Additional Virtual Reality Sitting Balance Training Using XBox Kinect™ in Patients with Neurological Disorders: A Pilot Study
Xina Henry Quadros1, Sanjana Rao2, Senthil Kumaran Dharmaraj3
1 Physiotherapist, Department of Physical Medicine and Rehabilitation, Kokilaben Dhirubhai Ambani Hospital and Medical Research Institute, Mumbai, Maharashtra, India.
2 Physiotherapist, Department of Neurology, Justice K.S.Hegde Charitable Hospital, Mangalore, Karnataka, India.
3 Associate Professor, Department of Physiotherapy, School of Allied Health Sciences, Manipal University, Manipal, Udupi, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Senthil Kumaran Dharmaraj, Associate Professor, Department of Physiotherapy, School of Allied Health Sciences, Manipal University, Manipal-576104, Udupi, Karnataka, India.
E-mail: senthil.kumaran@manipal.edu
Introduction
Sitting balance is a prerequisite to upper extremity function, standing and walking, which is affected in various neurological diseases. It is important to attain a good level of sitting balance before one can proceed to standing. In recent years, virtual reality game training has gained a widespread application.
Aim
This pilot study aimed to examine the role of additional virtual reality sitting balance training using a commercial interactive virtual reality system- Xbox Kinect™ in patients with neurological disorders.
Materials and Methods
Four patients with sitting balance impairments following neurological disorders received two weeks of virtual reality based therapy along with the conventional physiotherapy. Sitting balance was evaluated using FIST (Function In Sitting Test) scores at baseline, one week and after two weeks of intervention.
Results
All four patients showed clinically significant improvement in FIST score between the pre and post intervention. Percentage of improvement in FIST score was approximately 27% with a minimum change of 10 points in the FIST score Minimal Clinically Important Difference (MCID=6.5).
Conclusion
Additional virtual reality training may improve sitting balance control in neurological patients with balance impairments. It can be used as an adjunct in routine neurorehabilitation.
Dynamic sitting, Gaming therapy, Neurorehabilitation
Introduction
Sitting balance is an important prerequisite to standing balance and predictor of the safe performance of many functional activities [1]. Sitting balance training involves various approaches and techniques, mainly conventional methods of training sitting balance like weight shifts, peg board activities, reaching, perturbations, rotations, inflatable disc or therapy ball, etc., [2]. In recent times, intervention techniques such as neurodevelopmental treatment, task oriented training and progressive resistive training have been implemented to improve balancing ability [3].
However, traditional balance training methods rely on the repetition of specific movements, which many patients presume to be monotonous, resulting in boredom furthermore leading to reduced motivation and compliance with training sessions [4]. Therefore, new and promising methods of applying biofeedback such as virtual reality are being considered in therapy.
Virtual Reality training involves innovative and interactive computer generated simulation that provides a virtual environment and makes the participant think that imaginary objects and incidents are real [5]. Virtual rehabilitation approaches to sitting balance have been used for enhancing recovery in function that may lead to decrease in risk of falling [6].
Xbox Kinect™ is a video gaming system that perceives the user’s movement via infrared camera sensors. Unlike other commercial gaming systems, with Xbox Kinect™, the users can view the virtual environment without the need for a special controller and their movement is captured in real time where immediate feedback is provided [7].
In rehabilitation, it is important to attain a good level of sitting balance before one can proceed to standing. Hence, we aimed at examining the role of virtual reality sitting balance training using Xbox Kinect™ in patients with neurological disorders.
Materials and Methods
This pilot case series was reviewed by Institutional research committee and Institutional ethics committee. Total duration of the study was six months (August 2012-January 2013) during which 16 patients with neurological disorders were screened from a tertiary care hospital. Out of these, 12 patients were excluded for the following reasons: cognitive impairment (two), Full Function In Sitting Test (FIST) score at baseline (four), visual impairment (one), medical conditions affecting testing and treatment (three), age > 65 years (two). The remaining four patients aged between 18 and 65 years, either gender and those who had the ability to sit with or without supervision but with impaired or affected sitting balance were included in the study and an informed consent was obtained.
Baseline assessment including demographic details and sitting balance using FIST was done. FIST is a clinical, performance-based test for assessing sitting balance. Patients were asked to perform 14 basic, everyday activities in a seated position with an examiner scoring their performance using a 0-4 point ordinal scale [8]. A clinically meaningful change is indicated by an increase in score of ≥6.5 points [9].
For the study, the FIST was administered with the patient seated in bed/chair with half of femur length supported by mattress while sitting and hip-knee flexed to 90°, with feet on the floor, thighs in neutral, hands on lap (unless needed for balance support). The examiner was beside the patient to ensure patient safety and to assist as needed for scoring purposes at all time [8]. The total FIST score was calculated.
Following baseline assessment, intervention was given to all participants in the form of routine conventional physiotherapy (which included individualized protocols as per the therapist’s and patient’s goals) along with additional 30 minutes a day, 6 sessions per week for 2 weeks of virtual reality gaming using Xbox Kinect™ was given. The games used for virtual reality based intervention were Rally ball and Joy ride Kinect. Post intervention assessment using FIST score at one week and at two weeks was done. Patient experiences in the form of an informal interview were taken along with FIST score.
Results
The demographic details of the four patients are shown in [Table/Fig-1] which depicts variations in chronicity and characteristics of patients. The pre and post intervention one week and two weeks FIST scores have been shown in [Table/Fig-2] respectively. Following two weeks of virtual reality rehabilitation program, an average of 27% improvement was seen in all patients with a minimum change of at least 10 points in FIST score.
Demographic details of the patients (n=4).
| Demographics | Patient 1 | Patient 2 | Patient 3 | Patient 4 |
|---|
| Gender | Male | Male | Male | Male |
| Age (in yrs) | 54 | 57 | 60 | 20 |
| Occupation | Photographer | Bank Manager | Farmer | Student |
| Hand dominance | Right | Right | Right | Right |
| Diagnosis | Traumatic Brain Injury | Right MCA infarct-Hemorrhagic stroke | Recovered Old MCA infarct stroke (2003), recurrent progressive lacunar stroke (2012) | Traumatic Brain injury |
| Duration of Diagnosis | 6 months | 1 month | 5 days | 1½ years |
Change in FIST score during the study (n=4).
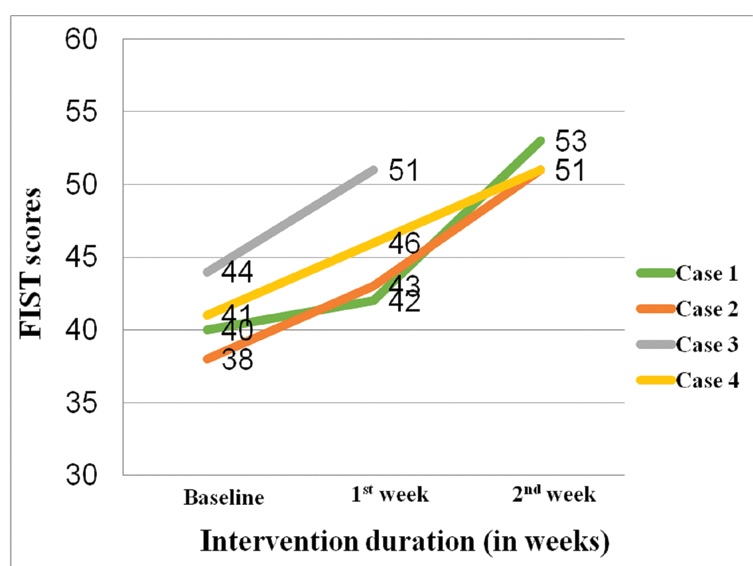
In this study, out of four patients, three patients completed two weeks of therapy sessions. One patient (Case 3) was able to complete only 1week of therapy due to early discharge. However, an improvement of 7 points (16%) in FIST scores was observed even in that patient. All the patients found this form of therapy to be a “fun filled and enjoyable” experience.
Discussion
This pilot study was done to examine the effect of a commercial and innovative Xbox Kinect™ virtual reality gaming system on sitting balance in neurological rehabilitation. All four patients had a heterogeneous diagnosis (CVA-2, TBI-2) with varying chronicity. To measure changes in sitting balance; FIST was used as the clinical tool.
Following two weeks of virtual reality rehabilitation program, clinically significant improvement in FIST score on sitting balance was observed in these patients. Percentage of improvement in FIST score was approximately 27% with a minimum change of 10 points in the FIST score. This is a clinically meaningful and significant difference.
Although Case 3 completed only one week of therapy, improvement of 7 points (16%) in FIST scores was recorded. Hence, it could be cautiously concluded that even with one week of intervention, virtual reality gaming therapy could show promising results on sitting balance.
This clinical improvement could be attributed to the fact that the interactive virtual reality gaming provided both, patient and therapist, with immediate feedback about performance, goal achievement and successful progression from simple to complex tasks. It was observed through the informal interviews that the patients found the therapy to be a motivating, fun and enjoyable experience.
Similar study was done by Betkar AL et al., with the video gaming without the avatar in which the effect of game based exercises on dynamic short sitting balance in people with chronic spinal cord and Traumatic Brain Injuries was examined [10]. Centre of Pressure (COP) controlled video game based tool with the Force-Sensitive Applications (FSA) software and pressure mat was used for training in the study. No conventional therapy was given during the treatment period. The quantitative measurements were obtained through a questionnaire that was administered after the exercises and dynamic balance improvements were measured using Clinical Test of Sensory Interaction and Balance as the clinical tool. They found that video gaming improves the dynamic balance control and motivates the participants along with being a fun filled exercise in the study. This conclusion is in line with our study demonstrates the effect of additional virtual reality training on sitting balance.
Limitation
The limitation of the study was that the (a) sample size was small; (b) the study was conducted over a patient population of varying diagnosis; (c) we cannot completely rule out chances of spontaneous recovery in two patients and (d) patient’s experiences with any form of measure or scale could not be quantified. Future study can be conducted as a randomized control trial using a large sample of homogenous patient population. A scale or a measure to quantify the patient’s experience can be considered.
Conclusion
Additional virtual reality based gaming using Xbox Kinect™ improves sitting balance control in neurological patients with balance impairments. It can be used as an adjunct in routine neurorehabilitation.
[1]. Bohannon RW, Smith MB, Larkin PA, Relationship between independent sitting balance and side of hemiparesisPhys Ther 1986 66(6):944-45. [Google Scholar]
[2]. Leroux A, Pinet H, Nadeau S, Task-oriented intervention in chronic stroke: changes in clinical and laboratory measures of balance and mobilityAm J Phys Med Rehabil 2006 85(10):820-30. [Google Scholar]
[3]. O’Sullivan S, Assessment of motor functionIn Physical Rehabilitation: Assessment and Treatment (4th ed.), O’Sullivan S, Schmitz TJ, Eds 2000 PhiladelphiaFA Davis [Google Scholar]
[4]. Gil-Gómez JA, Lloréns R, Alcañiz M, Colomer C, Effectiveness of a Wii balance board-based system (eBaViR) for balance rehabilitation: A pilot randomized clinical trial in patients with acquired brain injuryJ Neuroeng Rehabil 2011 23(8):30 [Google Scholar]
[5]. Weiss PL, Katz N, The potential of virtual reality for rehabilitationJ Rehabil Res Dev 2004 41(5):vii-x. [Google Scholar]
[6]. Cho KH, Lee KJ, Song CH, Virtual-reality balance training with a video-game system improves dynamic balance in chronic stroke patientsTohoku J Exp Med 2012 228(1):69-74. [Google Scholar]
[7]. Sin HH, Lee GC, Additional virtual reality training using Xbox Kinect in stroke survivors with hemiplegiaAm J Phys Med Rehabil 2013 92(10):871-80. [Google Scholar]
[8]. Gorman SL, Radtka S, Melnick ME, Abrams GM, Byl NN, Development and validation of the function in sitting test in adults with acute strokeJ Neurol Phys Ther 2010 34(3):150-60. [Google Scholar]
[9]. Gorman SL, Harro CC, Platko C, Greenwald C, Examining the function in sitting test for validity, responsiveness, and minimal clinically important difference in inpatient rehabilitationArchives of Physical Medicine and Rehabilitation 2014 95(12):2304-11. [Google Scholar]
[10]. Betker AL, Desai A, Nett C, Kapadia N, Szturm T, Game-based exercises for dynamic short-sitting balance rehabilitation of people with chronic spinal cord and traumatic brain injuriesPhys Ther 2007 87(10):1389-98. [Google Scholar]