The infections of the genital tract are most commonly seen in women of reproductive age group; which in many cases remain asympt-omatic. Commonly detected pathologic flora includes Trichomonas vaginalis, Gardnerella vaginalis, Actinomyces, Candida albicans and Human Papilloma virus [1].
Infections incited by micro-organisms in the female genital tract are associated with cytopathic effects. Additionally, an inflammatory response at the affected site is invariably present; these changes maybe of diagnostic importance [2]. After an extensive study of the relationship between inflammatory cervical smears and malignancies, it has been reported that the underlying infections could mask cancerous and precancerous changes and also prevent the detection of certain invasive cervical squamous cell carcinomas [3].
In the reproductive age group, genital infections could also pose a risk if left untreated, to the baby before and during childbirth [4,5]. Further, the significance and incidence of pathogenic flora in post-menopausal women as compared to the women in the reproductive age group, has not been extensively reported.
Papanicolaou test is a quick and painless procedure to retrieve the cells from the uterine cervix and is used for the detection of cervical abnormalities and precancerous dysplastic changes, thus serving as a screening test for the prevention of uterine cancer [1]. It can also detect infections of the uterus, which could often be precursors to malignancy.
The current Bethesda system of reporting Pap smears are specifically designed to identify such precursor lesions or even a frank malignancy. The same reporting system also underlines the importance of stating the findings in the report, along with a provision for microbial and parasitic infections [3].
If a precise diagnosis is made, the treatment is rendered relatively easy and early. As it is the most cost effective modality of inves-tigation for cervical pathology, the suitability of Papanicolaou Smear for the detection of the common vaginal infections should be determined.
This study seeks to measure the role of Papanicolaou smear in detection of pathologic flora: Candida albicans, Gardnerella vaginalis, Trichomonas vaginalis, HPV, HHV and Actinomyces; in a rural health care set up amongst women in the reproductive and menopausal age group.
Materials and Methods
The present retrospective study was conducted in the Department of Pathology, Kasturba Medical College, Manipal after obtaining the requisite Institutional Ethical Clearance. The study was completed in a time period of 14 months (July 2015-Sept 2016). An informed consent was obtained from the study participants following which the participants were subjected to a Pap smear test.
The test was carried out after visualizing the cervix using a sterile Cusco’s speculum and inserting a wooden spatula into the cervical os. Spatula was rotated thrice keeping the shoulder of the spatula in contact with the ecto-cervix thereby ensuring that the squamo-columnar junction is being sampled for Pap smear. Spatula was then wiped on one end of a labeled slide, which was fixed. After drying, the slide was sent immediately to the pathology laboratory for examination.
Expecting the isolation of the pathogen in 60% of asymptomatic women, with a relative precision of 15% at 5% level of confidence, the calculated minimum sample size was determined to be 150.
All asymptomatic women above 20 were not lactating or pregnant and have not had hysterectomies performed, were involved. Only smears with adequate cellularity were considered for the study. The participants on medication for gynaecological complications, women under 20 years of age, and the smears showing epithelial abnormalities and inadequate sampling were excluded from the study.
Cervical/vaginal smears were stained using the Papanicolaou stain and studied by 2 independent pathologists, with the senior cytopathologist reviewing the same.
Statistic Analysis
A descriptive statistical analysis was used for the present study with relative frequencies of the variables included.
Results
Of the total of 150 samples examined, Candida species was the most frequently detected (8.7 %) followed by Trichomonas vaginalis (5.3%) and Gardnerella vaginalis species (4.7%) [Table/Fig-1].
Frequency distribution of various infections on the Pap smear.
| Organism | Frequency | Percentage |
|---|
| Candida sp. | Present: 13 | 8.7 |
| Absent: 134 | 89.3 |
| Inadequate: 3 | 2 |
| Trichomonas vaginalis. | Present: 8 | 5.3 |
| Absent: 139 | 92.7 |
| Inadequate: 3 | 2 |
| Gardnerella vaginalis | Present: 7 | 4.7 |
| Absent: 140 | 93.3 |
| Inadequate: 3 | 2 |
| Actinomyces sp. | Present: 1 | 0.7 |
| Absent: 146 | 97.3 |
| Inadequate: 3 | 2 |
| HPV | Present: 3 | 2 |
| Absent: 144 | 96 |
| Inadequate: 3 | 2 |
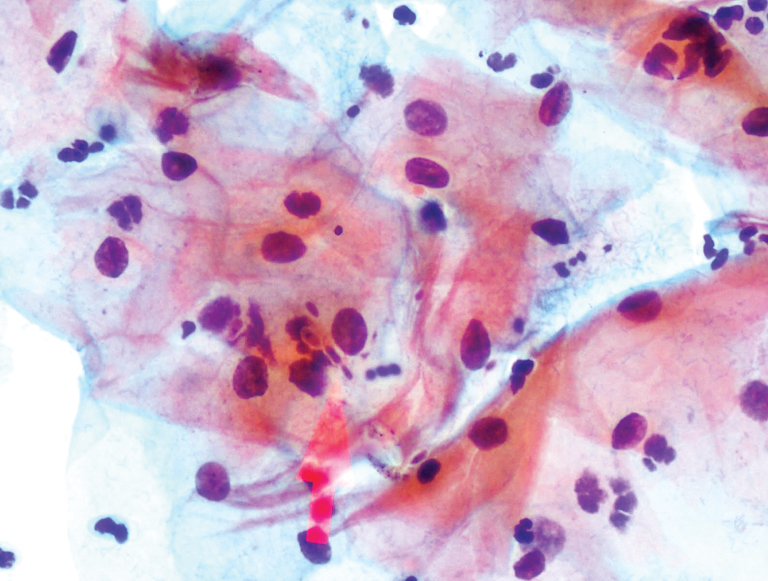
Candidal infection was characterized by alteration in the normal flora, a moderate to heavy neutrophilic infiltrate and variably distributed histiocytic infiltrates. The pseudohyphal forms were more numerous as compared to the spores [Table/Fig-2].
Pap smear showing yeast-like forms and pseudohyphae of Candida (arrow) species with variable surrounding inflammation. (Pap; 40X).
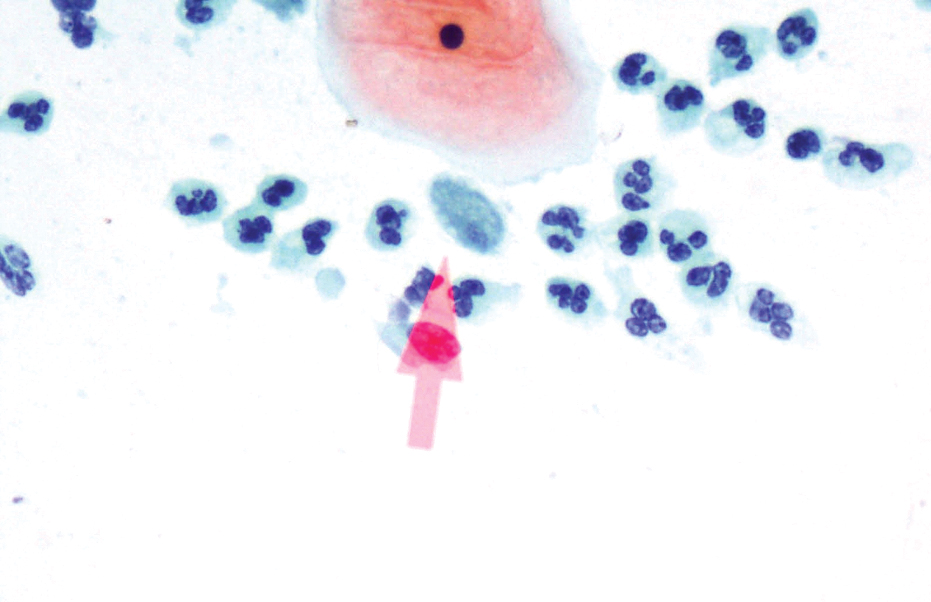
Trichomonas vaginalis infections were characterized by trophozoite forms and a background of moderate to heavy inflammatory exudate comprising chiefly of neutrophils, lymphoplasmacytes and few histiocytes. The surrounding flora also showed a variation to coccobacilli forms [Table/Fig-3].
Pap smear shows trophozoite forms of Trichomonas vaginalis species (arrow) with background altered flora. (Papanicolau; x400).
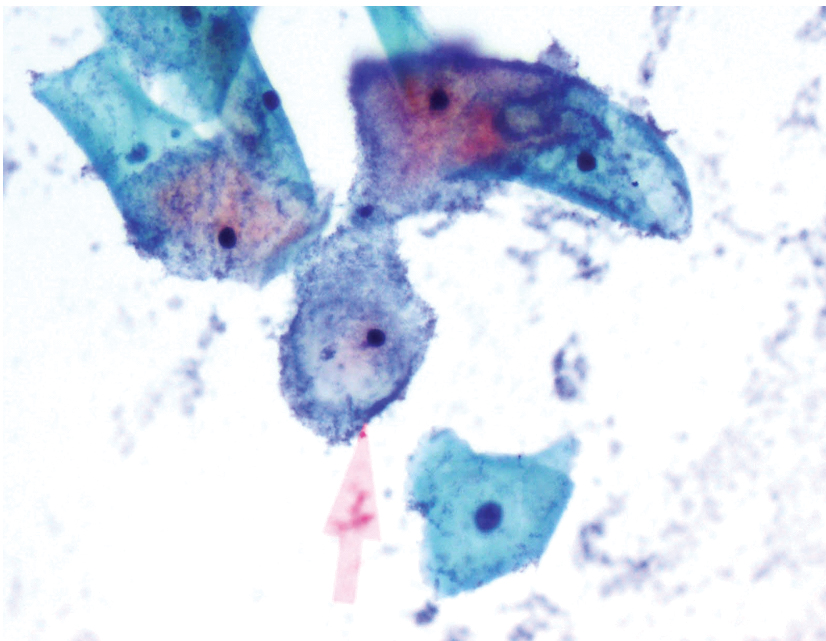
Gardnerella vaginalis infections were characterised by appearance of ‘clue cells’; composed of keratinocytes with studded coccobacillary forms and a background showing mild to moderate inflammation [Table/Fig-4]. In some instances, the background was clear, lacking inflammatory cells.
Pap smear showing clue cells in Gardnerella vaginalis. (arrow) (Pap; 40X).
HPV-induced changes were noted in a mere 2% of cases in the form of nuclear contortions and perinuclear halos (cumulatively referred to as koilocytic changes). However, a serologic/virologic testing of the same was not done. Actinomyces species was noted in less than 1% of cases.
Discussion
Despite being curable, vaginal infections continue to be a major health issue in most developing countries. Over 50% of those suffering from these infections are asymptomatic, making their detection and diagnosis difficult. Lack of awareness, low literacy rates and socioeconomic status, limited resources, poor personal hygiene and associated social stigma leading to poor attendance at Reproductive Tract Infection/Sexually Transmitted Disease clinics, are other factors adding to the depth of the problem among rural woman [6].
If an early and precise diagnosis is made, the treatment follows easily. Because of its success of cytological screening for cervical cancer, most countries including India have adopted Pap smear to become a routine procedure for women in reproductive and post-menopausal age groups. As it is a most cost-effective modality of investigation for cervical pathology, the suitability of Papanicolaou Smear for the detection of the common vaginal infections has constantly been under the scanner.
Increasing evidence points towards Gardnerella vaginalis as the key causative organism of bacterial vaginosis [1]. Although culture studies are renowned as the gold standard method for diagnosis for most bacterial infections, this does not hold true for bacterial vaginosis as the organisms constitute a part of the normal vaginal flora. According to various studies, 50-75% of women with bacterial vaginosis are asymptomatic [6-8]. This has led to a large number of cases being underdiagnosed. However, an association with many obstetric and gynaecological complications such as preterm labour, premature rupture of membranes, chorioamnionitis, postpartum endometritis and an increased risk of late miscarriages has rendered an early detection of this infection pertinent [4,5]. In a meta-analysis of five randomized trials of asymptomatic women with bacterial vaginosis at <22 weeks of gestation treated with clindamycin or placebo/no treatment, clindamycin therapy was associated with a reduction in preterm birth (3.7% versus 6.2%) and late miscarriage (0.3% versus 1.9%) [9].
Detecting bacterial vaginosis in Pap smears may not only help prevent complications in selected asymptomatic women by initiating timely treatment, but can also be an indication to avoid any further diagnostic investigations [2]. Studies have also shown that treatment of bacterial vaginosis may also reduce the risk of acquiring sexually transmitted diseases like human immunodeficiency virus [10,11].
Bacterial vaginosis is usually diagnosed according to the clinical criteria or microbiological tests. According to a study that used Gram stain for the diagnosis of bacterial vaginosis as the standard, Pap smear results had sensitivity of 43.1%, specificity of 93.6%, positive predictive value of 73.8%, negative predictive value of 79.8%, and diagnostic value of 78.8% for the diagnosis of bacterial vaginosis. Because of its high specificity, it may serve as adequate diagnostic criteria when it is positive [11].
Schnadig, et al., reported that Pap smears were more accurate than wet preparations for identifying clue cell and that there’s a high correlation between Pap smears and Gram smears for the diagnosis of bacterial vaginosis [12]. According to Platz-Christensen et al., detection of clue cells in Pap smears showed a sensitivity of 90% and a specificity of 97% when compared with clinical diagnosis of bacterial vaginosis [13]. Out of the 150 asymptomatic women we examined, excluding the 2% of inadequate sample obtained, 4.7% of them showed the presence Gardnerella on the pap smear.
Trichomonas vaginalis, Gardnerella vaginalis, and Candidaalbicans are responsible for 90% of vaginitis [12,14]. In a study held among Iranian women, 2511 out of 33600 (7.5%) cases had vaginal infections. 0.2%, 6.7%, and 0.6% of subjects were infected by T. vaginalis, Candida, and Gardnerella, respectively [15]. The findings of the present study by and large conform to this finding. Another study held among women in a prison in Brazil, demonstrated that T. vaginalis, Candida and Gardnerella were respectively found in 12%, 5.8%, and 21.8% of all the pap smears examined [16]. On studying 20,356 cases in Brazil using Papanicolaou smear, Adad et al., found that low and high indices of infections belong to Trichomoniasis (3.4%) and candidiasis (22.5%) [17].
Trichomonas vaginalis is a protozoan pathogen of the human urogenital tract. The prevalence of Trichomonas vaginalis has been reported to be as high as 26% among female patients. In infected female patients, the symptoms range from vaginal discharge and pruritis to dysuria and dyspareunia [18]. Our study matched this clinical profile. The classical green, frothy, foul-smelling discharge is documented in a mere 10% of the women. Surprisingly, over 50% of the infected patients are asymptomatic [15]. This poses diagnostic challenges and hence, a larger and pivotal role for the Pap smears. Additionally, trichomoniasis is also reported to be contributory in cervical neoplasia, postoperative infections and adverse pregnancy outcomes, pelvic inflammatory diseases and rarely, even in infertility [15]. The presence of T. vaginalis in the vagina increases predisposition to HIV sero-conversion [17]. In the present study, the prevalence of Trichomonas species as detected by Pap smear was 5.3%, which is in alignment with most afore-mentioned literature.
Human Papilloma Virus is the most important causative agent of cervical cancer. Despite the prevalence of pap smear for over half a century, cervical cancer continues to remain a leading cause of death among women [18]. Our study reported a prevalence of HPV of 2%. LO Sarian et al., evaluated the cervix using a visual inspection method with acetic acid (VIA), Lugol’s iodine, cervical cytology and HPV testing as cervical screening tools. Overall test positivity was 11.6% for VIA, 23.0% for VILI, 2.2% for Pap smear (LSIL threshold), 1.1% for Pap smear (HSIL threshold) and 17.1% for Hybrid Capture II [6], They reported that a combined use of VIA or VILI with the Pap test or Hybrid Capture II would allow a specific detection of cervical abnormalities [19]. Another study that compared Human Papillomavirus DNA versus Papanicolaou smears as screening tests for cervical cancer reported that HPV testing was more sensitive (39.2% difference) and only 2.7% less specific than Pap testing. However, for women who get screened less frequently that required, they recommended a more sensitive test like HPV testing [19].
Actinomyces-like organisms rarely appear on routine PAP smears. Our study showed a prevalence of 0.7%. Out of 9,080 women reviewed, Güdücü et al., reported only 33.5%, 30.4%, 43.3%, and 0% of patients with bacterial vaginosis, Trichomonas vaginalis, Candida and Actinomyces, respectively on pap smear [10]. A study conducted to compare PCR, culturing and Pap smear microscopy for the diagnosis of genital Actinomyces reported culture and Pap smear to have low sensitivity which is probably, also the reason for the low prevalence in our study. They reported PCR analysis to be highly sensitive and specific for the identification of clinical Actinomyces [18].
Limitation
We concentrated on a well-defined age group: perimenopausal and menopause. Also, since this study only involved subjects who consented to be part of the project, the non-participants could not be profiled. Additionally, the serologic/virologic testing of HPV was also not done in this study.
The omission of dysplastic conditions from the study group also limited the association between the infection and pre-neoplastic conditions. Also, the hormonal status of all the patients was not available due to a lack of documentation. Hence, an association between the hormonal status and cervical infection could not be evaluated.
Conclusion
The Papanicolaou test for examining cervical smear was found to be useful in detecting vaginal microorganisms. Candidaalbicans species was the most frequently detected; followed by Trichomonas vaginalis and Gardnerella vaginalis. HPV and Actinomyces species were seldom noted. Despite its limitations, the Pap smear is cost-effective, quick and acceptable to most women. Therefore, this method maybe used in rural health care set up as one test can solve two problems.
If similar studies are carried out involving a more diverse group of participants, it has a potential to yield more encouraging results. It also may uncover much rarer causative organisms which may or may not have a role in carcinogenesis.