Periodontally Accelerated Osteogenic Orthodontics (PAOO) Assisted Management of Palatally Impacted Canine with Five Years Follow Up
R. Navaneethan1, K.K. Shantha Sundari2, K. Ambika3
1 Senior Lecturer, Department of Orthodontics and Dentofacial Orthopedics, Saveetha Dental College, Saveetha University, Chennai, Tamil Nadu, India.
2 Professor and Head, Department of Orthodontics and Dentofacial Orthopedics, Saveetha Dental College, Saveetha University, Chennai, Tamil Nadu, India.
3 Senior Lecturer, Department of Orthodontics and Dentofacial Orthopedics, SRM Dental College, Potheri, Srm Nagar, Kattankulathur, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. R. Navaneethan, Senior Lecturer, Department of Orthodontics, Saveetha Dental College, No: 162, Poonamallee High Road, Vellappanchavadi, Chennai-600077, Tamil Nadu, India.
E-mail: dentistry.sparkle@gmail.com
Periodontally Accelerated Osteogenic Orthodontics (PAOO), a patented technique by the Wilcko brothers has become very popular in reducing the treatment time in Orthodontics. A 17-year-old male patient presented to the Department with a Class I skeletal and a Class I dental pattern with bilateral canine impactions. The canine impaction was buccal on the right side (13) and palatal on the left side (23). The initial treatment plan was to disimpact 13 with a piggy back wire and 23 using the K9 spring respectively and it did not involve the PAOO Technique. However, six months into treatment, the patient stopped reporting for his regular appointments and reported after a time interval of one and a half years to continue his treatment. At the time of his return, considerable bone loss around the region of 23 was noticed on radiographs. The PAOO technique was therefore, carried out to augment bone around 23 as well as reduce the time for treatment.
Accelerated orthodontics, Alveolar corticotomies, Orthodontic tooth movement
Case Report
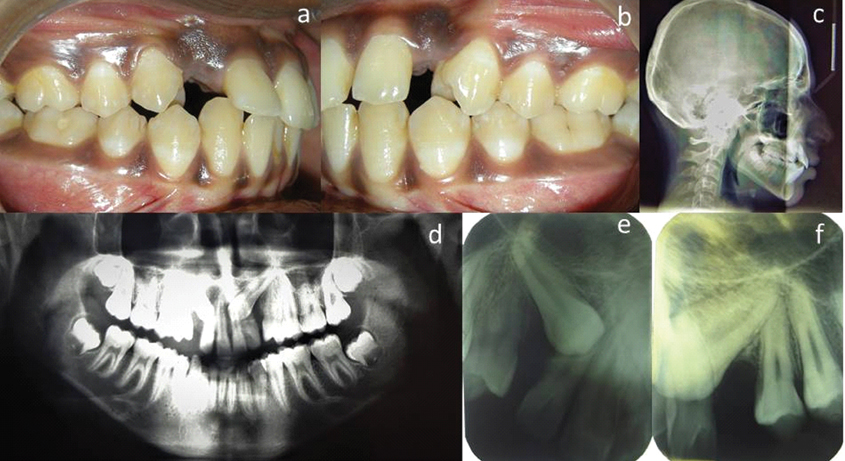
A 17-year-old male patient presented to the Department of Orthodontics with a Skeletal Class I pattern and an Angle’s Class I malocclusion with proclined upper and lower anteriors and missing maxillary canines [Table/Fig-1a-c]. The OPG revealed that the patient had bilaterally impacted canines [Table/Fig-1d]. Further, radiographic examination using the SLOB technique revealed that the canine impaction was buccal on the right side (13) and palatal on the left side (23) [Table/Fig-1e,f].
Pretreatment photographs and radiographs: a) Intraoral photograph-right buccal view showing missing right canine(13); b) Intraoral-left buccal view showing missing left canine(23); c) Pretreatment Lateral Cephalogram showing proclined upper teeth; d) OPG showing bilaterally impacted maxillary canines; e) Intraoral periapical radiograph of bucally impacted 13; f) Intraoral periapical radiograph of palatally impacted 23.
After going through a comprehensive analysis of the patient, the initial treatment plan was to extract all four first premolars to gain space for the disimpaction of the canines and correction of proclination of the anterior teeth. Disimpaction of 13 using the piggy back technique [1] and 23 using K9 spring [2] followed by final space closure with Friction Mechanics was planned.
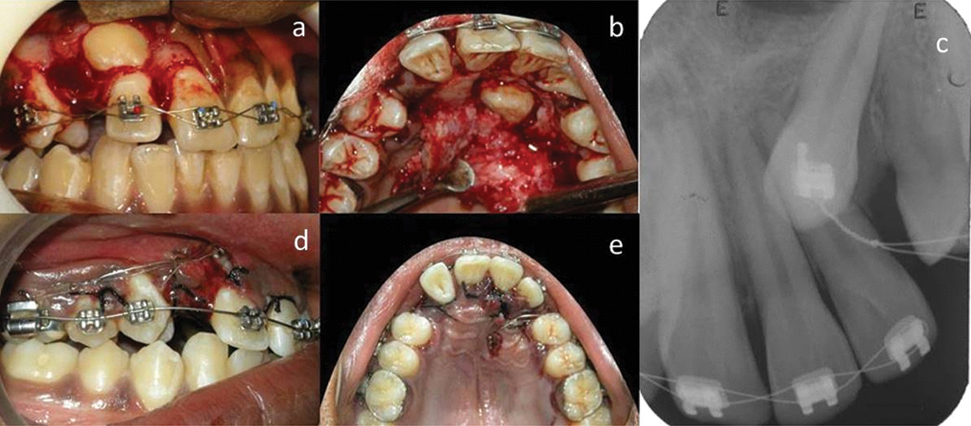
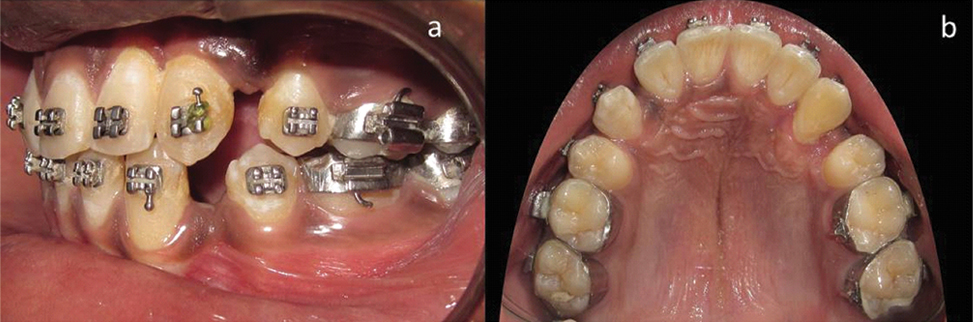
The patient was strapped up with a 0.022 slot MBT (McLaughlin-Bennett-Trevisi) prescription bracket system and a 0.016 inch Nickel Titanium (NiTi) wire. After 2 months, when the wire had been stepped up to a 0.016x 0.022 inch NiTi, mucoperiosteal flaps were raised to expose the impacted canines[Table/Fig-2a,b]. The canine brackets were then bonded to the impacted canines [Table/Fig-2c]. After bonding the brackets, the full thickness flaps were sutured back leaving a small window for the canine brackets. The canine bracket of the palatally impacted canine (23) and the bucally impacted canine (13) were then ligated to the main arch wire (0.016x0.022 inch NiTi) and the molar hook of 16 respectively using Stainless Steel ligature wires [Table/Fig-2d,e].
Surgical exposure of the impacted canines; a) Exposure of the bucally impacted canine (13) by raising the buccal mucoperiosteal flap; b) Exposure of the palatally impacted canine (23); c) Radiograph of 23 after bonding of canine bracket and closure of the palatal flap; d) Ligature wire extending from the bracket of the bucally impacted 13 to the molar hook of 16; e) Ligature wire extending from the bracket of the palatally impacted 23 to the main arch wire.
One month later, the first premolars were extracted to gain space for the impacted canines and the main arch wire was stepped up to 0.016x 0.022 inch Stainless steel wire. A 0.0155 inch Stainless steel Coaxial wire was used to correct the bucally impacted canine (13) with the piggy back technique. Along with the piggy back technique, an active ligation using an elastic module and ligature wire was used to apply a distal force to 13 from the molar (16) [Table/Fig-3a]. The 0.016 x 0.022 inch Stainless steel wire was segmental, in that it extended from right molar(16) to the lateral incisor of the opposite quadrant. A K9 spring, fabricated using a 0.017x0.025 inch TMA (Titanium Molybdenum Alloy) wire was used for the correction of the palatally impacted 23 [Table/Fig-3b,c].
Disimpaction of canines: a) Piggy back technique used for the disimpaction of bucally impacted 13: b) Occlusal view showing the K9 spring secured to the palatally impacted 23: c) Buccal view showing the K9 spring.

After a time period of 4 months, 13 had aligned with the arch while the crown of 23 had emerged from the palatal bone and had a 90 degree mesio palatal rotation. However, the patient was not able to make his regular monthly visits after the initial 6 months due to personal reasons. He came back to continue treatment after a period of one and a half years.
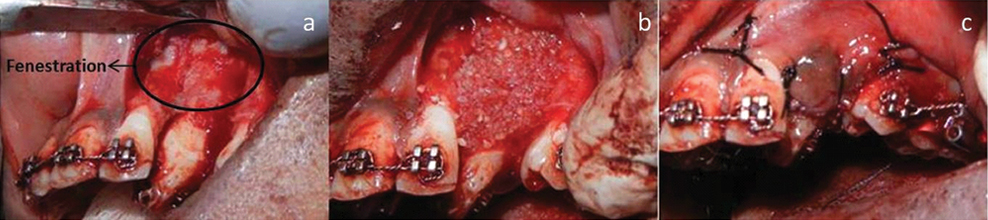
Modification of the treatment plan: The radiographic examination done when the patient had returned to continue his treatment after one and a half years, revealed bone loss in the region distal to 23 [Table/Fig-4]. Hence, in order to make up for the lost time as well as to augment the bone in the region of the palatally impacted canine (23), a PAOO procedure along with a Freeze Dried Irradiated Bone Allograft (FBDA) was performed with the patients consent. The buccal mucoperiosteal flap in relation to 23 was raised and vertical corticotomy cuts were given in the bone mesial and distal to 23. The fenestration that was visible in relation to 22 and 23 on raising the flap further, confirmed the compromised nature of the periodontium [Table/Fig-5a]. The two vertical corticotomy cuts were connected by a horizontal corticotomy cut made above the root apex of 23. The cuts were followed by bone augmentation using FDBA and the mucoperiosteal flap was then sutured back [Table/Fig-5b,c]. The patient was prescribed 500 mg Amoxicillin for three days and paracetamol 500 mg twice daily for 1 day after the PAOO procedure.
Intraoral periapical radiograph showing bone loss distal to 23 (when the patient returned for treatment after one and a half years).

PAOO procedure in relation to 23: a) Elevation of the buccal mucoperiosteal flap showing fenestrations in 22 and 23 region: b) Freeze dried irradiated bonegrafts placed after corticotomy cuts were given mesial and distal to 23: c) Flap sutured back after PAOO procedure.
Following the PAOO procedure, a couple force was given to derotate 23 [Table/Fig-6a-c]. Once a significant amount of derotation was achieved, a 0.017 x 0.025 inch Cu-NiTi (copper-NiTi) was placed to bring about the final derotation and position 23 along the arch. The derotation and alignment of the canine into the maxillary arch was completed in 45 days [Table/Fig-7a,b]. Once 23 was fully corrected, the remaining spaces were closed with friction mechanics [Table/Fig-8a-d]. The retention protocol followed was a Begg’s wrap around retainer in the upper arch and fixed retainer in the lower arch.
Derotation and correction: a) Buccal view of a couple force being applied to derotate 23 while the space is being maintained with an open coil spring: b) Occlusal view showing elastics used to apply a coupled force on 23: c) Radiograph showing rotated 23.
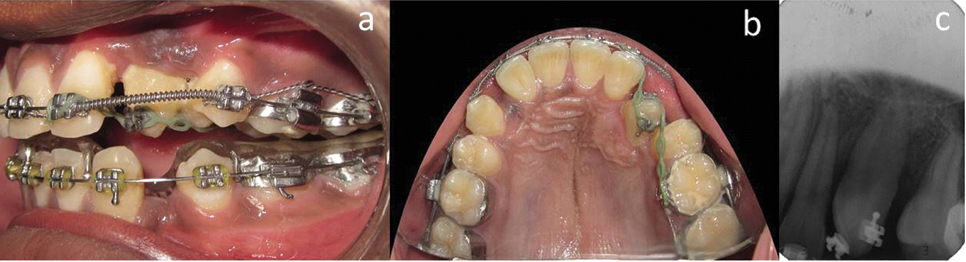
Post Derotation: a) Buccal view after correction of canine rotation (23): b) Occlusal view after correction of canine rotation (23).
Post Treatment Pictures and radiographs (made 9 months after PAOO Procedure): a) Intraoral frontal image showing good occlusion in the maxillary arch: b) Post treatment lateral cephalogram showing correction of proclination: c) Post treatment OPG: d) Post treatment Intraoral periapical radiograph of 23 showing adequate bone around 23.
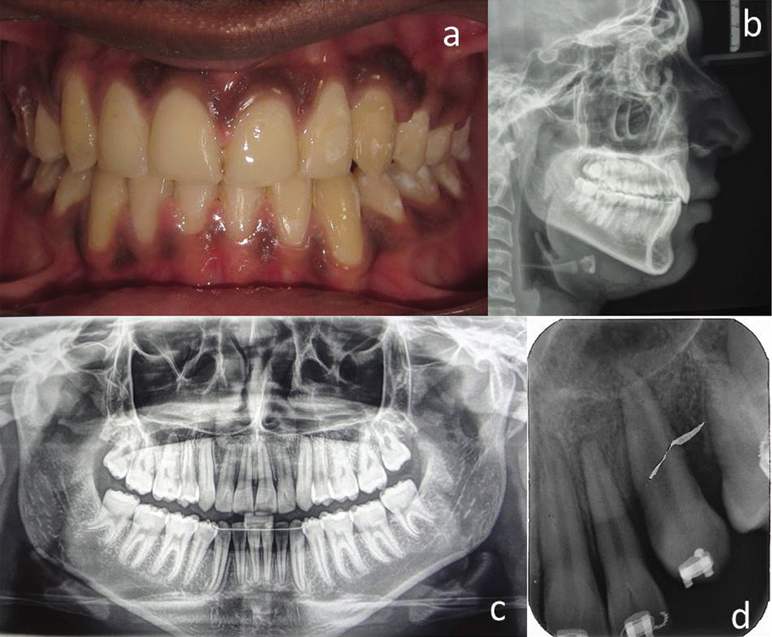
Post treatment follow up after five years: The patient was recalled after five years for re-evaluation and an intraoral radiograph (RVG) for the 23 region was made. The radiograph showed the presence of sufficient bone and an intact lamina dura distal to 23 region. The occlusion appeared to be fairly stable except for the slight mesio palatal rotation that had recurred in 23 [Table/Fig-9a-d].
Recall evaluation after 5 years: a) Frontal view showing good occlusion 5 years after treatment completion: b) Left buccal view: c) Right buccal view: d) Intraoral radiograph (RVG) of 23 showing adequate bone levels and slight root resorption.

Discussion
Among the various methods of accelerating treatment, Corticotomy has become very popular in the recent years due to its effectiveness [3]. It is based on the “Regional Acceleratory Phenomenon (RAP)”, where an injury to bone causes a rapid outburst of a localized remodelling which accelerates the healing process [4]. The teeth adjacent to the corticotomy sites move faster due to the reduced resistance from bone that is undergoing rapid bone remodelling [5]. The Wilcko brothers developed their patented PAOO technique which advocated the use of corticotomy cuts along with alveolar augmentation with bone grafts [6].
Animal and human studies have shown that corticotomy procedures reduce orthodontic treatment time without affecting the periodontium [7-11]. Fischer has shown that corticotomy procedure reduces the treatment time in case of palatally impacted canines [12]. However, no study has been done so far to use the PAOO procedure to improve the bone levels in patients with bone loss.
In the present case, the total treatment time taken for the correction of 23 following PAOO was 45 days. The remaining treatment after canine correction was completed in 9 months. It has to be taken into consideration that the PAOO procedure was carried out only on the buccal surface of the palatally impacted maxillary canine (23) as the procedure was not done to bring about space closure but to correct the position and rotation of 23 and to augment the bone around it. The use of freeze dried bone graft ensured sufficient buccal bone for the canine (23) at the end of the treatment.
Some of the advantages of PAOO apart from rapid tooth movement include lack of any appreciable root resorption and maintainence of vitality of the tooth being moved [3,13]. In our case, the canine presented with a very mild blunting which was not evident on debonding records. This can be attributed to the long trail traversed by the 23 to be brought to alignment. The picture presented by the five year post treatment evaluation also stands testimony to the stability of the PAOO treatment.
Conclusion
PAOO could be a boon in all difficult cases of Orthodontic tooth movement. The main advantage of the technique is that it has neligible deleterious effects on the teeth. Adult patients who have a denser bone but require rapid treatment could be encouraged to undergo this technique as it has been shown that PAOO assisted tooth movement has better post treatment stablity when compared to conventional Orthodontics.
[1]. Sandler PJ, Murray AM, Di Biase D, Piggyback archwiresClin Orthod Res 1999 2(2):99-104. [Google Scholar]
[2]. Varun Kalra, The K-9 spring for Alignment of Impacted CaninesJCO 2000 34(10):606-10. [Google Scholar]
[3]. Buschang PH, Campbell PM, Ruso S, Accelerating tooth movement with Corticotomies. Is it possible and desirable?Semin Orthod 2012 18(4):286-94. [Google Scholar]
[4]. Verna C, Regional Acceleratory phenomenonFront Oral Biol 2016 18:28-35. [Google Scholar]
[5]. Goldie RS, King GJ, Root resorption and tooth movement in orthodontically treated, calcium-deficient, and lactating ratsAm J Orthod 1984 85:424-30. [Google Scholar]
[6]. Wilcko MT, Wilcko WM. Orthodontic method and device. US patent 6,109,916 A. 29th Aug 2000 [Google Scholar]
[7]. Wilcko MT, Wilcko WM, Bissada NF, An evidence-based analysis of periodontally accelerated orthodontic and osteogenic techniques: a synthesis of scientific perspectivesSemin Orthod 2008 14(4):305-16. [Google Scholar]
[8]. Aboul SMBED, El-Beialy AR, El-Sayed KMF, Selim EMN, El-Mangoury NH, Mostafa YA, Miniscrew implant-supported maxillary canine retraction with and without corticotomy-facilitated orthodonticsAm J Orthod Dentofacial Orthop 2011 139(2):252-59. [Google Scholar]
[9]. Mostafa YA, Fayed MM, Mehanni S, ElBokle NN, Heider AM, Comparison of corticotomy-facilitated vs standard tooth-movement techniques in dogs with miniscrews as anchor unitsAm J Orthod Dentofacial Orthop 2009 136(4):570-77. [Google Scholar]
[10]. Ren A, Lv T, Zhao B, Chen Y, Bai D, Rapid orthodontic tooth movement aided by alveolar surgery in beaglesAm J Orthod Dentofacial Orthop 2007 131(2):160.e1-10. [Google Scholar]
[11]. Iino S, Sakoda S, Ito G, Nishimori T, Ikeda T, Miyawaki S, Acceleration of orthodontic tooth movement by alveolar corticotomy in the dogAm J Orthod Dentofacial Orthop 2007 131(4):448.e1-448.e8. [Google Scholar]
[12]. Fischer TJ, Orthodontic Treatment Acceleration with Corticotomy-assisted Exposure of Palatally Impacted CaninesThe Angle Orthodontist 2007 77(3):417-20. [Google Scholar]
[13]. Ferguson DJ, Nazarov A D, Makki L, Wilcko MT, Wilcko WM, Post treatment and retention outcomes with and without periodontally accelerated osteogenic orthodontics assessed using ABO objective grading systemAPOS Trends Orthod 2016 6(4):194-99. [Google Scholar]