Amyand’s Hernia – Vermiform Appendix in an Inguinal Hernia: A Rare Finding
Prakash Kumar Sahoo1, Suman Saurav Rout2, Abhijit Samal3
1 Professor, Department of General Surgery, Institute of Medical Sciences and SUM Hospital, Bhubaneswar, Odisha, India.
2 Postgraduate Trainee, Department of General Surgery, Institute of Medical Sciences and SUM Hospital, Bhubaneswar, Odisha, India.
3 Postgraduate Trainee, Department of General Surgery, Institute of Medical Sciences and SUM Hospital, Bhubaneswar, Odisha, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Prakash Kumar Sahoo, SB-66, Aditya Enclave, Kanan Vihar, Phase II, Patia, Bhubaneswar-751031, Odisha, India.
E-mail: drpksahoo2003@yahoo.co.in
A variety of surprises may spring up when the sac is opened in an inguinal hernia. Omentum, bowel diverticulum, ovary, fallopian tube, urinary bladder, large bowel, Meckel’s diverticulum or foreign bodies being the varied contents of a hernia sac. The presence of vermiform appendix in the hernia sac in an inguinal hernia is a rare finding. This condition has been named as “Amyand’s Hernia” in the honour of an English surgeon, Claudius Amyand. A diagnosis preoperatively is difficult and is most often made intraoperatively.
We report here a 52-year-old patient who presented with acute intestinal obstruction due to an obstructed right sided inguinal hernia. A diagnosis of Amyand’s hernia was confirmed when on exploration appendix along with a part of ascending colon was found to be content of the sac along with a few loops of small bowel. The contents were reduced after checking the viability and Bassini’s repair was done. The patient had an uneventful postoperative period.
Appendicectomy, Bassini’s repair, Basson, Losanoff
Case Report
A 52-year-old male patient who presented with a right sided inguinoscrotal swelling along with features of acute intestinal obstruction. On physical examination, the patient was found to have right inguinal hernia which was obstructed with features of acute intestinal obstruction. The laboratory investigations revealed a TLC of 13200/cumm, Na+-130 mEq/L, K+-3.3 mEq/L, Urea–23 mg/dl, Cr–0.7 mg/dl. Patient was resuscitated with IV fluids and IV antibiotics and was taken up for emergency surgery. On USG Abdomen, a blind ended tubular structure with increased vascularity was seen in the hernial sac.
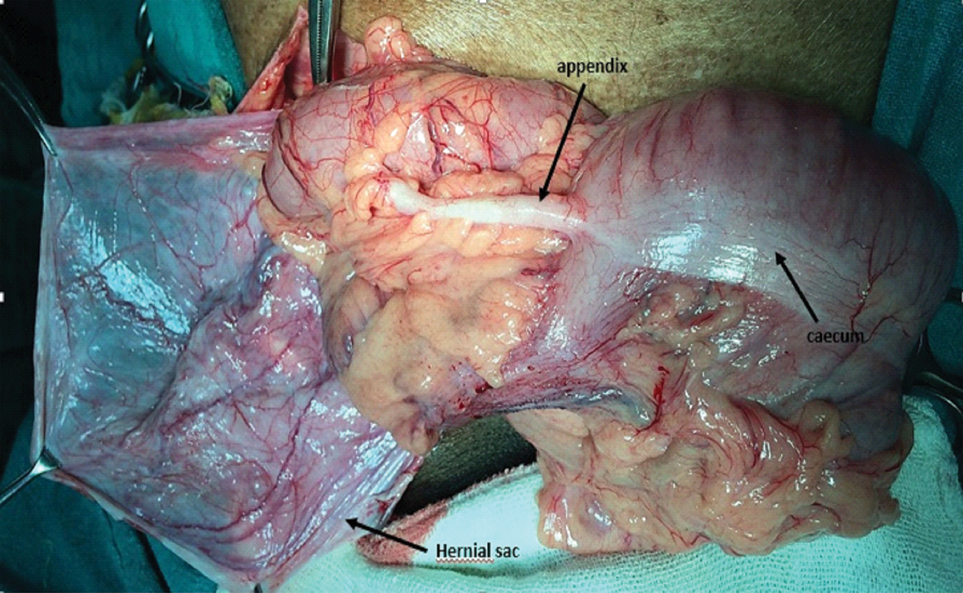
On Inguinal exploration, the obstructed hernial sac was found, dissected and opened. On opening the sac it revealed the caecum and the vermiform appendix along with a few loops of ileum as its contents [Table/Fig-1]. There were minimal inflammatory changes of the appendix or the caecum. The sac contents were reduced into the peritoneal cavity after assessing the viability of the bowel. Appendicectomy was done. Bassini’s repair of the hernia defect was done. The patient had an uneventful postoperative period and was discharged on the 12th postoperative day.
Cut open hernia sac showing caecum and appendix as the contents.
Discussion
With a reported incidence of around 0.28% to 1% of all inguinal hernias Amyand’s Hernia does classify itself into a rare entity [1,2]. The occurrence of such a herniation has been reported mostly in right sided inguinal hernias [3], probable cause being the normal anatomical location of the appendix. Existing literature suggests relatively fewer numbers of reported cases of left sided Amyand’s Hernia [4-6]. The cause being attributed to the association of situs inversus or a malrotation. No particular preference has been seen for age group or sex but more commonly Amyand’s hernia are seen in paediatric age group probably due to the patent processus vaginalis [7].
Acute Appendicitis found within the hernia sac is seen in about 0.1% and is caused by extraluminal obstruction due to pressure on the hernia neck rather than intraluminal pathology [8]. The presence or absence of inflammation of the appendix is a very important determinant of appropriate treatment. It is hard to determine whether a primary visceral inflammation is the pathological mechanism, or if the primary event is strangulation of the herniated appendix.
Losanoff and Basson distinguished four basic types of Amyand’s hernias [9,10], which should be treated accordingly. A Type 1 hernia has a normal appendix in an inguinal hernia, which is managed with a reduction and mesh repair. Types 2–4 have acute appendicitis within an inguinal hernia sac. Type 2 has an inflamed nonperforated appendix. Type 3 has a perforated appendix and type 4 is complicated with intraabdominal pathology. Type 2–4 hernias are managed with appendectomy and primary repair (without mesh). In addition, to the primary repair and appendectomy, type 3 includes a laparotomy for abdominal irrigation, possible orchiectomy or colectomy and type 4 includes investigation of pathology. This classification was later modified by Rikki Singal et al., [11]. The present case falls under type 2 Amyands hernia.
A preoperative clinical diagnosis of Amyand’s Hernia is almost practically impossible though sometimes careful imaging by experienced skillful radiologists may pick up this condition on transabdominal ultrasonography or CECT Abdomen. On USG Abdomen, a blind ended non-compressible tubular structure and increased vascularity may be seen entering the hernia sac [12]. While on CECT abdomen a tubular blind-ended structure originated from the cecum wall is observed and extends to the hernia sac [13]. There are no absolute figures on the sensitivity and specificity of these imaging methods for the diagnosis preoperatively.
Surgical modalities are varied in different presentations of Amyand’s Hernia and the above classification forms a rough guide. Use of a prosthetic material in the repair of a type 1 Amyand’s hernia is probably advocated due to the lack of inflammation. Whether to perform an appendicectomy is still debatable due to lack of evidence based data. Paediatric age group patients have a higher risk of developing an acute appendicitis and thus their appendices may be removed as compared to middle and adult age group where the appendix should be left intact [9,10]. There are various scenarios where performing an appendicectomy or using a prosthetic mesh comes into the picture. Psarras et al., reported a 32-year-old man, with the clinical appearance of an incarcerated right groin hernia, had acute appendicitis and underwent simultaneous appendectomy and conventional modified Bassini hernia repair [14].
In another case reported by Morales et al., they found a right side inguinal hernia with appendix in the sac without any signs of ischemic complications in 40-year-old male patient. Appendicectomy followed by hernioplasty was performed without any postoperative complications [15].
In our case with minimal inflammatory signs, sac contents were reduced into the peritoneal cavity after an appendicectomy and a Bassini’s repair of the hernia defect was done.
These decisions are rather simple and straightforward in type 2 where appendicectomy is undertaken and the hernia repair done without the use of any prosthetic materials. In case of type 3 and type 4, one should directly opt for an appendicectomy followed by simple anatomical repair of the hernia.
Conclusion
A surgeon performing a hernia surgery may encounter unexpected intra operative scenarios among which an Amyand’s hernia is a possibility. The presentation might be as an incidental finding during a routine hernia surgery or during an emergency surgery for an incarcerated or strangulated hernia, the decision regarding technicalities of the surgery become multifactorial. It is therefore very important to be aware of such a setting and to take an appropriate and individualized surgical approach towards such case.
[1]. D’Alia C, Schiavo ML, Tonante A, Taranto F, Gagliano E, Bonanno L, Amyand’s hernia: case report and review of the literatureHernia 2003 7(2):89-91. [Google Scholar]
[2]. Sharma H, Gupta A, Shekhawat NS, Memon B, Memon MA, Amyand’s hernia: a report of 18 consecutive patients over a 15-year periodHernia 2007 11(1):31-35. [Google Scholar]
[3]. Pellegrino JM, Feldman SD, Case report: acute appendicitis in an inguinal herniaNew Jersey Medicine: The Journal of The Medical Society of New Jersey 1992 89(3):225 [Google Scholar]
[4]. Gupta S, Sharma R, Kaushik R, Left-sided amyand’s herniaSingapore Med J 2005 46(8):424-25. [Google Scholar]
[5]. Breitenstein S, Eisenbach C, Wille G, Decurtins M, Incarcerated vermiform appendix in a left-sided inguinal herniaHernia 2005 9(1):100-02. [Google Scholar]
[6]. Carey LC, Acute appendicitis occurring in hernias: a report of 10 casesSurgery 1967 61(2):236-38. [Google Scholar]
[7]. Ivanschuk G, Cesmebasi A, Sorenson EP, Blaak C, Loukas M, Tubbs SR, Amyand’s hernia: a reviewMedical Science Monitor 2014 20:140-46. [Google Scholar]
[8]. Logan MT, Nottingham JM, Amyand’s hernia: a case report of an incarcerated and perforated appendix within an inguinal hernia and review of the literatureThe American Surgeon 2001 67(7):628-29. [Google Scholar]
[9]. Losanoff JE, Basson MD, Amyand hernia: what lies beneath—a proposed classification scheme to determine managementThe American Surgeon 2007 73(12):1288-90. [Google Scholar]
[10]. Losanoff JE, Basson MD, Amyand hernia: a classification to improve managementHernia 2008 12(3):325-26. [Google Scholar]
[11]. Singal R, Gupta S, “Amyand’s Hernia”–pathophysiology, role of investigations and treatmentMaedica A Journal of Clinical Medicine 2011 6(4):321-27. [Google Scholar]
[12]. Michalinos A, Moris D, Vernadakis S, Amyand’s hernia: a reviewThe American Journal of Surgery 2014 207(6):989-95. [Google Scholar]
[13]. Luchs JS, Halpern D, Katz DS, Amyand’s hernia: prospective CT diagnosisJournal of Computer Assisted Tomography 2000 24(6):884-86. [Google Scholar]
[14]. Psarras K, Lalountas M, Baltatzis M, Pavlidis E, Tsitlakidis A, Symeonidis N, Amyand’s hernia-a vermiform appendix presenting in an inguinal hernia: A case seriesJournal of Medical Case Reports 2011 5(1):463 [Google Scholar]
[15]. Morales-Cárdenas A, Ploneda-Valencia CF, Sainz-Escárrega VH, Hernández-Campos AC, Navarro-Muniz E, López-Lizarraga CR, Amyand hernia: Case report and review of the literatureAnnals of Medicine and Surgery 2015 4(2):113-15. [Google Scholar]