Introduction
More than half of the infants are started on complementary feed before six months. Perception of Inadequate Milk supply (PIM) remains one of the most frequent causes of early institution of complementary feeding. Perception of Inadequate Weight Gain (PIWG), may also influence a mother’s decision to start early complementary feeding which may be a consequence of PIM.
Aim
To find the proportion of early complementary feeding and to compare predictive models in identifying mothers who are more likely to initiate early complementary feeds.
Materials and Methods
A descriptive epidemiological study with cross-sectional design was carried out for three months between May-July 2013 among 99 mother-child dyads, with children in the 6-24 months age group, residing in Matigara block of West Bengal. Data were collected regarding infant feeding practices and prevalence of early complementary feeding was calculated. Logistic regression was done using SPSS Version 20.0 with the predictor variables classified under three constructs of socio-demography, health system related factors and mothers perceptions; and models were constructed using one, two or all three constructs.
Results
The proportion of early complementary feeding was 30.3%. In univariate analysis, none of the variables were found to be statistically significant. However, on multivariate analysis, Model (with all variables) was found to be statistically significant. The best Area Under Curve (AUC) was found with the inclusion of the socio-demography, health system related factors and mothers’ perception.
Conclusion
The perception of the mother regarding adequacy of her milk production and regarding the child’s weight gain are the most important predictors of early initiation of complementary feeding. All counselling activities for the mother should therefore be designed in a way as to address these issues.
Introduction
More than half of the infants are started on complementary feed before the WHO recommended age. Lack of knowledge among the mothers is often cited as the main reason for the same [1]. However, early complementary feeding has been seen to be prevalent even among women who were aware of the WHO recommended time of initiation [1-4]. Several determinants have been found to influence a mother’s decision to start early complementary feeding. The sex of the child, maternal age, wealth and marital status of the mother and maternal and paternal education are a few of the socioeconomic factors that influence decisions regarding complementary feeding in mothers from Asia and Africa [2,5-11]. In the United States, studies have shown that low income African-American mothers had weaned children already during the first month of life with cereal in the bottle [12]. Other factors that have been shown to influence the timing of initiation of complementary feeding are Antenatal Care (ANC) follow up, postnatal care, and institutional delivery [5-9,11]. Employed mothers and home delivered mothers have been shown to have a higher risk of early initiation of complementary feeding [13].
Inadequate milk production, low enough to cause inadequate weight gain in infants is seen in less than 5% of mothers [14,15]. On the other hand, the PIM, remains one of the most common problems and the most frequent cause of cessation of breast milk feeding and early institution of complementary feeding [16,17]. About 23% to 56% of women who had weaned their children before the recommended duration cited PIM as the cause for the same [18,19]. PIM makes the mother more likely to stop breast feeding regardless of the age of the child [20,21]. Perception of Inadequate Weight Gain (PIWG) in infants during the early months, may also influences a mother’s decision to start early complementary feeding, either as a consequence of PIM or in the absence of it [22,23].
Despite the fact that a programmed effort to promote exclusive breast feeding till the age of six months is underway in the country, latest data (NFHS 4) show that only 52.3% of children under age six months are exclusively breastfed in West Bengal [24]. Identification of the reasons for this in the remaining half of children would be useful to health professionals to address the issues leading to early complementary feeding and to health officials attempting to device targeted interventions during health planning.
In this context, the present study attempts to find out the proportion of mothers that have started complementary feeding before the recommended period of six months and to compare predictive models to help identify mothers more likely to initiate early complementary feeds in their children.
Materials and Methods
Study Design and the Participants
A descriptive epidemiological study with cross sectional designwas conducted during May-July 2013. Participants were mother-child dyads with children aged 6-24 months, residing in Matigara block of Darjeeling district, West Bengal, India. Exclusion criteria involved mothers who refused to give consent and children who were very ill.
Data Collection
All the Panchayat Headquarter sub-centres under Matigara block were visited and all mother-child dyads with children aged 6-24 months were recruited. Data were collected using a predesigned and pretested schedule administered to the mothers.
Questionnaire
The semi-structured questionnaire consisted of three sections:
Section I: included questions on socio-demographic variables (age of child, sex of the child, religion, caste, literacy of care giver, per capita income of family, birth weight of the child).
Section II: included questions on health system delivery related variables (place where the child was delivered, whether services were received before or after the initiation of IMNCI, post natal visits done by the health worker and pre-lacteal feed given to child).
Section III: included variables recording the perception of the mother regarding the adequacy of breast milk and adequate weight gain in the children.
The questionnaire was customised for the study with the help of Integrated Management of Neonatal and Chilhood Illnesses (IMNCI) checklists [Appendix1] and data were collected by the investigators. Translation, back-translation, and re-translation of the prepared questionnaire was done with the help of language experts, followed by pre-testing among a convenience sample of 30 children attending the Immunization OPD of North Bengal Medical College and Hospital.
Sample Size Calculations
The proportion of children age 6-8 months receiving solid or semi-solid food and breast milk in West Bengal as reported in the National Family and Health Survey-4 (i.e., 52%), 24 was used for calculating the sample size. Sample size was computed by using the formula:
N = Z2(1-α/2)p (1-p)/ d2Where, p: Expected proportion, d: Absolute precision, 1- α/2: Desired Confidence level. Considering a 10% absolute precision (L), the final sample size comes out to be 96.
Outcome Variables
‘Early initiation of complementary feeding’ was the dichotomous outcome variable recorded as ‘yes’ or ‘no’. Prevalence was calculated by dividing the number of children started on complementary feeding before six months by total number of children 6-24 months, included in the sample.
Exploratory Variables
The exploratory variables were classified under three constructs of socio-demography, health system related factors and mothers perceptions.
Ethical Committee Approval
The Institutional Ethics Committee of the North Bengal Medical College, Sushrutanagar, Darjeeling reviewed and cleared the proposal for the present study.
Data Analysis
Data were collected in predesigned and pretested questionnaires and handled with strict confidentiality. Data were entered into Excel (Microsoft Inc) and all calculations were done using IBM Statistical Package for the Social Sciences (SPSS) (Version 20.0, IBM).
Statistical Analysis
Data was analysed using principles of descriptive and analytical statistics. Univariate logistic regression was done to assess the unadjusted odds of the event. Multivariate logistic regression was carried out with all the variables irrespective of their significance on univariate results. Three models were constructed using one, two or all three constructs. Model 1 uses the socio-demographic constructs/ characteristics of mothers to predict early initiation of complementary feeding among the children. In model 2, both socio-demographic and health service related variables have been used to model the prediction. Model 3 uses the variables related to the perception of the mother regarding adequacy of feeding and weight gain in the infant in addition to the variables in model 2. The Hosmer Leme show goodness of fit of the respective models along with the Cox & Snell and Nagelkerke R Square were also calculated.
Results
Prevalence of Early Complementary Feeding
Among the 106 mother-child dyads, 99 (93.4%) finally participated in the study. Among them, the numbers of mother who weaned their child off breast milk before the recommended period of six months was 30 (30.3%).
Socio-demographic, Health Services Related and Variables Recording Mothers’ Perception
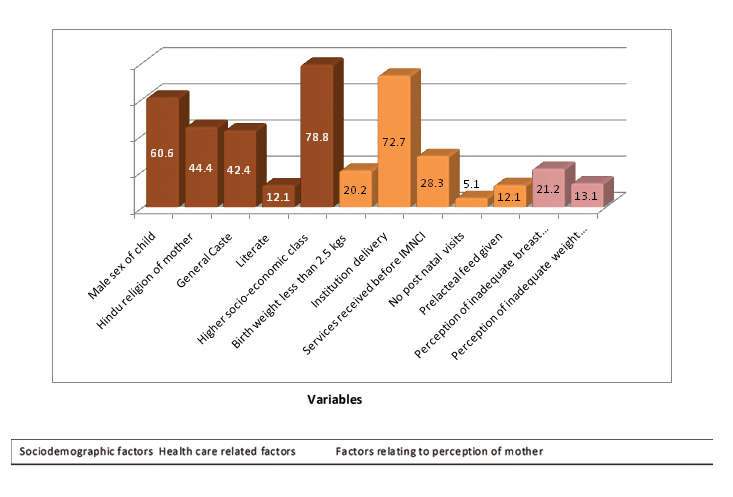
The proportion of mothers with a male child, of Hindu religion, general caste, with no formal literacy, lower socioeconomic condition was 60.6%, 44.4%, 42.4%, 87.9% and 21.2%respectively. Higher proportion of mothers were illiterate (87.9%) but belonged to a higher socio-economic class (78.8%). Low birth weight (<2.5Kg) was seen in only one-fifth of the children (20.2%). Post natal visits were done in 94.9% cases, which was higher than 72.7% of deliveries that were conducted at health institutions. Prelacteal feeds were given 12.1% of the children. Approximately a fifth (21.2%) of the mothers perceived that their milk production was not enough for the child while 13.1% of the mothers thought that the child was not gaining weight despite regular feeding [Table/Fig-1].
Distribution of risk factors associated with early complimentary feeding. n=99.
Factors Associated with Timely Initiation of Complementary Feeding
Univariate analysis:
[Table/Fig-2] shows that early complementary feeding was more common if the child was male and other than Hindu or general caste. It was also more likely in caregivers with no formal literacy and with a higher SE class. Early initiation was more common if the child was less than 2.5 kg at birth or had been delivered at home. However, none of these differences were statistically significant. There was a significantly increased odd of the child being started on early complementary feeding if prelacteal feeds were given to the child or there were PIM and inadequate weight gain in the infant by the caregiver.
Variables used in the study and univariate analysis of early complimentary feeding.
| Variables | Frequency of variables | Proportion of early complimentary feeding | COR (Confidence Interval) |
|---|
| Sex of the child | Female^ | 39 | 9 (23.1%) | 1.795 (0.719 – 4.479) |
| Male | 60 | 21 (35.0%) |
| Religion | Others ^ | 55 | 20 (36.4%) | 0.515 (0.211- 1.258) |
| Hindu | 44 | 10 (22.7%) |
| Caste | Others ^ | 57 | 20 (35.1%) | 0.578 (0.236, 1.414) |
| General | 42 | 10 (23.8%) |
| Literacy of care giver | No formal literacy ^ | 87 | 28 (32.2%) | 0.421 (0.087, 2.053) |
| Literate | 12 | 2 (16.7%) |
| Per capita income of family | Lower SE class [Per capita income <Rs. 2000] ^ | 21 | 6 (28.6%) | 1.111 (0.384. 3.213) |
| Higher SE class [Per capita income ≥ Rs. 2000] | 78 | 24 (30.8%) |
| Birth weight of the child | 2.5 kgs or more^ | 79 | 15 (19.0%) | 3.109 (1.090, 8.872)* |
| <2.5 kgs | 20 | 9 (45.0%) |
| Place where the child was delivered | Home^ | 27 | 9 (33.3%) | 0.824 (0.319, 2.125) |
| Institution | 72 | 21 (29.2%) |
| Services received in relation to IMNCI | After IMNCI^ | 71 | 23 (32.4%) | 0.696 (0.259, 1.871) |
| Before IMNCI | 28 | 7 (25.0%) |
| Post natal visits done by the health worker | PNC visit done^ | 94 | 27 (28.7%) | 3.722 (0.589, 23.534) |
| PNC visit not done | 5 | 3 (60.0%) |
| Pre-lacteal feed given to child | No^ | 87 | 23 (26.4%) | 3.896 (1.124, 13.497)* |
| Yes | 12 | 7 (58.3%) |
| Perception of inadequate milk production (PIM) | No^ | 78 | 16 (20.5%) | 7.750 (2.683, 22.386)* |
| Yes | 21 | 14 (66.7%) |
| Perception of inadequate weight gain (PIWG) | No^ | 86 | 22 (25.6%) | 4.655 (1.377, 15.732)* |
| Yes | 13 | 8 (61.5%) |
| Total population | 99 | 30 (30.3%) | |
N=99
^ denotes referent category, * denotes p<0.05.
Multivariate analysis:
[Table/Fig-3,4] show three predictive models for predicting early initiation of breast feeding that were developed for the present study. Model 1 includes only the socioeconomic variables, Model 2 includes the socioeconomic and health system related variable and Model 3 includes the perception of the mother regarding inadequate breast milk secretion and inadequate weight gain of the child in addition to the variables in model 2.
Multivariate models of early initiation of complimentary feeding.
| Variables | Model 1 | Model 2 | Model 3 |
|---|
| Intercept | -0.628 | -2.643 | -4.577 |
| Socio-demographic variables | Sex(1) | 2.08 (0.77, 5.61) | 1.12 (0.35,3.66) | 2.38 (0.49, 11.48) |
| Religion_coded (1) | 0.47 (0.17, 1.26) | 0.69 (0.19,2.53) | 0.70 (0.15, 3.38) |
| Caste_coded (1) | 0.41 (0.15, 1.10) | 0.54 (0.17, 1.73) | 0.28 (0.06, 1.30) |
| Caregiver_literacy (1) | 0.52 (0.10, 2.72) | 0.38 (0.06, 2.26) | 0.21 (0.02, 1.95) |
| PCI_regrouped (1) | 1.09 (0.36, 3.35) | 1.77 (0.46,6.82) | 4.08 (0.64, 25.85) |
| Health Service related variables | Birthplace (1) | | 0.19 (0.03, 1.10) | 0.32 (0.04, 2.65) |
| Birth_weight (1) | | 0.38 (0.09, 1.55) | 0.23 (0.04, 1.41) |
| Service_before_IMNCI (1) | | 3.51 (0.84, 14.60) | 3.20 (0.58, 17.65) |
| Any_PC_visit (1) | | 0.16 (0.01, 4.68) | 0.12 (0.00, 5.55) |
| Prelacteal_feed (1) | | 0.16 (0.03, 0.84) | 0.31 (0.04, 2.46) |
| Variables relating to perception of mother | Perception_inadequate_milk (1) | | | 29.55 (5.25, 166.39)* |
| Perception_weight_gain (1) | | | 16.90 (2.67, 107.04)* |
Model statistics for the three predictive models.
| Omnibus Tests of Model Coefficients | Hosmer Lemeshow P | -2 Log likelihood | Nagelkerke pseudo R Square |
|---|
| Chi-square | Degrees of freedom | Signi-ficance |
|---|
| Model 1 | 7.827 | 5 | .166 | .499 | 113.628 | .108 |
| Model 2 | 16.481 | 10 | .087 | .409 | 89.129 | .240 |
| Model 3 | 41.033 | 12 | .000 | .398 | 64.576 | .527 |
ROC curves and AUC:
The present study utilises the Receiver Operating Characterstic (ROC) curve (AUC) to compare models to predict early complementary feeding. ROC curve is often used as a measure of quality of the classification models. It may be used to assess accuracy quantitatively or to compare accuracy between predictive models. The ideal model would be one with an AUC of 1 while an AUC of 0.5 corresponds to the flipping of a coin. The inclusion of the health system related factors improves (Model 2) over the model including only the socio-demographic variables (Model 1), while the addition of the mothers perception in Model 3 improves the AUC to 0.892 [Table/Fig-5].
The test result variable(s): Model 1, Model 2, Model 3 has at least one tie between the positive actual state group and the negative actual state group. Statistics may be biased.
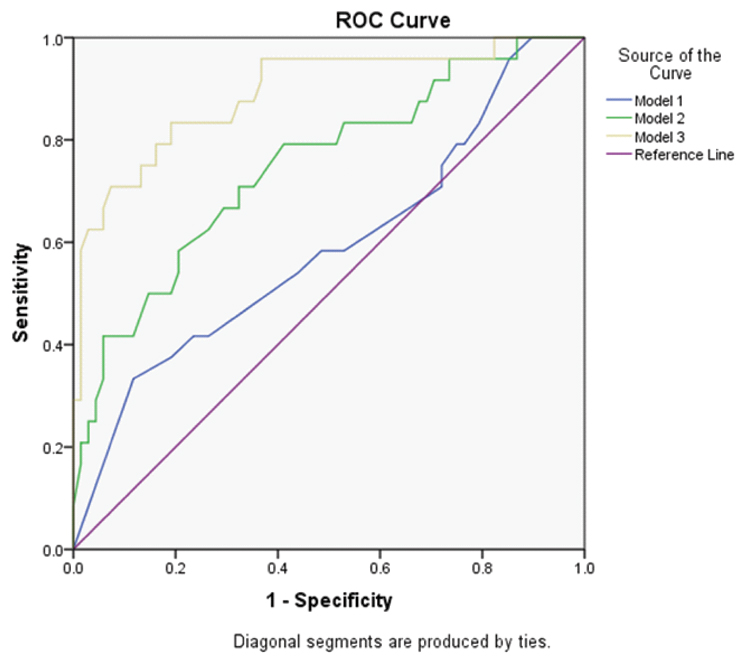 |
| Area Under the Curve |
| Test Result Variable(s) | Area |
| Model 1 | 0.591 |
| Model 2 | 0.748 |
| Model 3 | 0.892 |
Discussion
Early initiation of complementary feeding remains prevalent even in women having correct knowledge of the time of initiation of complementary feeding [8,25-28]. Despite aggressive campaigns advocating exclusive breast feeding for the first six months of life, there has not been a substantial increase in the duration of exclusive breast feeding in India. Data from the NFHS-2 in 1998-1999 to the NFHS-3 in 2005 -2006 has not shown any substantial increase (from 41.2% to 46.3%) [29]. In West Bengal, the proportion of children under six months that are exclusively breastfeed is 58.6% as per the NFHS-3 [29]. Even among other developed and developing countries the early initiation of complementary feeding remains common [30,31].
Several factors have been identified from studies around the globe that consistently influence a mother’s decision to initiate early complementary feeding in their children. These predictors can be broadly classified into three groups, namely, socio-demographic variables, health system related variables and perceptions of the mother. Socio-economic status, birth order, place of delivery, maternal and paternal education, male sex of the child were found to be statistically significant in studies conducted in India [1,32,33]. A study by Aggarwal et al., showed maternal education and paternal education were significantly related to timing of complementary feeding [32]. Among the health system related variables, women who had a history of antenatal care visit during their youngest child pregnancy period, gave their birth at health institution and had post natal visit tended to initiate complementary feeding timely.
Perceived inadequacy of milk supply or PIM is the most commonly reported problem by breast feeding mothers from all over the world. In a large section of these women, this leads to an early initiation of complementary feeding in their children [28,34]. A study in Bangladesh has observed that the common perception of “insufficient milk” was the main reasons for early initiation of complementary feeding in rural as well as urban children [35]. The findings were similar to the study by Semahegn et al., where the reason for too early initiation of complementary feeding was also the perceived inadequate breast milk production in 30.6% of the mothers [36].
However, early weaning is not ubiquitous in mothers with PIM and has also been noted in women without PIM [37]. A systematic review by Gatti deduced that apart from the maternal perception of insufficient milk supply, other cited reasons for early cessation of breastfeeding were infant satiety, previous experience, etc., [34]. The Infant and Young Children Feeding (IYCF) Guidelines of the government of India discuss the importance and management of mother with an actual decrease in milk supply (Mothers with Inadequate Milk), but does not discuss the issue of PIM, which is seen more frequently than an actual decrease in breast milk production [38]. Breastfeeding mothers have been observed to have concerns of inadequate weight gain in children either as a consequence of PIM or in the absence of it [34]. In the present study, PIWG has been noted as a significant predictor of early complementary feeding singly or after adjusting for other factors including PIM.
Limitation
The limitations of the study include inherent weakness of cross sectional studies to deduce a causal association. In addition, the study was undertaken in children of age group 6-24 months and data collected could be biased due to the inability to recall all details of the older children by mothers or caregivers.
Conclusion
The present study utilises three models that include the three groups of variables to try and identify predictors most likely to identify mothers who will initiate early complementary feeding in their children. Results of the study clearly depict that after adjustment for other factors it is the perception of the mother regarding adequacy of her milk production and her perception regarding the child’s weight gain were the most important predictors of early initiation of complementary feeding. All counselling activities for the mother should therefore be designed in a way as to address these issues.
[1]. Rao S, Swathi P, Unnikrishnan B, Hegde A, Study of complementary feeding practices among mothers of children aged six months to two years - A study from coastal south IndiaThe Australasian Medical Journal 2011 4(5):252-57. [Google Scholar]
[2]. Sisay W, Edris M, Tariku A, Determinants of timely initiation of complementary feeding among mothers with children aged 6–23 months in Lalibela District, Northeast Ethiopia, 2015BMC Public Health 2016 16(1):884 [Google Scholar]
[3]. Perez-Escamilla R, Lutter C, Segall AM, Rivera A, Exclusive breast-feeding duration is associated with attitudinal, socioeconomic and biocultural determinants in three Latin American countriesThe Journal of nutrition 1995 125(12):2972 [Google Scholar]
[4]. Tromp II, Briede S, Kiefte-de Jong JC, Renders CM, Jaddoe VW, Franco OH, Factors associated with the timing of introduction of complementary feeding: the Generation R StudyEuropean Journal of Clinical Nutrition 2013 67(6):625-30. [Google Scholar]
[5]. Saleh F, Ara F, Hoque MA, Alam MS, Complementary Feeding Practices among Mothers in Selected Slums of Dhaka City: A Descriptive StudyJournal of Health, Population, and Nutrition 2014 32(1):89-96. [Google Scholar]
[6]. Yemane S, Awoke T, Gebreslassie M, Timely initiation of complementary feeding practice and associated factors among mothers of children aged from 6 to 24 months in Axum town, north EthiopiaInternational Journal of Nutrition and Food Sciences 2014 3(5):438-42. [Google Scholar]
[7]. Agedew E, Demissie M, Misker D, Haftu D, Early Initiation of Complementary Feeding and associated factors among six months to two years young children, in Kambaworeda, south west Ethiopia: a community–based cross-sectional studyJournal of Nutrition & Food Sciences 2014 4(6):314 [Google Scholar]
[8]. Kimani-Murage EW, Madise NJ, Fotso J-C, Kyobutungi C, Mutua MK, Gitau TM, Patterns and determinants of breastfeeding and complementary feeding practices in urban informal settlements, Nairobi KenyaBMC Public Health 2011 11(1):1 [Google Scholar]
[9]. Mihrshahi S, Kabir I, Roy SK, Agho KE, Senarath U, Dibley MJ, South Asia Infant Feeding Research Network (SAIFRN)*. Determinants of infant and young child feeding practices in Bangladesh: secondary data analysis of Demographic and Health Survey 2004Food and Nutrition Bulletin 2010 31(2):295-313. [Google Scholar]
[10]. Senarath U, Agho KE, Akram DE, Godakandage SS, Hazir T, Jayawickrama H, Comparisons of complementary feeding indicators and associated factors in children aged 6–23 months across five South Asian countriesMaternal & Child Nutrition 2012 8(s1):89-106. [Google Scholar]
[11]. Khanal V, Sauer K, Zhao Y, Exclusive breastfeeding practices in relation to social and health determinants: a comparison of the 2006 and 2011 Nepal Demographic and Health SurveysBMC Public Health 2013 13(1):958 [Google Scholar]
[12]. Bentley M, Gavin L, Black MM, Teti L, Infant feeding practices of low-income, African-American, adolescent mothers: an ecological, multigenerational perspectiveSocial Science & Medicine 1999 49(8):1085-100. [Google Scholar]
[13]. Deme G, Bekele S, Argaw M, Berhane Y, Factors Associated with Early Initiation of Complementary Feeding in Bishoftu Town, Oromia, EthiopiaOpen Access Library Journal. 2015 2(e1949):1-9. [Google Scholar]
[14]. Neifert M, DeMarzo S, Seacat J, Young D, Leff M, Orleans M, The influence of breast surgery, breast appearance, and pregnancy induced breast changes on lactation sufficiency as measured by infant weight gainBirth 1990 17(1):31-38. [Google Scholar]
[15]. Butte NF, Garza C, Smith EO, Nichols BL, Human milk intake and growth in exclusively breast-fed infantsJ Pediatr 1984 104(2):187-95. [Google Scholar]
[16]. Colin WB, Scott JA, Breastfeeding: Reasons for starting, reasons for stopping and problems along the wayBreastfeeding Review 2002 10:13-19. [Google Scholar]
[17]. Cooke M, Sheehan A, Schmied V, A description of the relationship between breastfeeding experiences, breastfeeding satisfaction, and weaning in the first three months after birthJournal of Human Lactation 2003 19(2):145-56. [Google Scholar]
[18]. Schluter PJ, Carter S, Percival T, Exclusive and any breast-feeding rates of Pacific infants in Auckland: Data from the pacific islands families first two years of life studyPublic Health Nutrition 2006 9(6):692-99. [Google Scholar]
[19]. Sheehan D, Krueger P, Watt S, Sword W, Bridle B, The Ontario mother and infant survey: breastfeeding outcomesJournal of human lactation 2001 17(3):211-19. [Google Scholar]
[20]. Li R, Fein SB, Chen J, Grummer-Strawn LM, Why mothers stop breastfeeding: mother’s self-reported reasons for stopping during the first yearPediatrics 2008 122(suppl 2):S69-S76. [Google Scholar]
[21]. Neifert MR, Breastmilk transfer: positioning, latch-on, and screening for problems in milk transferClin Obstet Gynecol 2004 47(3):656-75. [Google Scholar]
[22]. Moore LC, Harris CV, Bradlyn AS, Exploring the relationship between parental concern and the management of childhood obesityMaternal and Child Health Journal 2012 16(4):902-08. [Google Scholar]
[23]. McDonald SW, Ginez HK, Vinturache AE, Tough SC, Maternal perceptions of underweight and overweight for 6–8 years olds from a Canadian cohort: reporting weights, concerns and conversations with healthcare providers BMJ Open 2016 6:e012094 [Google Scholar]
[24]. International Institute for Population Sciences (IIPS) and Macro International. 2016. National Family Health Survey (NFHS-4), India, 2015-16: West Bengal. Mumbai: IIPS. http://rchiips.org/nfhs/pdf/NFHS4/WB_FactSheet.pdf[Last accessed on 12th October 2017] [Google Scholar]
[25]. Shumey A, Demissie M, Berhane Y, Timely initiation of complementary feeding and associated factors among children aged 6 to 12 months in Northern Ethiopia: an institution-based cross-sectional studyBMC Public Health 2013 13(1):1050 [Google Scholar]
[26]. Onyango AW, Esrey SA, Kramer MS, Continued breastfeeding and child growth in the second year of life: a prospective cohort study in western KenyaLancet 1999 354(9195):2041-45. [Google Scholar]
[27]. Madise NJ, Mpoma M, Child malnutrition and feeding practices in MalawiFood Nutr Bull 1997 18(2):190-201. [Google Scholar]
[28]. Roy S, Dasgupta A, Pal B, Feeding practices of children in an urban slum of KolkataIndian J Community Med 2009 34(4):362-63. [Google Scholar]
[29]. International Institute for Population Sciences (IIPS) and Macro International. 2008. National Family Health Survey (NFHS-3), India, 2005-06: West Bengal. Mumbai: IIPS. Available from: http://rchiips.org/NFHS/NFHS-3%20 Data/wb_state_report_printed_version.pdf. Last accessed February 15, 2017 [Google Scholar]
[30]. Tarrant RC, Younger KM, Sheridan PM, White MJ, Kearney JM, Factors associated with weaning practices in term infants: a prospective observational study in IrelandBr J Nutr 2010 104:1544-54. [Google Scholar]
[31]. Cavalcante Caetano M, Ortiz Ortiz TT, Lopes Da Silva SG, Suano De Souza FI, SaccardoSarni RO, Complementary feeding: inappropriate practices in infantsRevistachilena de Pediatría 2012 83(5):503 [Google Scholar]
[32]. Aggarwal A, Verma S, Faridi MM, Complementary feeding—reasons for inappropriateness in timing, quantity and consistencyIndian Journal of Pediatrics 2008 75(1):49-53. [Google Scholar]
[33]. Parekh C, Bavdekar SB, Shaharao V, Study of infant feeding practices: factors associated with faulty feedingJournal of Tropical Pediatrics 2004 50(5):306-08. [Google Scholar]
[34]. Gatti L, Maternal perceptions of insufficient milk supply in breastfeedingJournal of Nursing Scholarship 2008 40(4):355-63. [Google Scholar]
[35]. Haider R, Rasheed S, Sanghvi TG, Hassan N, Pachon H, Islam S, Breastfeeding in infancy: identifying the program-relevant issues in BangladeshInt Breastfeed J 2010 5:21 [Google Scholar]
[36]. Semahegn A, Tesfaye G, Bogale A, Complementary feeding practice of mothers and associated factors in HiwotFana Specialized Hospital, Eastern EthiopiaPan African Medical Journal 2014 18:143 [Google Scholar]
[37]. Harris N. Perceived insufficient breastmilk and infant feeding practices for mothers of infants from birth to four months - a mixed methods study (Thesis, Master of Science). University of Otago. 2011 Retrieved from http://hdl.handle.net/10523/1808 [Last accessed on 3rd September 2017] [Google Scholar]
[38]. Tiwari S, Bharadva K, Yadav B, Malik S, Gangal P, Banapurmath CR, Infant and young child feeding guidelinesIndian Pediatrics 2016 53(8):703-13. [Google Scholar]