Primary Multidrug-Resistant Extrapulmonary Tuberculosis Presenting as Empyema Necessitans in an Immuno-competent Young Girl
Jyoti Bajpai1, Surya Kant2, Ajay Kumar Verma3
1 Senior Resident, Department of Respiratory Medicine, King George’s Medical University, Lucknow, Uttar Pradesh, India.
2 Professor and Head, Department of Respiratory Medicine, King George’s Medical University, Lucknow, Uttar Pradesh, India.
3 Associate Professor, Department of Respiratory Medicine, King George’s Medical University, Lucknow, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Surya Kant, Professor and Head, Department of Respiratory Medicine, King George’s Medical University, Lucknow-226003, Uttar Pradesh, India.
E-mail: skantpulmed@gmail.com
Empyema Necessitans (EN) is a variant of empyema that extends to extrapleural space and can affect chest wall too. Although, tuberculosis is the most common cause of EN, primary multidrug resistant TB presenting as EN is rare. Despite the ominous upward trend of drug resistant pulmonary tuberculosis prevalence globally, only sparse reports of extrapulmonary involvement by drug resistant mycobacteria have been documented in literature. Uptill now, culture has been the gold standard for diagnosis of TB. However, the availability of simple and rapid molecular tests has made the diagnosis of extrapulmonary forms of TB possible with high sensitivity and specificity. Here, we report a case of primary Multidrug-Resistant (MDR) extrapulmonary tuberculosis presenting as EN in an immuno-competent young girl.
CECT thorax, Empyema, Molecular test
Case Report
A 15-year-old girl from northern India presented with chief complaints of right side chest pain with right anterior chest wall swelling for last two months. She had low grade fever with evening rise and weight loss of 5-7 kg for last one and half months. She had complaints of dyspnoea for last 15 days. She had no history of cough or haemoptysis. Fever was not associated with chills, rigors, rash, burning micturition or yellowish discoloration of sclera. Her weight was 35 kilos and she had lean body built. She had no history of tuberculosis in past and no history of tuberculosis in family members, no history of contact tuberculosis. Two month prior to presentation she developed right sided dull aching chest pain that was non radiating and she also developed a swelling in right anterior chest wall. There were no other systemic symptoms and no significant past medical history such as recurrent childhood infections, bronchial asthma, tuberculosis.
On examination, she was found to be ill, wasted and febrile. Her respiratory system examination showed tachypnea with respiratory rate 32 per minute. She was also dyspneic with reduced chest expansion on right side. There was stony dull note on percussion of right hemithorax but normal resonant percussion on left hemithorax. There was reduced breath sound in right hemithorax. There was a non tender swelling in right anterior chest which was firm in consistency and the overlying skin was normal.
Diagnosis and Management: Haematological Investigations revealed Haemoglobin - 10.4 gm%, TLC (total leucocytes count) - 11.5x109 /L and Platelet count- 250,000 platelets per microliter of blood. Biochemical parameters were as follows –RBS (Random Blood Sugar)- 110mg/dl, Liver Function Test (LFT) and Renal Function Test (RFT) were within normal limits. Sputum smear was negative for acid fast bacilli by Ziehl- Neelsen (ZN) staining method. Serology for HIV was negative. Purified Protein Derivative (PPD) test was suggestive of positive induration of 16 mm.
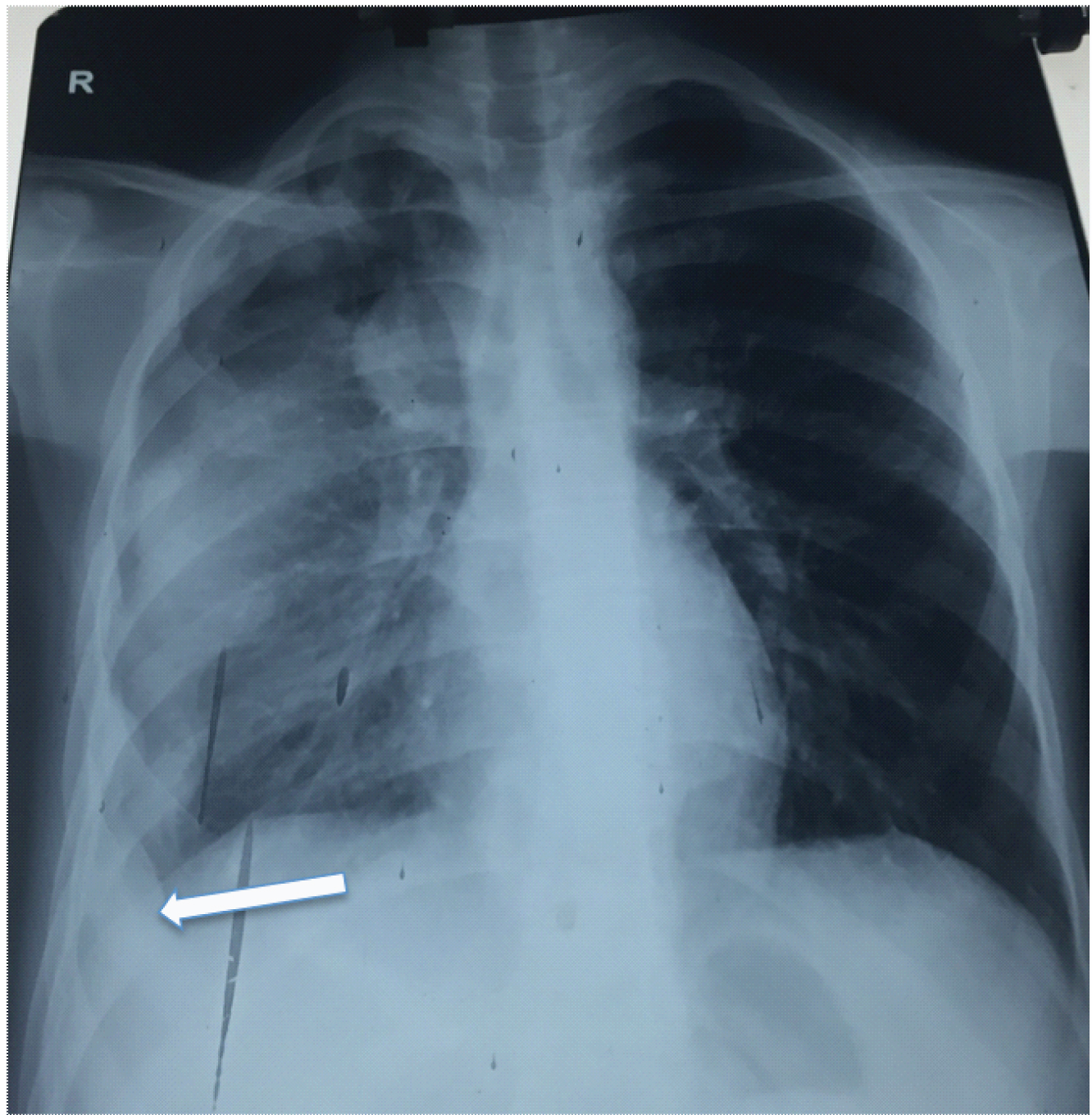
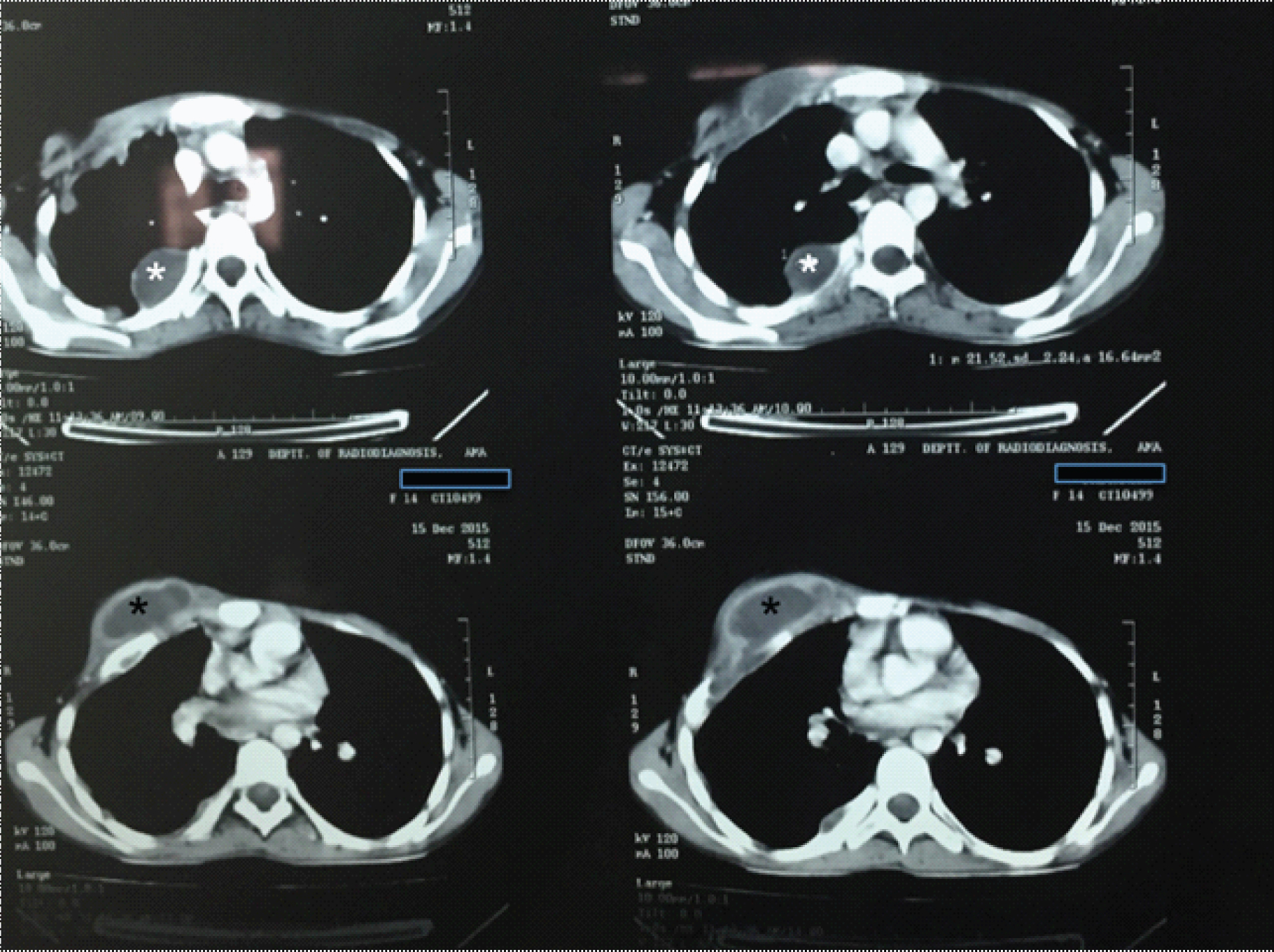
Chest X-ray PA view [Table/Fig-1] revealed a homogenous opacity in right lower zone with obliteration of costophrenic angle and mediastinal shift towards left. Contrast Enhanced Computed Tomography of thorax (CECT thorax, [Table/Fig-2]) confirmed the presence of loculated collection of fluid, attenuation and multiple septations in right pleural cavity. Thickening of overlying pleura causing indentation of underlying lung parenchyma was suggestive of empyema. The collection was seen extending antero-laterally into the muscles of chest wall leading to formation of abscess with the largest measuring 5.5 x 2.5 cm. Mild crowding of ribs was noted on right side. Pleurocentesis was done and pus was aspirated from right pleural cavity and also from anterior chest wall swelling. Both the samples were sent for direct smear and culture sensitivity for AFB and Gram staining. Aspirated pus was also sent for the molecular test Line Probe Assay (LPA). Both pus samples were resistant for rifampicin and isoniazid by LPA. Direct smear from both the samples were positive for AFB. On the basis of LPA report patient was diagnosed as MDR tuberculosis and was put on category four (CAT IV) treatments. CAT IV regimen included Injection kanamycin 75 gm, pyrazinamide 1000 mg, ethambutol 600 mg, ethionamide 750 mg in divided doses, cycloserine 750 mg in divided doses, levofloxacin 750 mg for six months followed by ethambutol, ethionamide, cycloserine and levofloxacin as in their previous doses for next 18 months.
CXR PA view showing homogenous opacity in right hemithorax with obliteration of right costophrenic angle (white arrow).
CECT thorax showing loculated collection of thick fluid attenuation with multiple septation in right pleural cavity (white astrik) with collection which are extending antero-laterally into the muscle of chest wall leading to formation of abscess (5.5x2.5cm) (black astrik).
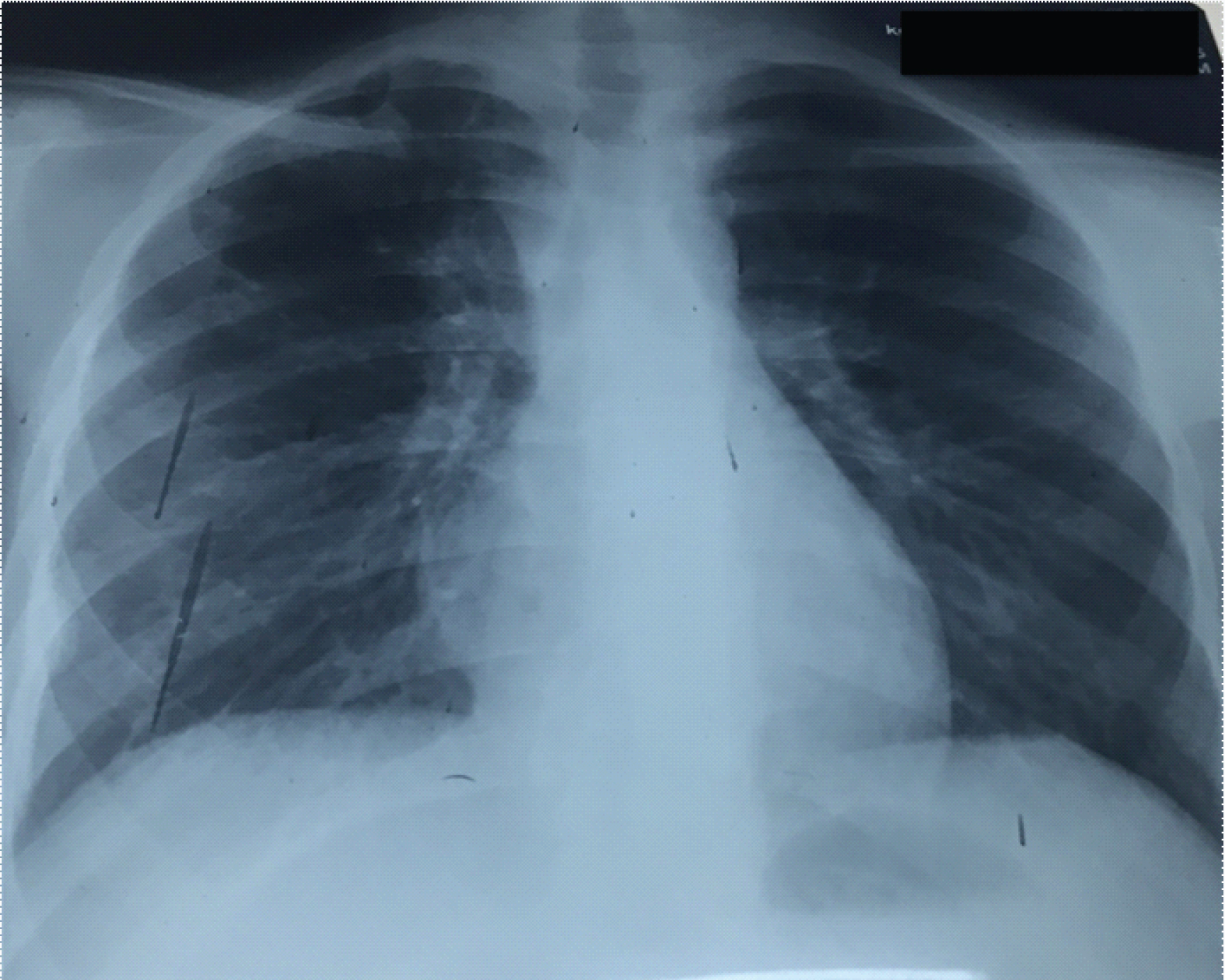
Following initiation of therapy she developed nausea and vomiting that resolved gradually after medication. Patient responded to treatment with resolution of fever, improvement in appetite and reduction in chest pain. She took total 24 months of complete treatment following which she was completely relieved of her symptoms. Her chest X-ray, PA view [Table/Fig-3] also showed radiological improvement.
CXR PA view showing radiological improvement after 24 months of CAT IV treatment, clearing of right costophrenic angle.
Discussion
Global incidence of new cases of tuberculosis is 10.4 million worldwide [1]. Estimated incidence of tuberculosis in India is 2.8 million, of which 480,000 cases are of Multidrug-Resistant TB (MDR-TB) [2]. MDR pulmonary tuberculosis is a grave problem caused by rifampicin or both rifampicin and isoniazide resistant strain of Mycobacterium tuberculosis. A 20% of prior treated cases of tuberculosis and 3.3% of new TB cases are suffering from MDR tuberculosis worldwide [3]. Pulmonary form of MDR tuberculosis is common now-a-days but extrapulmonary primary MDR tuberculosis cases are rare in literature. Extrapulmonary tuberculosis accounts for 20% of all tuberculosis cases even higher upto 50% in immunocompromised HIV individuals worldwide [4]. EN is an infrequent clinical entity and uncommon form of extrapulmonary tuberculosis.
Extrapulmonary Tuberculosis (EPTB) is frequently underdiagnosed because it is difficult to isolate mycobacteria from extrapulmonary specimen. In India, EPTB forms 10-15% of all TB, mostly TB lymphadenitis and pleural effusion [5]. Patients with extrapulmonary manifestations need specialized investigations and the diagnosis is usually based upon clinical, radiographic, molecular or histopathological findings, rather than bacteriologic evidence. Therefore, there are very few reports available on drug susceptibility patterns of EPTB as these patients are usually not included in drug resistance surveys, which focus mainly on pulmonary TB [6]. Empyema may be of traumatic or non traumatic origin [7]. Infection is a leading cause of non traumatic empyema. Upto 60% cases of empyema are associated with pneumonia. EN is an extremely unusual complication of empyema and commonly due to rupture of sub pleural tuberculous caseous foci in 73% of cases; rare causes are due to malignancy, pyogenic lung abscess, blastomycosis. Most common infectious causative organism is Mycobacterium tuberculosis, Actinomycosis, Staphylococcus, pneumococci, E.coli, Klebsiella, Pseudomonas and anaerobic bacteria [8]. Other site of empyema extension include vertebral column, paravertebral soft tissue, retroperitonium, bronchus mediastinum, breast, diaphragm and rarely esophagus, flank, groin and pericardium. Its overall mortality is 66% [9]. This was the rare case seen in our hospital after long time confirming the rarity of the condition. It is also reported to be rare by other workers elsewhere. Akgü l et al., reported only nine cases of EN over a 4-year period in Turkey [10]. Hoffman, in United Kingdom, also reported its rarity where he reported a prevalence of 3.2% [11]. Our patient had empyema and chest wall swelling was present for two months before presenting to the hospital for intervention. If pleural effusion is left untreated for months this can lead to development of EN. This might have contributed to the development of EN in our patient. Lung CT scan is pathognomonic in diagnosing EN. The sign is connection of pleural effusion with extrapleural mass of chest wall. Now till date no case of primary MDR empyema necessitans is reported. Our case is unique because patient was immuno-competent and aetiology for empyema necessitans was primary MDR. Rapid molecular diagnostic methods like Cartridge Based Nucleic Acid Amplification Test (CBNAAT), Line Probe Assay (LPA) are very useful to diagnose cases of extrapulmonary tuberculosis. In our case, with the help of LPA we were able to diagnose primary MDR EN in this young immuno-competent girl. She responded well to a CAT-IV anti-tubercular therapy also. Surgical therapy is usually reserved for chronic empyema (due to late presentation or improper antibiotics), ICD failure, multi-loculated empyema and persistent effusion [12]. Techniques include rib section, decortication, open drainage, VATS and rarely lung resection. Video Assisted Thoracoscopic Surgery (VATS) is newer and less invasive method for removing thickened pleural peels however may be inadequate.
Conclusion
Newer diagnostic methods are very helpful in early diagnosis of extrapulmonary tuberculosis and followed by early initiation of therapy. MDR extrapulmonary cases are increasing now days. EN is a rare form of extrapulmonary tuberculosis. Most of EN cases are pyogenic in origin and for treatment they require antibiotic therapy and surgical management but primary MDR cases of EN are also seen. Second line antitubercular therapy is prime management for primary MDR EN.
[1]. Global tuberculosis control: WHO report 2011. Available from URL: http://whqlibdoc.who.int/publications/2011/ 9789241564380_eng.pdf (Accessed on December 2011) [Google Scholar]
[2]. Gupta DK, Sharma S, Management of empyema—role of a surgeonJ Indian Assoc Pediatr Surg 2005 10:142-46. [Google Scholar]
[3]. Sharma SK, Mohan A, Gupta R, Kumar A, Gupta AK, Singhal VK, Clinical presentation of tuberculosis in patients with AIDS: an Indian experienceIndian J Chest Dis Allied Sci 1997 39:213-20. [Google Scholar]
[4]. Sharma SK, Mohan A, Extrapulmonary tuberculosisIndian J Med Res 2004 120:316-53. [Google Scholar]
[5]. Arora VK, Rajnish G, Trends of EPTB under Revised National TB Control Programme: A study from South DelhiIndian J Tuberc 2006 53:77-83. [Google Scholar]
[6]. Lawn SD, Zumla AI, Diagnosis of extrapulmonary tuberculosis using the Xpert® MTB/RIF assayExpert Review of Anti-Infective Therapy 2012 10(6):631-35. [Google Scholar]
[7]. Brims FJH, Lansley SM, Waterer GW, Lee YCG, Empyema thoracis: new insights into an old diseaseEuropean Respiratory Review 2010 19(117):220-28. [Google Scholar]
[8]. Kono SA, Nauser TD, Contemporary empyema necessitatisAm J Med 2007 120(4):303-05. [Google Scholar]
[9]. Acharya PR, Shah KV, Empyema thoracis: A clinical studyAnnals of Thoracic Medicine 2007 2(1):14-17. [Google Scholar]
[10]. Akgül AG, Örki A, Örki T, Yüksel M, Arman B, Approach to empyema necessitatesWorld Journal of Surgery 2011 35(5):981-84. [Google Scholar]
[11]. Carter E, Waldhausen J, Zhang W, Hoffman L, Redding G, Management of children with empyema: pleural drainage is not always necessaryPediatr Pulmonol 2010 45(5):475-80. [Google Scholar]
[12]. Bailey KA, Bass J, Rubin S, Barrowman N, Empyema management: twelve years’ experience since the introduction of video-assisted thoracoscopic surgeryJ Laparoendosc Adv Surg Tech A 2005 15:338-41. [Google Scholar]