Unilateral Foot Drop: An Unusual Presentation of a more Common Disease
Rameshwar Nath Chaurasia1, Abhishek Pathak2, Vijay Nath Mishra3, Deepika Joshi4
1 Associate Professor, Department of Neurology, Institute of Medical Sciences Banaras, Hindu University, Varanasi, Uttar Pradesh, India.
2 Assistant Professor, Department of Neurology, Institute of Medical Sciences Banaras, Hindu University, Varanasi, Uttar Pradesh, India.
3 Professor, Department of Neurology, Institute of Medical Sciences Banaras, Hindu University, Varanasi, Uttar Pradesh, India.
4 Professor, Department of Neurology, Institute of Medical Sciences Banaras, Hindu University, Varanasi, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rameshwar Nath Chaurasia, Associate Professor, Department of Neurology, Institute of Medical Sciences Banaras, Hindu University, Varanasi-221005, Uttar Pradesh, India.
E-mail: goforrameshwar@gmail.com
An isolated and unilateral foot drop due to intracranial lesion is quite rare. Presenting herein a case of a 14-year-old female who complained of inability to wear and hold slipper in her left foot. Detailed neurological examination revealed left foot dorsiflexion which had 1/5 muscle power along with brisk left ankle reflex. Magnetic resonance imaging of the brain revealed multiple conglomerate inflammatory granulomas in cerebrum and cerebellum, larger one in right parasagittal region with perifocal oedema. Magnetic resonance spectrum was suggestive of tuberculoma. Her chest X-ray chest revealed milliary shadowing. She was put on anti-tubercular drugs, steroid and a prophylactic anti-epileptic drug. The dorsiflexion improved to grade 4/5 after three weeks of treatment. The motor homunculus for foot is located in parasagittal area. Therefore, in patients with foot drop, we must keep high index of suspicion for parasagittal lesions, so that prompt diagnosis and early management can be done to prevent complications and improve the quality of life of patient.
Lower motor neuron, Magnetic resonance imaging, Spastic foot drop, Tuberculoma, Upper motor neuron
Case Report
A 14-year-old female presented with history of difficulty in walking for last three days after left foot drop. She noticed difficulty in her left foot when she was trying to wear shoes go to school. Weakness gradually progressed within next two days so much so that she was unable to hold slipper and clear the ground without tripping by her left foot. There was no history suggestive of weakness in right lower limb, both upper limbs and cranial nerves. She denied any history of backache, radicular pain or trauma, headache, vomiting seizures, hypo pigmented patch, sensory abnormalities and bladder or bowel complaints.
On examination: On detailed neurological examination, her higher mental functions and cranial nerves were normal. At the left ankle, dorsiflexion was grade 1/5 while planti-flexion was grade 5/5 on Medical Research Council (MRC) scale; extensor hallucis longus contraction was grade 1/5. Power at other joints and in rest of the muscle groups was normal. Left ankle reflex was brisk with asymmetry in plantar response in form of equivocal plantar response on left side and normal response on right side. Primary modalities of sensation as well as cortical sensations were normal. There was no cerebellar dysfunction. She had a high stepping gait as evidenced by an abnormal lift of the left lower limb while walking. Examination of the peripheral nerves did not reveal any abnormality and no cutaneous markers were found. Lung fields were clear and auscultation revealed normal sounds.
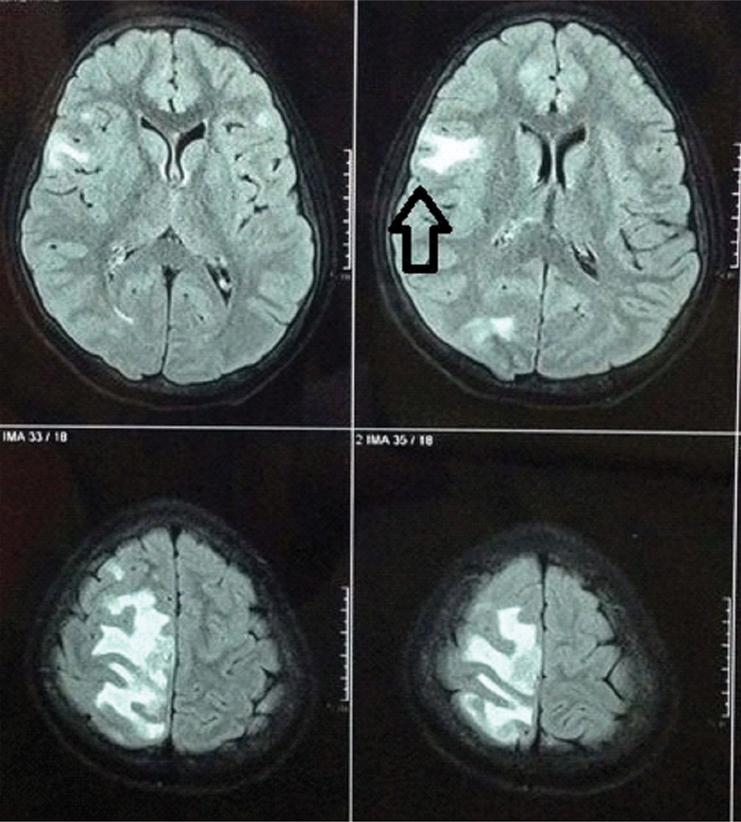
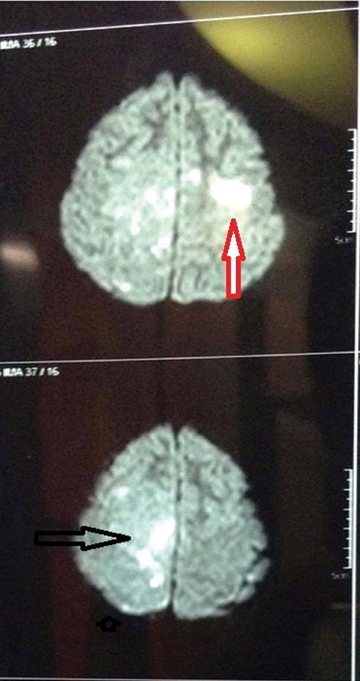
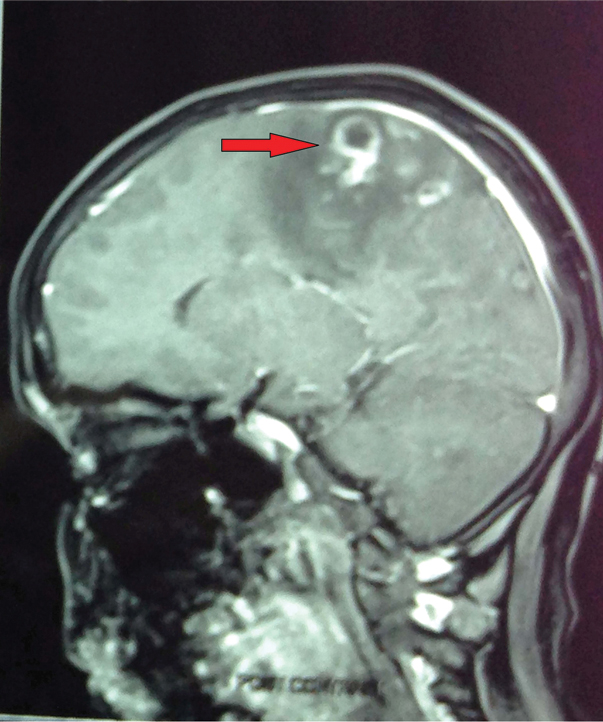
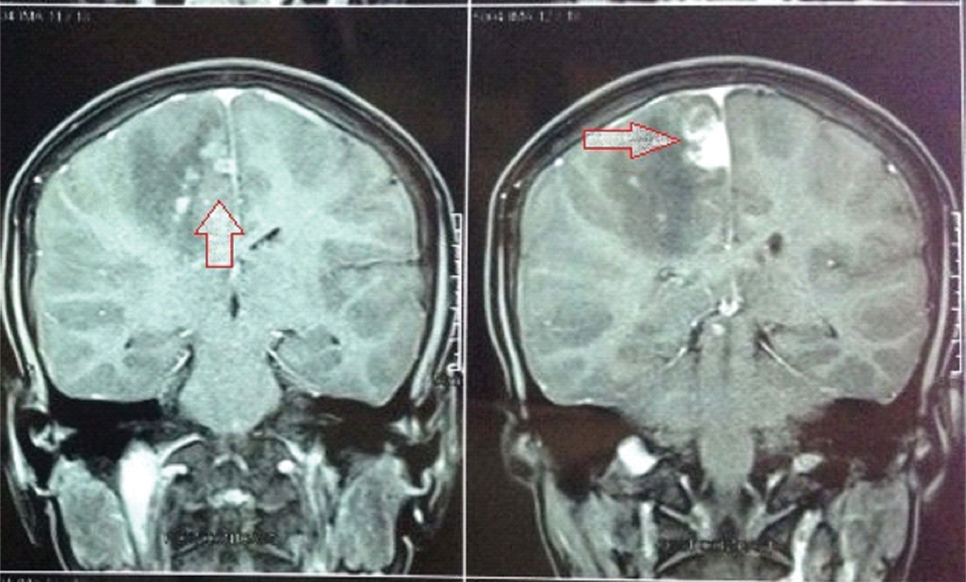
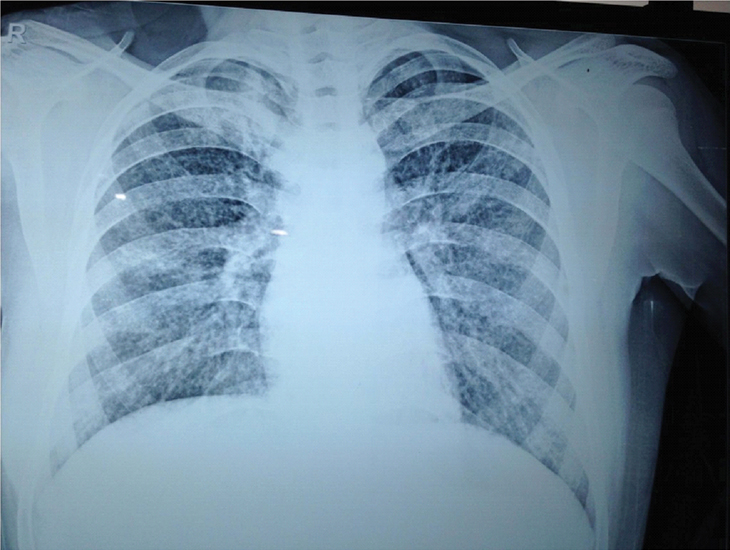
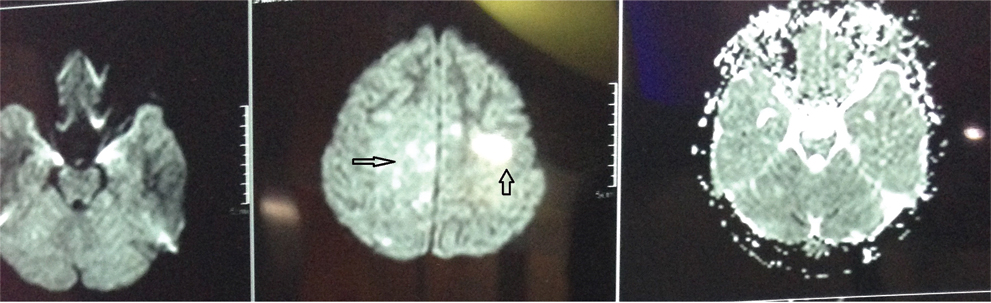
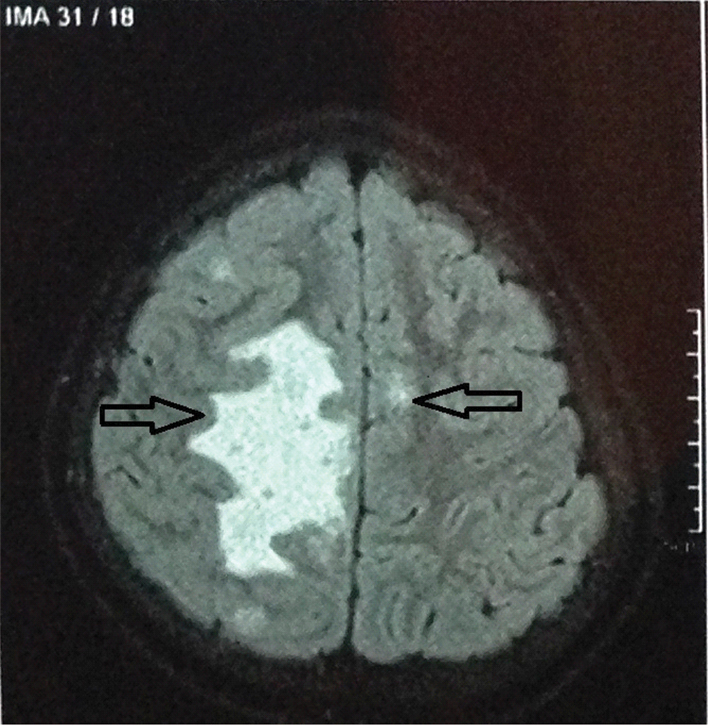
Investigation: Routine haematological investigations (complete blood count, blood sugar, urea/ creatinine) were unremarkable except for raised erythrocyte sedimentation rate (54 mm in first hour). MRI brain and spine was subsequently performed. MRI (1.5 Tesla) of the brain revealed multiple conglomerate inflammatory granulomas in cerebrum and cerebellum, larger one in right parasagittal region with perilesional oedema. Largest granuloma in brain (1.5 cm × 1.4 cm × 2.3 cm), in flair axial sequences showed hyper intensity [Table/Fig-1]. Few lesions in bilateral frontal lobe showed diffusion restriction on DWI [Table/Fig-2]. Sagittal and coronal section of T1 gadolinium contrast sequences revealed these lesions to be hypo intense and had a well-circumscribed thick walled shaggy ring enhancement in right frontal lobe, suggestive of tuberculomas [Table/Fig-3,4]. MR spectroscopy of largest lesion was suggestive of tuberculoma. MRI spine study was normal. X-ray chest was performed to look for any other site for tuberculosis, which revealed milliary shadowing in bilateral lung fields [Table/Fig-5]. As restriction is clear in DWI sequence but it is not so clear in ADC map [Table/Fig-6]. Flair axial image corresponding to [Table/Fig-2] DWI level is shown here [Table/Fig-7].
FLAIR axial sequences of MRI brain showing hyperintense multiple granulomatous lesions (largest one 1.5 x 1.4 x 2.3 cm size) with perilesional oedema in the right precentral gyrus (motor cortex).
Diffusion weighted image showing diffusion restricted granulomatous lesions in bilateral frontal lobes.
Sagittal T1weighted Gadolinium section shows hypo intense and well-circumscribed thick walled saggy ring enhancing granulomatous lesion suggestive of tuberculomas.
Coronal T1weighted Gadolinium Contrast section showing hypo intense and well-circumscribed thick walled saggy ring enhanced granulomatous lesion suggestive of tuberculomas.
X-ray chest PA view showing milliary shadowing bilateral lung fields.
Flair axial image corresponding to Table/Fig-2 DWI level.
Treatment: Patient was put on standard dose of four anti-tubercular drugs (rifampicine, isoniazid, pyrazinamide and ethambutol), prednisolone 1 mg/kg and prophylactic anti-epileptic drug (levetiracetam 20 mg/kg).
Outcome and follow up: The dorsiflexion of her foot improved up-to grade 4/5 after three weeks of treatment. Seven weeks later she developed one episode of focal seizure with secondary generalisation which was treated with antiepileptic drug (levetiracetam 20 mg/kg in two divided doses. She again developed 2-3 episodes of seizure after a period of three weeks, for which dose of levetiracetam was increased to 30 mg/kg in two divided doses and seizure was controlled. She is doing fine in follow up till now.
Discussion
Foot drop can develop from weakness of the dorsiflexors and extensor muscles of the foot. This weakness is caused by either an upper or lower motor neuron injury most commonly by later, either L5 radiculopathy or peroneal nerve injury [1]. Other lower motor neuron lesions causing foot drop include sciatic mononeuropathy, lumbosacral plexopathy, polyneuropathy, or a severe L5 radiculopathy [2]. Anecdotal cases of foot drop with intracranial inflammatory granuloma as the prime cause have been reported [3,4]. Sometimes detailed history and neurological examination can give clues to suspect and promptly diagnose a central lesion. The usual causes of foot-drop are common peroneal nerve entrapment at the fibular head and lower lumbar disc prolapse with nerve root compression. Hansen’s disease must also be kept in mind while encountering such cases, in a tropical country like India. Spastic foot drop or central (intracranial/upper motor neuron) causes for foot drop is due to involvement of the parasagittal precentral (motor) gyrus representing the leg area [5,6]. Other intracranial or central causes of foot drop such as high-grade glioma, parasagittal meningioma and granulomatous lesions including tuberculoma have been described previously in literature [7-9]. This case represents a rare and unusual presentation of relatively common central nervous system infection. Important clinical examination findings in the form of pure motor weakness, brisk left ankle jerk and asymmetrical plantar response were the reasons to go directly for MRI brain study. Findings were incompatible with peripheral neuropathy and spinal cord lesions.
Conclusion
Intracranial cause of isolated unilateral foot drop is extremely rare. Delay or misdiagnosis of such cases may lead to unnecessary investigations and interventions. Missing signs of upper motor neuron (UMN) lesions, in the initial examination may delay or misdiagnose case.
[1]. Stewart JD, Foot drop: where, why and what to do?Pract Neurol 2008 8:158-69. [Google Scholar]
[2]. Katirji MB, Wilbourn AJ, Common peroneal mononeuropathy: a clinical and electrophysiologic study of 116 lesionsNeurology 1988 38(11):1723-28. [Google Scholar]
[3]. Panda AK, Intracranial tuberculoma in motor cortex: a central cause of isolated unilateral foot dropBMJ Case Rep 2013 2013:Pii:bcr-2013-010285 [Google Scholar]
[4]. Sahu R, Garg RK, Malhotra HS, Lalla R, Spastic foot-drop as an isolated manifestation of neurocysticercosisBMJ Case Rep 2012 2012:Pii:bcr-2012-006795 [Google Scholar]
[5]. Guthrie BL, Ebersold MJ, Scheithauer BW, Neoplasms of the intracranial meninges. In: Youmans ER, (Ed.)Neurological Surgery 1990 PhiladelphiaWB Saunders:3250-315. [Google Scholar]
[6]. Ozdemir N, Citak G, Acar UD, Spastic foot drop caused by a brain tumour: a case reportBr J Neurosurg 2004 18:314-15. [Google Scholar]
[7]. Wilbers J, Idema A, Gijtenbeek A, A bilateral foot drop due to neuroschistosomiasisJ Neurol 2010 257:853-55. [Google Scholar]
[8]. Lath R, Rajshekhar V, Unilateral foot dropPostgrad Med J 1996 72:573-74. [Google Scholar]
[9]. Goia E, Hamilton L, Chan J, Wei X-C, Mah JK, Rho JM, Unilateral foot drop as an initial presentation of a brain tumor in a childJ Child Neurol 2013 29:955-58. [Google Scholar]