Degenerated Cystic Uterine Myoma Mimicking Postpartum Haemoperitonium
Servet Gençdal1, Hüseyin Aydoğmuş2, Serpil Aydogmus3, Zafer Kolsuz4, Sefa Kelekçi5
1 Lecturer, Department of Obstetrics and Gynecology Clinic, Izmir Atatürk Education and Research Hospital, Ministry of Health, Izmir, Turkey.
2 Lecturer, Department of Obstetrics and Gynecology Clinic, Izmir Atatürk Education and Research Hospital, Ministry of Health, Izmir, Turkey.
3 Associate Professor, Department of Obstetrics and Gynecology, Izmir Katip Celebi University, School of Medicine, Izmir, Turkey.
4 Lecturer, Department of Obstetrics and Gynecology Clinic, Izmir Atatürk Education and Research Hospital, Ministry of Health, Izmir, Turkey.
5 Professor, Department of Obstetrics and Gynecology, Izmir Katip Celebi University, School of Medicine, Izmir, Turkey.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Servet Gençdal, Lecturer, Department of Obstetrics and Gynecology Clinic, Izmir Atatürk Education and Research Hospital, Ministry of Health, Izmir, Turkey.
E-mail: servetgencdal@hotmail.com
Haemoperitoneum due to spontaneous haemorrhage of intraleiomyoma is a very rare complication of uterine myoma. Acute complications of uterine myoma are seldom seen, but it may be fatal. We hereby report case of a female, who presented with abdominal pain and distension, postpratum, found to have degenerated cystic uterine myoma, mimicking postpartum haemoperitonium.
Cystic degeneration, Myoma uteri, Intrauterine haematoma
Case Report
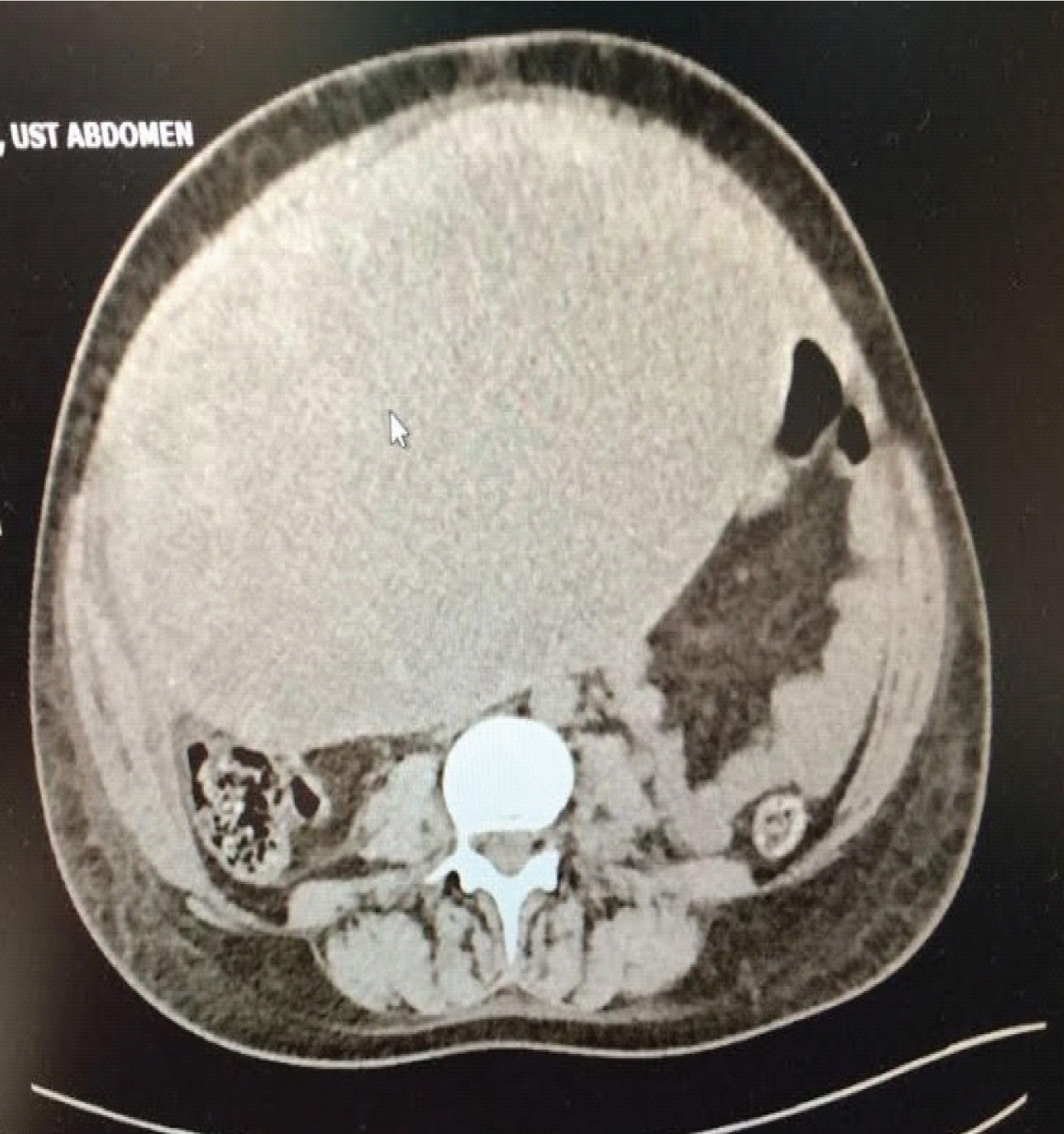
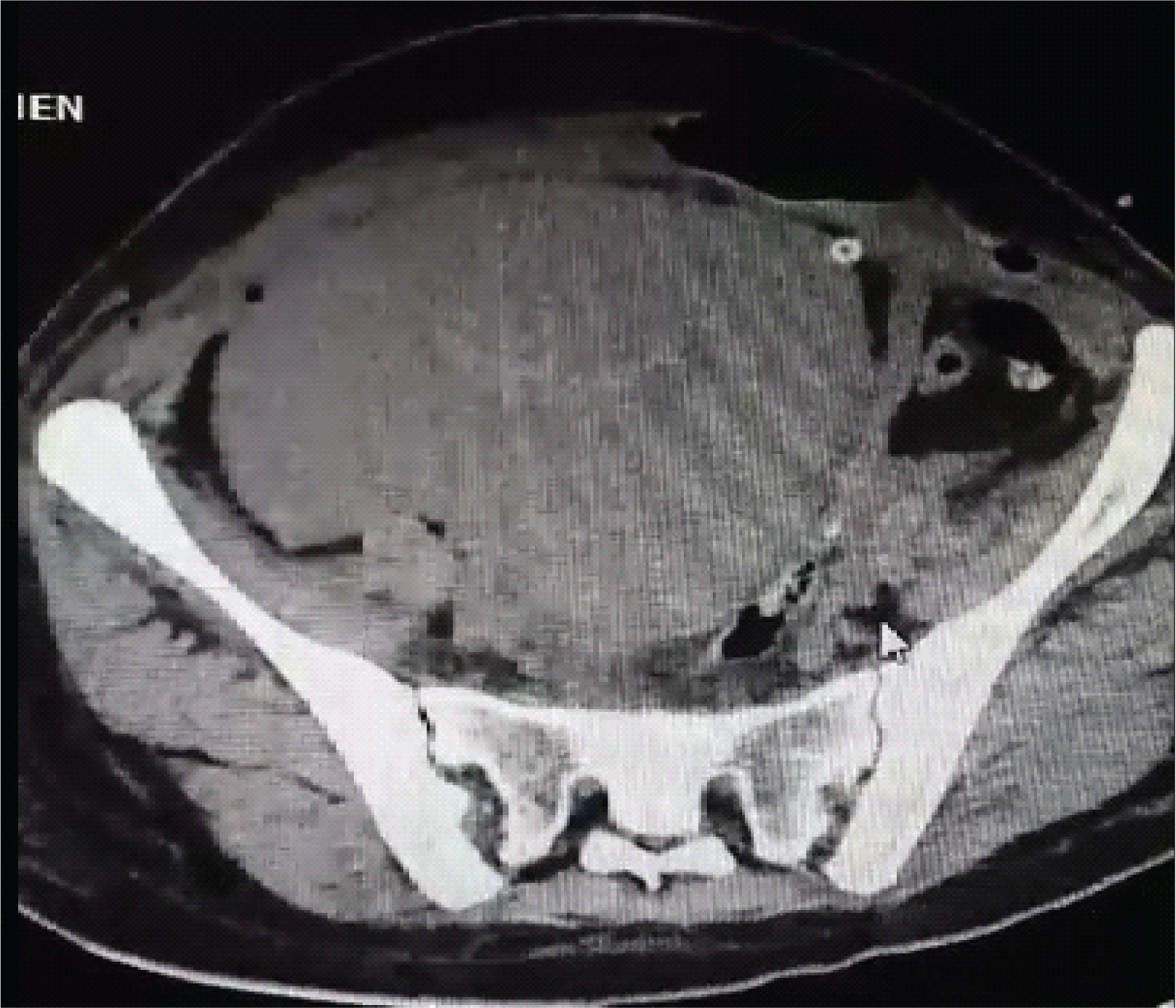
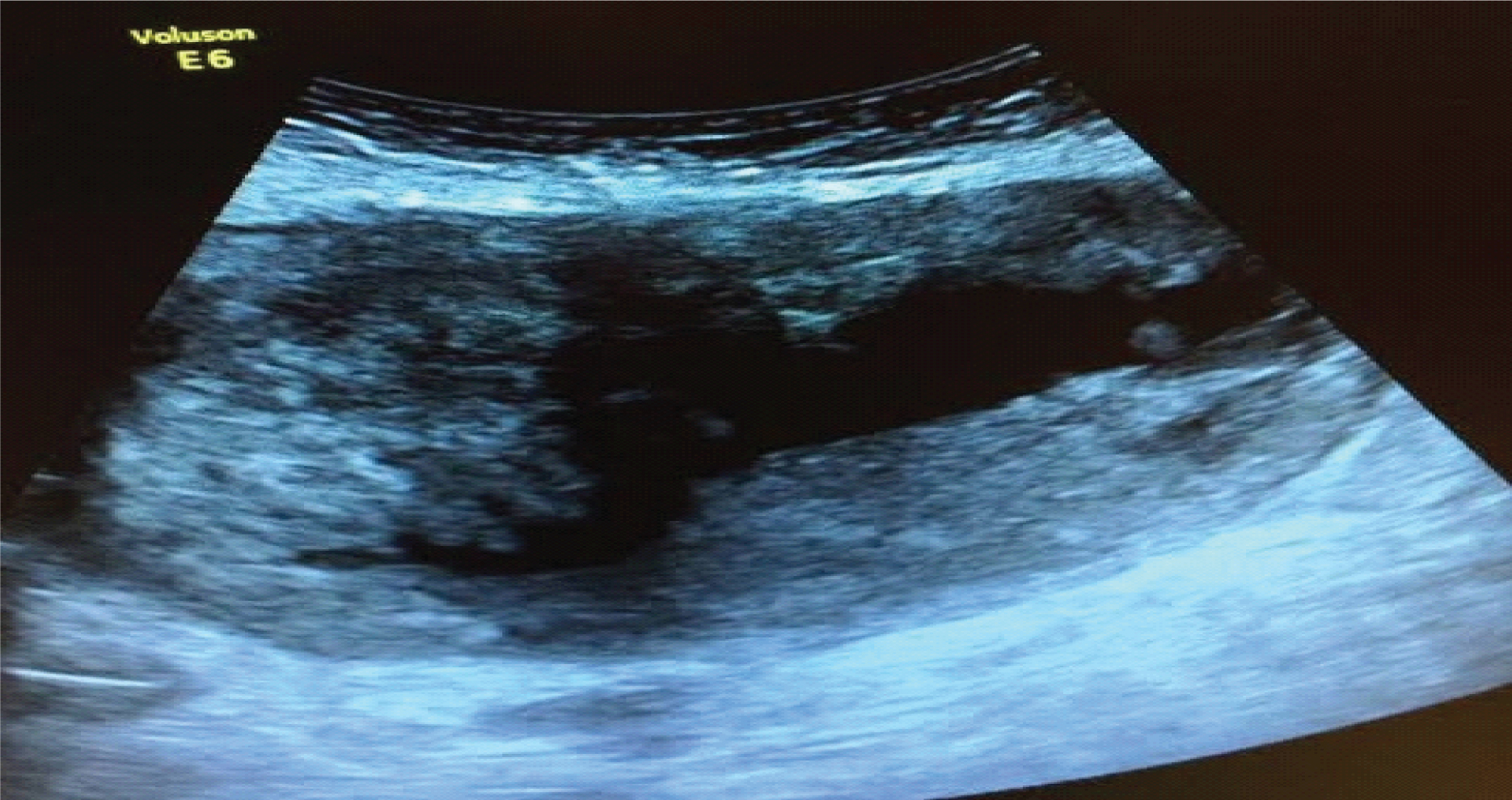
A 25-year-old, female gravida 1 and parity 0, was admitted to a local clinic for abdominal pain in her 35th week of gestation. Her vitals were stable and her medical history was unremarkable. The Ultrasonography (USG) examination revealed a 10-15 cm haematoma in posterior fundus behind the placenta and the patient was taken for emergency caesarean section with an initial diagnosis of placental abruption. A 2600 gm, male baby was born alive and there was no sign of placental abruption or placental separation. The haematoma detected on USG was found to be a 15–20 cm blue-purple mass near the uterus and the patient and her baby were transferred to our clinic with a possible diagnosis of postpartum haematoma; since, the local hospital did not have the necessary equipment to manage such kind of situation. Before the transfer, an abdominal drain was placed by the gynaecologist. The patient’s general condition was good-to-moderate and her vitals were stable. The discharge from the drain was 200 cc which was serous-haemorrhagic type. Urine output was 700 cc and post operative Haemoglobin (Hb) level was 8.7 gm/dL. USG in our clinic revealed a 15.8 ×17.6 cm cystic mass which was arising from the uterine fundus. The patient was given two units of packed cells and one unit of fresh-frozen plasma. Susequent Hb was measured as 10.4 gm/dL and patient’s vitals were stable on the second day. However, the patient did not pass any gas or stool during that period. Abdominal drain was removed on second day after measuring 30 cc serous-haemorrhagic fluid discharge. On post operative day 3, the patient started to show signs of abdominal distension with still no passage of gas or stool, but she did not have acute abdomen findings. Following consultation from general surgery clinic, a total abdominal Computed Tomography (CT) was ordered by the surgeons. Abdominal CT results revealed an 18 × 18.5 cm cystic mass on fundus-corpus section which was reported as post operative intrauterine haematoma [Table/Fig-1,2]. CT was only sagittal, there was no coronal plane, because general surgeons ordered one plane for emergency conditions. Due to progressing abdominal distension, general surgeons considered re operation for both possible ileus and evacuation of haematoma, but patient did not give consent for the surgery. Hence, drainage of haematoma was planned after obtaining patient’s written consent. Under local anaesthesia, an 18-gauge spinal needle was used with USG guidance to enter the cystic mass from left side of umbilicus. [Table/Fig-3] shows uterine myoma with cystic degeneration. About 200 cc of serous fluid was aspirated. After shrinkage of cystic mass, the mass was found to be a subserous myoma placed on uterus fundus posterior. After drainage of haematoma, patient passed gas and stool and did not have any complaint. The patient was discharged as desired on fourth day of operation. Patient was informed about possible complications and symptoms. On 10th day of operation patient was seen in the clinic and no complications were detected.
Computed tomography shows an 18 × 18.5 cm wide post operative intrauterine haematoma.
Computed tomography shows post operative intrauterine haematoma.
Uterine myoma with cystic degeneration which was misdiagnosed as haematoma in USG.
Discussion
Leiomyoma is a benign tumour that originates from uterine smooth muscle cells. They can be seen in 1 out of 5 women during reproductive period [1]. About 10-40% of myomas can cause complications during pregnancy [2]. Elevated oestrogen level may cause its enlargement during the first trimester of pregnancy; thus, 15-30% myomas may enlarge during pregnancy and shrink during puerperium [3]. The various types of degeneration include hyaline, myxoid, cystic, and red degeneration [4]. Myoma degeneration can cause pain during pregnancy by causing torsions of the myomas with a base or uterus torsion due to mass effect. Abrupt intraperitoneal haemorrhage with fibroid uterus can also be seen as acute abdomen. However, in our case there was no sign of acute abdomen [5]. The bleeding is likely to occur from torn enlarged veins coursing over the surface of subserous leiomyomas, resulting in haemoperitonium and hypovolemic shock [6]. Spontaneous haemoperitonium due to fibroid rupture is a rare entity with less than 100 cases reported in the literature [6]. Ultrasound is often the initial diagnostic imaging modality for suspected complications of fibroids. However, USG examinations loose their diagnostic power in late term pregnancy and the lesions detected are frequently misdiagnosed as either adnexa masses or haemorrhage, as in our case. Initial USG examination of the patient was suggestive of placental abruption and hence, she was taken for emergency caesarean section.
Degeneration of leiomyoma gives a greater complex ultrasound view with fields of cystic alteration and Doppler may show peripheral vascularity. The diagnosis of ruptured uterine fibroid may be clinically difficult but, CT and Magnetic Resonance Imaging (MRI) can aid in correctly establishing the diagnosis [7]. CT is not the primary modality for diagnosing or evaluating fibroids; however, fibroids are often found incidentally on CT scan. Therefore, familiarity with their various CT appearances is important [8]. The typical finding is a bulky, irregular uterus, or a mass in continuity with the uterus. In our case uterus was not seen properly because of bulky/enlargement of myoma uteri mimicking haematoma [Table/Fig-1].
Magnetic resonance imaging is highly accurate in evaluating leiomyoma size, number, location, and presence or extent of degeneration, but it requires a stable patient and may be difficult to perform in a timely fashion in the emergency department [9]. Although, the vitals of our case were stable, no MRI was ordered since both the USG and CT scan cystic mass interpreted the mass as a haematoma.
In literature, case reports about drainage of cystic degenerated myoma are very few; when reported these are CT guided for temporary relief of symptoms, where myomectomy surgery is unavailable. We feel that this case is unique, because USG guided aspiration was done for both patient symptom relief and to aid in diagnosis.
Conclusion
Though, uterine leiomyoma generally has a typical USG view, degenerating fibroids can have variable presentation and be a diagnostic challenge. MRI may be helpful in complicated cases but should not be used indiscriminately. Multidisciplinary approach and possibilities of differentials may be helpful in the diagnosis and management of such cases.
[1]. Duhan N, Advances in management of uterinemyomasFront Biosci (Elite Ed) 2013 1(5):12-22. [Google Scholar]
[2]. Ouyang DW, Obstetric complications of fibroidsObstet Gynaecol Clin North Am 2006 33(1):153-69. [Google Scholar]
[3]. Raja K, Tasleem H, Effects of uterine leiomyoma on the course of pregnancy and labourRawal Medical Journal 2009 34(1):79-81. [Google Scholar]
[4]. Dasari P, Maurya DK, Haemoperitoneum associated with fibroid uterusJ Obstet Gynaecol India 2005 55:553-54. [Google Scholar]
[5]. Sue W, Scott-Barrett S, Radiological appearances of uterine fibroidsIndian J Radiol Imaging 2009 19:222-31. [Google Scholar]
[6]. Manopunya M, Tongprasert F, Sukpan K, Tongsong T, Intra-leiomyoma massive haemorrhage after deliveryJ Obstet Gynaecol Res 2013 39:355-58. [Google Scholar]
[7]. Kamat NV, Telkar HB, Ramani SK, Thakker AP, Ruptured degenerated uterine fibroid diagnosed by imagingObstet gynaecol 2001 98(5 Pt 2):961-63. [Google Scholar]
[8]. Bennett GL, Slywotzky CM, Giovanniello G, Gynaecologic causes of acute pelvic pain: Spectrum of CT findingsRadiographics 2002 22:785-801. [Google Scholar]
[9]. Lotterman S, Massive haemoperitoneum resulting from spontaneous rupture of uterine leiomyomaAm J Emerg Med 2008 26:974.e1-2. [Google Scholar]