Osteoarthritis is complicated by different types of degenerative changes including osteophyte formation on spinal vertebral bodies. Osteophytes or bony spurs are defined as abnormal bony growths or projections formed along the intervertebral joints. Although vertebral osteophytes are considered as a common finding in the cadaveric anatomy. More importantly, vertebral osteophytes are reported as a common radiological finding affecting 20–30% of the elderly population [1]. Studies indicate that the risk of development of osteophytes in the vertebral column increases with the age [2]. Cvijetic et al., found that 21.3% of men and 23.9% of women over 45 years of age had osteophytes on the lumbar spine [3]. The observations of Pye et al., depicted that when the mean age is 65 years of age, 73% of men and women had evidence of lumbar osteophytes [4].
The appearance of lumbar osteophytes might result in medical problems and can remain unnoticed without any adverse effects. Though important, its real significance is yet far from clear. On literature review, it was found that cadaveric studies of lumbar osteophytes are scanty and there are no reports on the histopathology of these osteophytes. Hence, a detailed morphometric and histological study of lumbar osteophytes was conducted in the cadaveric vertebral spines to understand the frequency of their occurrence and distribution.
Materials and methods
During routine cadaveric dissections for medical students, the presence of lumbar osteophytes in dissected specimens was noticed. This was an observational study in which, frequency of occurrence of lumbar osteophytes in 40 male cadavers of South Indian origin over a period of four years i.e., from March 2013 to February 2017 were examined. The cadavers were obtained from the Department of Anatomy. The approximate age of the cadavers ranged from 55-80 years. Vertebral columns with no signs of trauma, congenital anomalies were included in the study. Any vertebral column which had deformity, signs of trauma, general widespread bone disease, or local disease of vertebral column were excluded from the study. Osteophytes were considered to be present if a bony protrusion bigger than 5mm was observed on the vertebra. Each lumbar vertebra was examined in the specimen. Osteophytes were diagnosed when bony outgrowths developed on the margins of vertebral bodies. The lumbar part of the vertebral column was dissected and cleaned. The soft tissue was removed. When osteophytes were found to be present, their vertebral level, exact distribution on the vertebral body, its vertical and transverse diameters in centimeters were recorded using a scale. The procured data was compiled, organized, and analysed by using percentage statistics. The results obtained were represented as tables using Microsoft Office 2016. A small piece of the osteophyte was removed and preserved in 10% formalin. It was processed for histopathological examination without decalcification. The sections were stained with routine Haematoxylin & Eosin (H&E) stains and examined under the microscope using different magnifications for histopathological studies and photographs were taken.
Results
Gross Anatomy Findings
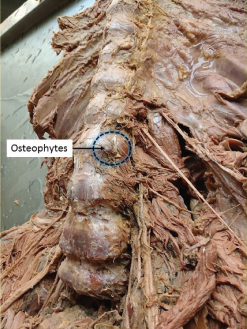
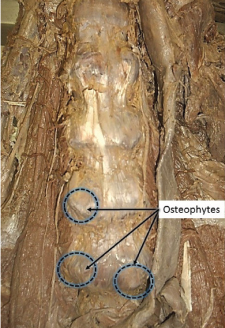
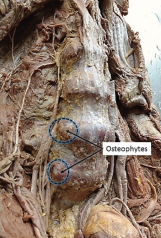
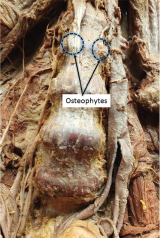
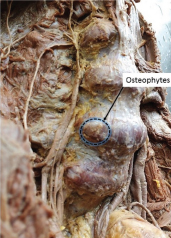
Out of the 40 specimens studied, the occurrence of osteophytes was seen in 4 lumbar vertebral column (10%). Detailed morphometric measurements of these osteophytes, with their vertebral levels and distribution is shown in [Table/Fig-1]. All osteophytes were present on the anterolateral or lateral side of the vertebral bodies near the intervertebral discs. It was noticed that the osteophytes occcured mostly on the right side of the vertebral bodies than the left side (5 on right side, 3 on left side of vertebra). Photographs of the lumbar vertebral column showing the presence of osteophytes at different vertebral level are shown in figures [Table/Fig-2,3,4,5 and 6].
Table is showing the occurrence and distribution of lumbar osteophytes and their detailed morphometric measurements.
| Specimen number | Position | Vertebral level | Morphometric measurements |
|---|
| 1 (osteophytes: 2) | Right and left, anterolateral side of vertebral body | L2 (Bilateral) | Right: Vertical= 2.5 cmTransverse= 2.5 cmLeft: Vertical= 2.5 cmTransverse= 3 cm |
| 2 (osteophytes: 2) | Right and left, anterolateral sideof vertebral body | L3 (Bilateral) | Right: Vertical= 1.4 cmTransverse= 1.5 cmLeft: Vertical= 1.6 cmTransverse= 2 cm |
| 3 (osteophytes:1) | Right, lateral sideof vertebral body | L4 | Vertical=3.8 cmTransverse= 3 cm |
| 4 (osteophytes: 3) | Right, lateral sideof vertebral bodyRight and left, anterolateral sideof vertebral body | L4L5 (Bilateral) | Vertical=3.8 cmTransverse= 3 cmRight: Vertical= 2.5 cmTransverse= 2.5 cmLeft: Vertical= 2.5 cmTransverse= 3 cm |
Dissection of the lumbar vertebral column showing osteophyte growth at the level of L3 vertebra (highlighting left side).
Dissection of the lumbar vertebral column showing osteophyte growth at the level of L4 (right - unilateral) and L5 vertebrae (bilateral).
Dissection of the lumbar vertebral column showing osteophyte growth at the level of L4 and L5 vertebrae (highlighting right side).
Dissection of the lumbar vertebral column showing osteophyte growth at the level of L2 vertebrae (bilateral).
Dissection of the lumbar vertebral column showing osteophyte growth at the level of L4 (right).
Histological Findings
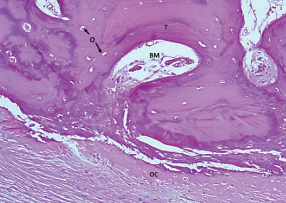
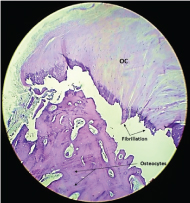
The H&E stained sections of the osteophytes showed features which resembled a cancellous bone. Sections show fragment of degenerative osteophytic cartilage with the foci showing fibrillation overlying trabecular bone enclosing fatty marrow spaces containing haematopoietic elements. There was no evidence of granuloma in any of the sections studied [Table/Fig-7,8].
Photograph showing the section of osteophyte growth stained with H&E stain. The section shows the degenerative osteophytic cartilage fragments (OC) in the background of trabeculae (T) of osteocytes (O) enclosing fatty bone marrow (BM). (Magnification: 20X).
Low magnification (10X) view of H&E stained section of osteophytes, showing the fragment of degenerative osteophytic cartilages (OC) with fibrillation overlying the trabecular bone.
Discussion
Osteophytes are outgrowths on the vertebral columns. It is a common change that occurs with age and closely resembles the process of chondrogenesis and endochondral bone formation. This fact was evident in the histological analysis of osteophyte done in the present study wherein, a layer of osteophytic cartilage capping the trabecular bone was noted, which is an indication of endochondral ossification. The pathogenesis of osteophytes begins with the degeneration of the vertebral column precisely, the nucleus pulposus [5]. As one ages, the nucleus pulposus loses its aqueous content, resulting in decreased height of the intervertebral disc and less resiliency to load-bearing weight. Alongside, the annulus fibrosus also begins to lose elasticity. To maintain maximal load-bearing potential, the margins of the zygapophyseal joint form bony projections to increase the surface area for weight distribution. This results in the formation of bony protrusion called osteophytes from the vertebral body [6]. There are many theories regarding the formation of osteophytes. Schmorl G et al., formulated a pathogenic hypothesis that because of tears in the attachment of the annulus fibrosus, the nucleus pulposus protrudes forward against the anterior longitudinal ligament. The increased strain causes the formation of spurs on the vertebral bodies (Schmorl’s rim lesion theory) [7]. Collins formulated a theory of osteophyte formation that associates degeneration of the entire intervertebral disc and the resultant anterior protrusion with subsequent osteophyte formation. The protrusion of the disc lifts the periosteum lateral to anterior longitudinal ligament and stimulates new subperiosteal bone (Collins’ bulging disc theory) [8]. According to Macnab’s theory, osteophytes are formed as a result of instability between adjacent vertebral bodies (Macnab’s instability theory) [9].
Kasai et al., in their clinical study on anterior lumbar vertebral osteophytes, distributed the osteophytes into six groups based on the direction of extension of each pair of osteophytes across the intervertebral disc space: Group A, no osteophytes; Group B, the pair of osteophytes extended in the direction of the adjacent disc; Group C, there was almost complete bone bridge formation by a pair of osteophytes across the intervertebral disc space; Group D, the pair of osteophytes extended in a direction away from the adjacent disc; Group E, the osteophytes extended nearly horizontally to the vertebral body border without closing the intervertebral disc space; and Group F, ungroupable [10]. The anterolateral osteophytes noticed in the present study falls into Group B osteophytes of the above classification wherein the osteophytes extended in the direction of the disc space.
Occurrence of lumbar osteophytes is clinically important. Studies have shown a significant association between increased anterior lumbar osteophytes and prevalence of abdominal aortic calcification [11]. The presence of calcified lesions in the abdominal aorta has been associated with cardiovascular morbidity and mortality [12]. The present study found anterior and lateral osteophytes in greater numbers. These osteophytes can pressurize the abdominal aorta or inferior vena cava wall leading to ischemia or perforation. The close proximity of the abdominal aorta and inferior vena cava to the lumbar part of vertebral column is attributed to the pathological findings in such cases. Due to this lumbar osteophytes have also been associated with inferior vena cava obstruction [13]. Posterior lumbar osteophytes when presented may contribute to lumbar stenosis. Postero-lateral osteophytes can compress lumbar spinal nerve roots causing back and leg pain [14]. Osteophyte-induced nerve root compression is a common clinical scenario in recent years. In a study by Matsumoto et al., found 6 out of 7 cadavers with osteophytes on the vertebral bodies of L5 and S1, which entrapped the L5 nerve in the lumbosacral tunnel [15]. However, entrapment of nerve by osteophytes was not found in the present study but the impingement by osteophytes should be kept in mind by the clinicians treating patients who have definite L5 radiculopathy.
Study of osteophytes is also important to anthropologists because it is hypothesized that skeletal osteophyte findings can be used for age-at-death estimations [16]. The occurrence of vertebral osteophytes is an enigma to anatomists, clinicians, anthropologists, and radiologists. Hence, further research will be required to investigate the osteophyte development, the mechanisms underlying osteophyte formation and its molecular characterization.
Future studies can be focused on exploring prevalence of osteophytes in cervical and thoracic region of the vertebral column. Further evaluation using radiological means can be studied in clinically relevant cases in association with gross anatomical specimens. Using special stains for glycosaminoglycans, composition of osteophytes can be explored in detail which might give full explanation of the factors contributing to vertebral osteophyte development.
Limitation
Limitation of the study were inadequate sample size and comparison using an appropriate statistical test under age /gender distribution and bilateral occurrence of osteophytes could not be assessed.
Conclusion
In current study lumbar osteophytes were found in 10% of the specimens studied. Histological analysis of the osteophytes showed fragments of degenerative osteophytic cartilage layer capping the trabecular bone, which is an indication that osteophytes develop through endochondral ossification. These cadaveric reports deserve further attention given their potential clinical implications. Knowledge regarding occurrence and incidence of osteophytes is essential to understand for the management of common degenerative changes of the vertebral column.