH and malesI; J Both complications in same patient.
Overall mean duration of surgery was a little more than an hour [65.18 minutes]. SPLA took maximum time [82.79 minutes] but difference between OA and CLA was not even one second [OA= 56.93, CLA= 57.00 minutes] [p=0.018]. Minimum duration of surgery was almost similar in all arms, least in CLA [25 minutes in CLA, 30 minutes each in OA and SPLA]. In patients with BMI <25 [n=28, 63.6%], OA took significantly less time [54 minutes] compared to CLA [62 minutes] and SPLA [89.44 minutes] [p=0.013]. In contrast, in patients with BMI >25 [n=16, 36.4%], duration of surgery was least in CLA [49.5 minutes] followed by OA and SPLA [62.8 and 70.8 minutes] [p=0.525]. Duration of surgery in patients with pain <3 days [n=33, 75%] was 61.15 minutes and in those with ≥3 days [n=11, 25%] was 77.27 minutes [p=0.110]. When treatment arms were compared within those who presented with a shorter duration pain [<3 days], CLA took significantly less time compared to other two procedures [OA=58.0, CLA=46.8, SPLA=79.6 minutes; p=0.027].
Significant statistical difference was noted in postoperative pain perception, measured as visual analog scale score [VASS], among three treatment arms [Table/Fig-5].
Mean Visual Analog Scale Score [VASS] in postoperative period across three treatment arms. Dotted red denotes overall mean, yellow OA, blue CLA and green SPLA. Numerals against VAS indicates postoperative hour, DIS=discharge, D10=10th follow up day.
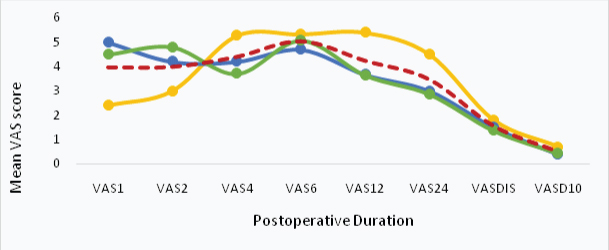
Overall mean VASS was maximum [5.05/10] at 6th hour. Mean VASS in immediate postoperative period (first and second hour) was higher for CLA (5.07, 4.27) and SPLA (4.5, 4.79) compared to OA (2.4, 3.0) (p<0.001 and 0.001). Pattern of VASS started reversing at 4th hour when we found it to be higher for OA (5.27) than CLA (4.2) and SPLA (3.71) (p=0.001). VASS at six hours remained elevated for all treatment arms and was comparable to overall mean (5.05) (p=0.387). VASS at 12 hours and 24 hours remained high for OA (5.4 and 4.53) compared to CLA (3.67 and 3) and SPLA (3.64 and 2.86) (p<0.001 for both 12 and 24 hours). VASS at discharge and at 10th postoperative day was substantially low for all procedures (p=0.121 and 0.237). No significant difference could be established in VASS at any point of time following surgery when VASS was compared among different age-groups and between genders. Difference was significant in VASS at first postoperative hour among patients in the BMI sub-groups (6 for BMI>30, 2.8 for BMI≤18.5, p=0.007) as well as at six hours (5.4 for BMI>30, 4.65 for BMI=18.5-25, p=0.041). BMI groups were also significantly different (0 for BMI>30 and 1 for BMI≤18.5) from each other for VASS at 10th day (p=0.023).
Postoperative pain was significantly higher as the duration of surgery increased. Difference noted in mean VASS at 2nd hour was significant (6 for >120 minutes, 3.44 for 31-60 minutes; p=0.047) as was at 4th hour (4.94 for 31-60 minutes, 3.5 for 61-90 minutes, p=0.016) and 12 hours (5 for >120 minutes, 3.33 for 61-90 minutes, p=0.032). The patients who complained of pain, though mild (VASS=2), even at day 10 following surgery, had a longer duration of surgery (88 minutes against overall 65.18 minutes). No significant difference was found for comparison made between VASS at various points of time and presence of adhesions except for higher VASS at 4th postoperative hour in patients having omental adhesions (p=0.047) and at 2nd hour for patients having small bowel adhesions (p=0.006). Location of appendix did not show any bearing on VASS except for VASS at 24 hours for preileal location (six for preileal, <3.5 for others, p=0.019).
In the first hour following surgery, requirement of analgesia was significantly higher for patients who underwent either CLA or SPLA than those who underwent OA (p=0.038). Analgesia requirement again surged at 4th postoperative hour but it was now more for OA than for CLA and SPLA (p=0.072). Thereafter, in patients undergoing OA, additional analgesia continued to be needed by patients at the end of 12 (p<0.001) and 24 hours (p=0.002).
Postoperative nausea and vomiting remained less frequently occurred entity as only two patients suffered from it that too who underwent OA. Vital parameters [pulse rate, blood pressure, respiratory rate, temperature and transcutaneous oxygen saturation (SpO2)] were recorded simultaneously with VASS and analgesia requirement. Difference found in any parameter among treatment arms or among various other groups based on age, gender, BMI or duration of surgery was not significant.
Almost 45% patients had their bowel sounds heard at two hours following surgery (OA=6, CLA=6, SPLA=8). Number of patients whose bowel sounds were present at the end of six hours rose to 75% (OA=9, CLA and SPLA each=12). Mean duration after which bowel sounds appeared in OA, CLA and SPLA was 6.27, 4.8 and 3.86 hours, respectively (p=0.336).
Wound infection remained low in the study (4, 9.1%). Out of these four patients, two patients underwent OA and one each CLA and SPLA (p=0.780). Overall mean duration of hospital stay was 3.68 days. Patients who underwent OA stayed for a significantly longer duration (OA=5.27, CLA=2.4, SPLA=3.36 days, p=0.048). Patients who underwent CLA and SPLA resumed their usual daily schedule [calculated as return to job] almost a week earlier (13.2 and 13 days, respectively) than OA (19.73 days) (p<0.001). Mean patient scar acceptance scale (PSAS) was 25.57 ranked as mostly acceptable to patients. PSAS was highest for patients who underwent OA (37.93) (CILA=20.60, SPLA=17.64, p<0.001). Scar acceptability was no different between the two genders. Overall mean patient satisfaction score was 113.36. Patient satisfaction was almost similar in all treatment arms (OA=112.27, CILA=113.8, SPLA=114.07, p=0.762). Mean cost of treatment in OA and CLA was INR 13,963.33 and INR 14,150.20 compared to SPLA which cost INR 23049.86 (p=0.003) [Table/Fig-6].
| Parameter | Mean |
|---|
| OA | CLA | SPLA | p |
|---|
| Bowel sounds | 6.27 | 4.8 | 3.86 | 0.336 |
| Hospital stay | 5.27 | 2.4 | 3.36 | 0.048 |
| Resumption of job | 19.73 | 13.2 | 13 | <0.001 |
| PSAS | 37.93 | 20.6 | 17.64 | <0.001 |
| Patient satisfaction | 112.27 | 113.8 | 114.07 | 0.762 |
| Treatment cost [INR] | 13963.33 | 14150.20 | 23049.86 | 0.003 |
Discussion
Most of literature available regarding comparison of open and minimal invasive approach, especially SPLA is recent and whatever is available, is still sparse in finding out good study designs involving SPLA. This is further complicated by the fact that there is no standardization of SPLA, with various studies involving a unique way of doing it. A comprehensive comparison of designs of studies done in last 10 years is presented in [Table/Fig-7].
Comparison of various study designs.
| Author | Year | Place | Sample size | Study design | Procedure |
|---|
| Present | 2014 | India | 44 | RCT, double blinded | OA, CLA, SPLA |
| Minutolo V et al., [2] | 2014 | Italy | 230 | Retrospective | OA, CLA |
| Sateesh et al., [3] | 2014 | India | 50 | Prospective, observational | CLA, SPLA |
| Frutos et al., [4] | 2013 | Spain | 184 | RCT | CLA, SPLA |
| Baik SM et al., [5] | 2013 | Korea | 89 | Prospective, observational | CLA, SPLA |
| Liang HH et al., [6] | 2013 | Taiwan | 688 | Retrospective | CLA, SPLA |
| Kang J et al., [7] | 2012 | Korea | 217 | RCT | CLA, SPLA |
| Lee JS et al., [8] | 2012 | Korea | 63 | Retrospective | CLA, SPLA |
| Goudhar BV et al., [9] | 2011 | India | 204 | RCT | OA, CLA |
| Kehagias I et al., [10] | 2008 | Greece | 293 | Non-RCT, prospective | OA, CLA |
| Fukami Y., [11] | 2007 | Japan | 73 | Retrospective | OA, CLA |
| Katkhouda N et al., [12] | 2005 | USA | 247 | RCT, double blinded | OA, CLA |
| De U et al., [13] | 2005 | India | 278 | Non-RCT, prospective | OA, CLA |
Most of the studies have involved patients with similar age groups (25-35 years) and BMI (20-26). However, gender distribution was much broad (female/male ratio 0.7-1.5).
Time taken to perform SPLA was 26 minutes more than OA and CLA in our study. However, difference in duration between CLA and OA was negligible. We finished one SPLA within 30 minutes and two cases took less than an hour. Difference in mean duration of surgery in treatment arms in patients with BMI<25 was significant but not in patients with BMI ≥25. Patients were also compared in a similar setting in reference to duration of pain [<3 days versus ≥3 days] and we noted that CLA took significantly less time compared to OA and SPLA in patients who presented with a shorter duration of pain. Literature is extremely diverse when it comes to time taken to finish surgery. The relatively old studies show difference between OA and CLA is more than what we see today and reflects gain of skill in doing laparoscopic procedures. The same is true for SPLA as most studies show significant difference between SPLA and other two procedures and insignificant difference between OA and CLA. A longer time taken in performing SPLA might be attributed to use of existing laparoscopic instruments, actually not designed for and therefore, surgeons faced a greater difficulty and consequently a longer operating time [Table/Fig-8].
Duration of surgery, length of hospital stay and return to usual activity/job.
| Duration of Surgery[Minutes] | Hospital Stay [Days] | Return to Job [Days] |
|---|
| Author | Open | CLA | SPLA | Open | CLA | SPLA | Open | CLA | SPLA |
|---|
| Present | 56.93 | 57.00 | 82.79 | 5.27 | 2.40 | 3.36 | 19.73 | 13.20 | 13.00 |
| Minutolo [2] | 49.3 | 52.2 | - | 3.87 | 2.75 | - | OA>LA | - |
| Sateesh [3] | - | 34.2 | 39.0 | - | 2.08 | 1.8 | - | NA | NA |
| Baik [5] | - | 71.7 | 71.6 | - | 4.5 | 4.3 | - | NA | NA |
| Frutos [4] | - | 32.12 | 38.13 | - | 0.78# | 0.88# | - | NA | NA |
| Liang [6] | - | 50 | 60 | - | 2.29 | 3 | - | NA | NA |
| Kang [7] | - | 61.7 | 65.88 | - | 3.05 | 2.89 | - | NA | NA |
| Li [14] | 12.35* [OA<CLA] | - | 0.60*[CLA < OA] | - | 4.52* [OA>CLA] | - |
| Kehagias [10] | 47 | 44.3 | - | 3.1 | 2.2 | - | NA | NA | - |
| Katkhouda [12] | 60 | 80 | - | 3 | 2 | - | No Difference | - |
| De [13] | 25+ | 30+ | - | 5+ | 3+ | - | 14+ | 3+ | - |
| Ignacio [15] | NA | NA | - | OA>CLA | 0.9# | - | 11 [OA=CLA] | - |
*Difference in duration; +Median, all other are mean, #Originally in hours, converted to days for comparison, Underlined values are significant.
Most studies have not compared treatment groups with respect to BMI, duration of pain, presence of adhesions, initially visualized organ, and location of appendix. So, a comparative analysis of the present study with other studies could not be done.
Patients who underwent minimal invasive procedures in our study complained of more pain in immediate postoperative period (till 4th hour) compared to those who underwent OA. A reversal in pattern of pain from 4th hour onwards and persistence of statistically significant pain in patients in OA arm was noted at 12th and 24th hour following surgery. A detailed comparison of postoperative pain perception in various studies has been shown in [Table/Fig-9].
| Author | Postoperative pain |
|---|
| Early POP | Late POP |
|---|
| Finding | p | Finding | P |
|---|
| This Study | MIS>OA | <0.001 | OA>MIS* | <0.001 |
| Goudhar [9] | OA=CLA | -- | OA>CLA | 0.0123 |
| Kaplan [19] | OA>CLA, <0.05 |
| Kehagias [10] | OA=CLA, p=0.93 [p=0.82**] |
| Golub [16] | OA>CLA |
| Baik [5] | SPLA>CLA | 0.048 | SPLA=CLA | -- |
| Park [17] | SPLA>CLA | - |
*Includes both CLA and SPLA, **Degree of pain remission.
Pain in immediate postoperative period in laparoscopy may be explained by persistence of hypercarbia which may take some time to fully wash off from peritoneal cavity. Persistence of capnoperitoneum is a well-known entity that can cause irritation of nerve endings, operating site pain as well as referred pain elsewhere like shoulder pain [18]. We found most of the patients tolerated mild to moderate pain well up to score of 5 to 6. All the patients were offered analgesics on demand in addition to, regularly advised analgesia. Analgesia requirement was in coherence with VASS with a higher demand reflecting an increasing VASS, followed by a subsequent decline. Requirement for additional analgesics was more for patients in CLA and SPLA than OA in early postoperative period. Requirement reversed and then persisted in favor of patients in OA arm, who demanded more analgesics after 4 hours. Kaplan, Kehagias and Baik didn’t find any difference in total analgesic requirement in their respective study groups [5,10,19]. In contrast, Goudhar found requirement was more in OA arm (1.5+/-0.5, 2.5+/-0.5, p=0.3239) [9].
Incidence of PONV remained low in our study (Only 2 patients in OA, none in CLA and SPLA). Frutoshas mentioned occurrence of vomiting in one patient [1.07%] in CLA [4]. Most studies have not considered vital parameters worth comparing. Resumption of oral feeds following any GI-surgery is a major milestone in recovering from surgery as well as anaesthesia. Nearly 75% patients were allowed orally after six hours, remaining were kept NPO and allowed orally next morning. Mean time difference was not significant, however, studies elsewhere showed a striking difference in duration before resumption of oral feed [Table/Fig-10].
Resumption of Oral Feeding.
| Author | Open | CLA | SPLA |
|---|
| This Study | 6.27 (BS) | 4.80 (BS) | 3.86 (BS) |
| Minutolo [2] | 33.6 (OF) | 28.4 (OF) | N/A |
| Baik [5] | N/A | 30.6 (OF) | 28.4 (OF) |
| Liang [6] | N/A | 22 (OF) | 12 (OF) |
| Li X et al., [14] | 8 OA > CLA (OF) | N/A |
| Katkhouda [12] | 24 (OF) | 23.5 (OF) | N/A |
| De [13] | 72 (OF) | 24 (OF) | N/A |
| BS=Bowl Sound, OF=Oral Feeding |
Wound infection occurred in <10% of patients in our study. Incidence was more in OA than in CLA and SPLA but was insignificant. High incidence of wound infection in open surgeries compared to minimal invasive group has been supported by many studies [Table/Fig-11]. Increased wound infection in OA may be due to removal of inflamed appendix directly through the wound, whereas in LA it is extracted via a bag or trocar. In addition, port-sites in LA are smaller compared to larger wounds of OA, especially in obese patients. This result is consistent with the data shown in a recent meta-analysis, which reported a lower rate of postoperative complications, especially surgical wound infection rate, after LA [14]. Infection of the surgical wound worsens the quality of life in early postoperative period and prolongs recovery time. An advantage of LA is to reduce the wound infection rate. Mean hospital stay in our study was significantly less in CLA and SPLA than in OA [difference of >2 days] and this was similar to the findings of other reported series [Table/Fig-8]. Discrepancies in various studies may be due to social standards, insurance system and health care policies. Even in our study a relatively longer duration of hospital stay can be attributed to hilly terrain and also to the fact that most of the patients were from remote places where optimum postoperative health care facilities are still unavailable.
| Author | Open (%) | CLA (%) | SPLA (%) |
|---|
| This Study | 9.1 | 6.6 | 7.14 |
| Minutolo [2] | 5.49 | 0 | - |
| Sateesh [3] | - | 8 | 12 |
| Liang [6] | - | 15.7 | 7.1 |
| Baik [5] | - | 0 | 3.9 |
| Kang [7] | - | 8.5 | 5.3 |
| Li [14] | 8.4 | 3.8 | - |
| Kehagias [10] | 12.8 | 5.3 | - |
| De [13] | 14 | 4 | - |
| Katkhouda [12] | 39.1 | 33.3 | - |
Return to activity following appendectomy is the subject of intense debate. A minimally invasive operation by definition should allow for a quicker recovery, shorter convalescence at home, and quicker return to work. Similar results were shown by Li and De [13,14]. In contrast, Ignacio didn’t find difference in time to return to work [15] [Table/Fig-8]. Though, we found minimal difference in resumption of normal activity following CLA and SPLA, difference between OA and minimum invasive procedures was significantly more [>6 days]. These findings are supported by St Peter and a meta-analysis by Zhou [20,21]. The meta-analysis concluded days to normal activity were significantly shorter in the SILA/SPLA than in the CLA (weighted mean difference=–0.58, 95% CI=–1.02 to –0.14, p=0.01).
CLA has been demonstrated to have advantages in certain situations such as improved cosmetic outcome. Our study showed significantly better cosmetic results in CLA than OA. Similar results were shown by Pedersen (p<0.001), De and Goudhar [9,13,22]. SPLA too showed significantly better cosmetic results than CLA. Baik and Frutos mentioned SPLA has an advantage over CLA in terms of cosmetic concerns [4,5]. Liang mentioned lower abdominal and suprapubic surgical wounds were seen more obviously in patients who underwent CLA, whereas SPLA incision scar was well hidden in the skin folds of the navel [6]. Sateesh mentioned good scar healing in SPLA, which shows better cosmetic appearance than CLA group [3].
Our analysis showed no statistical significant difference in terms of total cost of treatment between OA and CLA. Similar findings were shown by Mintulo without any statistically significant difference (p=0.812) [2]. In a meta-analysis of 8 RCT’S, Wei compared LA and OA on the basis of the cost across different countries using the hospital cost ratio and found the difference insignificant between the cost of OA and LA [23]. However, these data are in contrast with those recently published by McGrath who compared the costs between LA and OA in 2,887,823 patients undergoing surgery in the period between 1998 and 2008 [24]. Similarly the cost of treatment was higher in LA in many studies and can be attributed to the use of disposable laparoscopic instruments and the longer operative time [10,25,26]. In our study, mainly by employing reusable laparoscopic instruments, we were able to minimize the operative costs. The cost of the treatment (Rupees) was 23049 in SPLA, and 14,150 in CLA (p= 0.132). Baik showed mean cost of treatment is marginally higher in CLA as compared to SPLA [5]. In contrast Lee showed the cost was significantly lower in TULA/SPLA group; this is because the instrument was made using slim pipes and trocar [27]. Differing time under anaesthesia due to different operative time also can be one of the causes for this lack of difference in cost.
We couldn’t find a significant difference in overall satisfaction of patients in the three treatment groups. Sateesh found the patient satisfactory score for CLA to be in between 6-10, with mean value of 8.04, whereas for SPLA it was in between 8-10 with mean valve of 9.08 (p≤0.001) [3].
Limitation
We took cases of only uncomplicated appendicitis and therefore, the actual results may be different especially regarding conversion, duration of surgery, scar acceptability and hospital stay. The results may be applicable to patients in urban area where patients present early without complications but definitely not in rural area where waiting till eleventh hour still an unavoidable rule.
Conclusion
For lean and thin persons with BMI <25, OA is an overall better option, CLA is good for overweight and obese. All three procedures are safe. Conversion is usually not required if it’s a simple appendicitis. Though immediate pain is comparable, patient do complain of prolonged postoperative pain in OA. Patients are usually satisfied in terms of scar as well as overall care, irrespective of treatment modality offered. Cost effectiveness might be an issue especially in developed countries where a large population still can’t afford their basic daily requirements and not yet covered by health insurance.
*Within the study group;
**Patients below 12 years and above 50 years have not been shown.
ABoth female patients, with Pfannenstiel scar; BChances of appendix visualization less with longer pain history [p<0.001], no impact by Gender [p=0.263] and BMI [p=0.932]; CPatients with BMI<25 [p=0.039] and pain ≥3 days [p=0.017] developed adhesions more commonly; DNo adhesions with sigmoid colon and right ovary, so excluded from final analysis; EPresence versus absence of adhesions; FMore common with pain of ≥3 days [p=0.001]; GNo impact on duration of pain [p=0.807]; Common in femalesH and malesI; J Both complications in same patient.
*Difference in duration; +Median, all other are mean, #Originally in hours, converted to days for comparison, Underlined values are significant.
*Includes both CLA and SPLA, **Degree of pain remission.