Clitoral Leiomyoma with Condyloma Accuminata in Young Female: A Rare Case Report
Taru Gupta1, Deepika2, Sangeeta Gupta3
1 Professor, Department of Obstetrics and Gynaecology, ESI-PGIMSR, Basaidarapur, Delhi, India.
2 Senior Resident, Department of Obstetrics and Gynaecology, ESI-PGIMSR, Basaidarapur, Delhi, India.
3 Senior Consultant and Head, Department of Obstetrics and Gynaecology, ESI-PGIMSR, Basaidarapur, Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sangeeta Gupta, Senior Consultant and Head, Department of Obstetrics and Gynaecology, ESI-PGIMSR, Basaidarapur-110092, Delhi, India.
E-mail: sangeetagupta58@hotmail.com
Leiomyomas are benign tumours of the smooth muscle. They occur predominantly during the reproductive age especially in females. Clitoral leiomyoma is a rare tumour and is usually asymptomatic but can present as a local growth with urinary complaints. MRI has a very high detection rate in the diagnosis as well as differentiation of benign from malignant. Here we are reporting a rare case of 22-year-old sexually active female with clitoral mass diagnosed as case of clitoral leiomyoma (rare location) with localised condyloma accuminata.
Clitoral mass, Genital warts, Nulliparous, Koilocytes
Case Report
A 22-year-old nulliparous sexually active female with multiple sexual partners presented to the Obstetrics and Gynaecology outpatient department with complaints of a swelling in the vulval region since 11 months. Patient denied lower urinary tract symptoms. There was history of dyspareunia. The swelling was painless and gradually increased to its present size. It was not associated with any history of local trauma. She attained menarche at the age of 14 years and menstrual cycles were normal and regular.
On general physical examination, her secondary sexual characters were normal. On local examination, there was an ovoid pink firm mass of 4x3 cm arising from clitoris with finger like projections on the surface [Table/Fig-1]. The mass was non tender, irreducible, non compressible. There were no ulceration and degenerative changes. Urethra was identified separately from the clitoral swelling. There was no other growth or lesion in the local area. The inguinal lymph nodes were not palpable. A provisional diagnosis of condyloma accuminata of the clitoris was made.

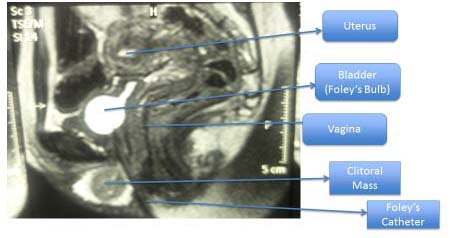
Human Papilloma Virus (HPV) DNA-16 and 18 was negative; HPV 6 and 11 was equivocal. Pap smear was negative for intraepithelial lesions with mild inflammation. X-ray chest was normal. Dermatologist opinion was taken for the patient. On the basis of finger like projections, it was diagnosed as case of condyloma accuminata and treatment advised was local podophyllin resin 10% for four to six weeks. On clinical suspicion of condyloma accuminata, topical Podophyllin 10% resin was applied locally on weekly basis in five sittings. There was no appreciable decrease in the size of the mass in six weeks. For further evaluation, MRI of pelvis was done which revealed a well defined, soft tissue lesion arising from the vulvar region with non visualisation of clitoris separately likely clitoral mass with involvement of anterior urethral wall [Table/Fig-2]. Advised histopathological correlation to rule out benign or malignant nature. Superficial edge biopsy of mass shows acanthotic squamous epithelial lining with fibroepithelial tissue s/o benign lesion.
MRI T2W image showing clitoral mass.
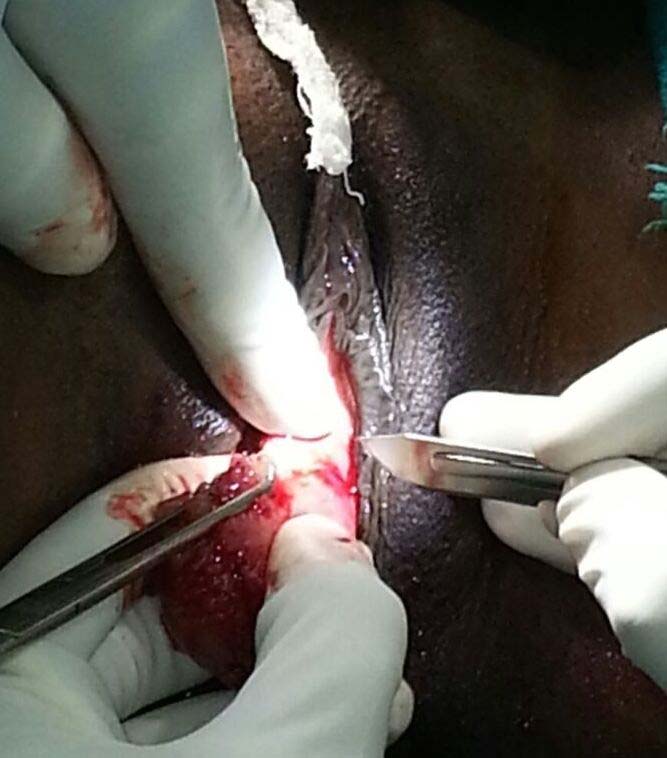
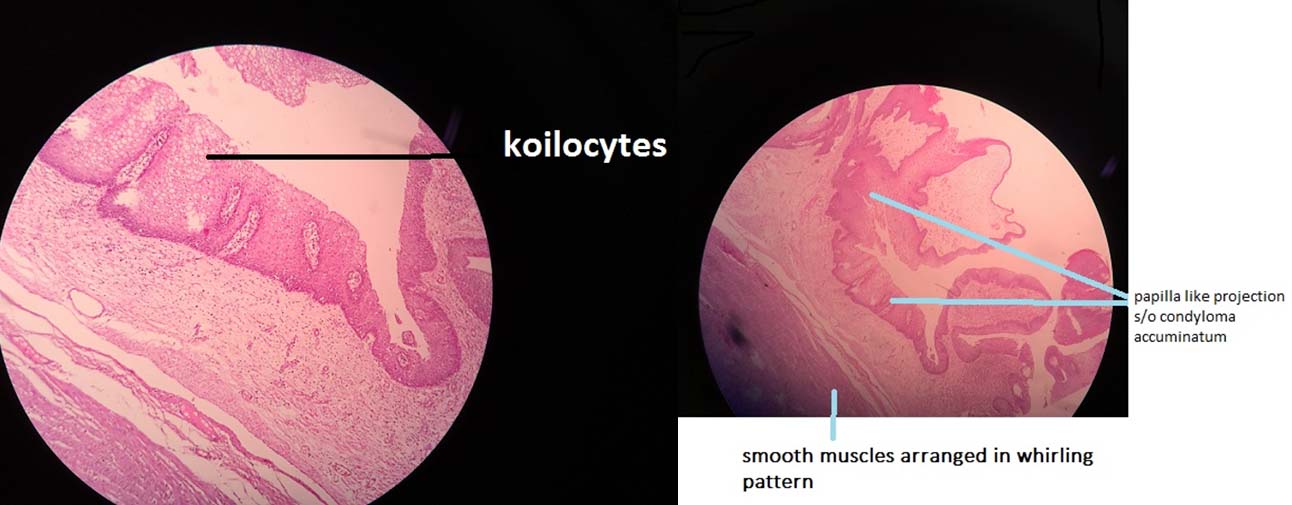
The urologist’s opinion was taken and cystoscopy was done to rule out urethral involvement. Decision for surgical excision of the clitoral mass was taken. Under spinal anesthesia, tumour was resected with circumferential incision at the base, removing the mass in toto, preserving the tip of clitoris followed by reconstruction of clitoris [Table/Fig-3]. Indwelling Foleys catheter number 18 was kept inserted for 10 days. Patient was discharged on third postoperative day. Histopathological examination of the excised specimen revealed spindle shaped smooth muscle fibres in a whirling pattern suggesting leiomyoma. Tumour cells were positive for oestrogen and progesterone receptor (ER/PR) as well as for Smooth Muscle Actin (SMA), confirming the diagnosis of leiomyoma. There was presence of papillae of different sizes and shape, lined by acanthotic squamous epithelium. Koilocytic changes were present in the most superficial layers of the squamous epidermis with mild inflammation; these findings were suggestive of condyloma accuminata [Table/Fig-4]. No mitotic figures were observed in the lower third of the epidermis.
Excision of clitoral mass.
Haematoxyline and Eosin stain 40X shows leiomyoma with condyloma acuminatum.
Patient was diagnosed as a case of “clitoral leiomyoma with condyloma accuminata”. Patient was doing well postoperatively without any difficulty in voiding and is under regular follow up. Her cosmetic result was excellent and her dyspareunia had resolved. She received three doses (0,1,6 months) of quadrivalent vaccine for HPV infection.
Discussion
Most common site of occurrence of leiomyomas is uterus. The presentation of clitoral leiomyoma as found in the present case is very rare. The mesenchyme of the urogenital sinus can be the origin of clitoral leiomyoma [1]. The clitoral leiomyomas are usually asymptomatic, painless and non tender but can present with urinary symptoms of paraurethral leiomyomas like dysuria, urinary frequency, urinary retention, and dyspareunia [2].
The clinical history, physical examination and imaging technique are helpful in diagnosis of clitoral mass. A careful clinical examination, urethroscopy, and radiological examination of the lower urinary tract are essential to differentiate the mass from urethra and paraurethral lesions.
For investigation, MRI is very useful not only in diagnosis but also in differentiation of benign from malignant tumour stating about the involvement of urethra and lymph node status.
MRI mostly diagnose above condition with a characteristic finding of low intensity signals that resembles that of smooth muscle on T2W images and isointense with T1W images with homogenous enhancement on intravenous contrast enhanced images [2,3]. Diagnosis can be confirmed with biopsy, which shows spindle-shaped tumour cells, arranged in palisading pattern with few areas of myxoid and hyaline degeneration. IHC studies show positivity for SMA and ER/PR [2].
These tumours are considered malignant if they have three or more of the following criteria [2]:
If mass is of five centimeter or more in size;
Infiltrative margins;
Five or more mitotic figures per ten high power fields;
Moderate to severe cytological atypia.
In our case, findings were suggestive of benign tumour since it did not fulfill above mentioned conditions.
On reviewing literature, we have found very few cases of clitoris leiomyoma. Chandrasekar A et al., and Kumar S et al., reported a case of clitoral leiomyoma in post menopausal and premenopausal female respectively [1,2]. Kumar S et al., reported a case of 42-year-old premenopausal woman with fungating mass having ulceration; arising from the crus of the clitoris with the size of 11×9 cm; excision of the mass was done and diagnosed as clitoral leiomyoma [2].
Shaia K et al., reported a case of 24-year-old African- American with a peri-clitoral mass 2.3x1.4x2 cm since two months [4]. After excision the final pathology of the mass was reported as a leiomyoma.
Anogenital warts are benign in nature and present as proliferative epithelial growth. They are caused by infection with HPV. These are very common particularly in young people, however with the use of HPV vaccination, its incidence has declined [5]. Diagnosis by biopsy and viral typing is not required on routine basis and can be reserved for those cases where diagnosis is uncertain. The common sites of the lesion are labia, clitoris, urethral meatus, introitus, vagina and cervix. The majority of external genital warts are caused by HPV types 6 and 11, and minorities of genital warts are caused by HPV types 16 and 18. HPV 6 and 11 are not associated with increased risk of neoplastic transformation, whereas HPV 16 and 18 are associated with an increased risk of cervical cancer, vaginal cancer, vulval cancer, penile cancers, anal cancers, oral and oropharyngeal cancers. It is a very rare case of clitoral leiomyoma with localised genital wart. No such case has been reported yet.
For treatment of external and perianal genital warts CDC recommends topical application of 10-25% solution of podophyllin resin in benzoin tincture once weekly for upto three to six weeks. Maximum recommended area is 10 cm2 and maximum volume of treatment session is <0.5 ml [5].
Simple excision is curative. Main principle in the surgery is preservation of sexual arousal function and cosmetic. Surgery in the form of simple excision is usually sufficient [2]. The conservative treatment with long acting gonadotropin releasing hormone (GnRH) agonists or antagonists may be used as an adjuvant therapy, because of estrogen receptor expression in the tumour [2].
Conclusion
Clitoral leiomyoma is very rare benign tumour of female genital tract that presents a diagnostic challenge. They are usually asymptomatic, painless and non tender but can present with urinary symptoms. Preoperative imaging with USG and MRI aids in diagnosis. MRI has important role in diagnosis of leiomyoma. Excision of the mass with preservation of normal anatomy is the desired treatment. The diagnosis was confirmed by the biopsy, with spindle-shaped cells arranged in whirling pattern.
[1]. Chandrasekar A, Devakannan Thirunarayanan, Leiomyoma of Clitoris, an unusual cause of Clitoromegaly in a post menopausal patient- A Case Report and Review of the LiteratureInt J Med Health Sci 2012 1(3):104-07. [Google Scholar]
[2]. Kumar S, Agrawal S, Jayant K, Shankargowda SA, Large clitoral leiomyoma in a forty two-year-old Premenopausal womanNephrourol Mon 2014 6(3):e17022 [Google Scholar]
[3]. Hubert KC, Remer EM, Rackley RR, Goldman HB, Clinical and magnetic resonance imaging characteristics of vaginal and paraurethral leiomyomas: can they be diagnosed before surgery?BJU International 2010 105(12):1686-88. [Google Scholar]
[4]. Shaia K, Khan A, Walsh C, Nentin F, A 24-year-old female with a peri-clitoral massJ Cases Obstet Gynecol 2017 4(1):18-21. [Google Scholar]
[5]. Centers for Disease Control and PreventionSexually Transmitted Diseases Treatment Guidelines, 2015MMWR Recomm Rep 2015 64(No. RR-3):1-137. [Google Scholar]