Large Ulcerated Oral Focal Mucinosis: A Rare Case Report
Saede Atarbashi-Moghadam1, Ali Lotfi2, Fazele Atarbashi-Moghadam3, Yasamin Ghaedsharafi4
1 Assistant Professor, Department of Oral and Maxillofacial Pathology, Dental School of Shahid Beheshti University of Medical Sciences, Tehran, Iran.
2 Retired Assistant Professor, Department of Oral and Maxillofacial Pathology, Dental School of Shahid Beheshti University of Medical Sciences, Tehran, Iran.
3 Assistant Professor, Department of Periodontics, Dental School of Shahid Beheshti University of Medical Sciences, Tehran, Iran.
4 Student, Research Center, Dental School of Shahid Beheshti University of Medical Sciences, Tehran Iran.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Fazele Atarbashi-Moghadam, 1st floor, School of Dentistry, Shahid Beheshti University of Medical Sciences, Daneshjoo Blvd, Evin, Chamran HWY, Tehran-1983963113, Iran.
E-mail: dr.f.attarbashi@gmail.com
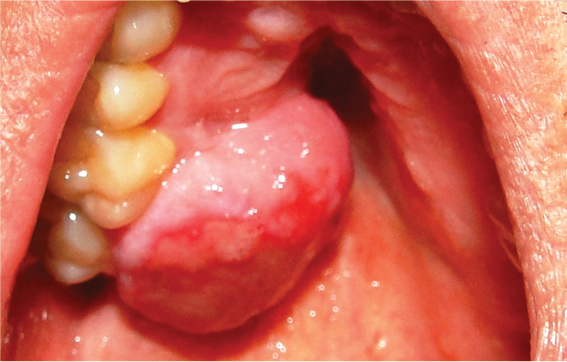
Exophytic mass, Gingiva, Myxoma
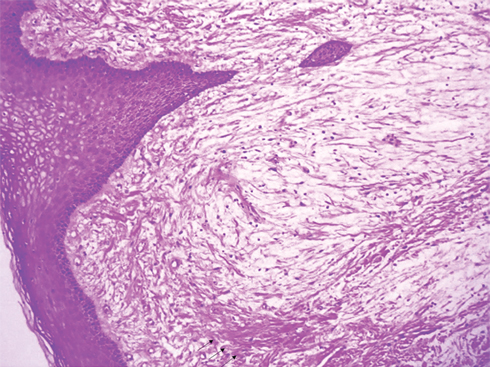
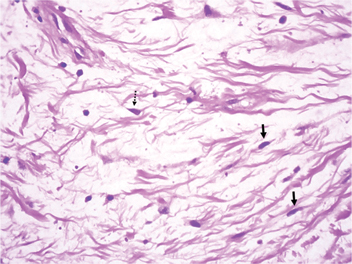
A 49-year-old man was referred to a private oral pathology center (Tehran, Iran) with chief complaint of a painless mass in the posterior of the maxilla which interfered with eating. Clinical examination showed a large (3 × 3 cm) pedunculated, submucosal ulcerated lesion that extended from palatal gingiva of 16 and 17 towards the palate [Table/Fig-1]. Its consistency was firm and it had been present for at least five years. Extra-oral examination was normal without any cervical lymphadenopathy. He had no medical problem. There was no history of previous trauma. The differential diagnosis of reactive lesions such as Peripheral Ossifying Fibroma (POF), Peripheral Giant Cell Granuloma (PGCG) and Pyogenic Granuloma (PG) were considered and excisional biopsy was performed. The specimen showed a solid, creamy-white and glisten cut surface [Table/Fig-2]. Histopathologic examination demonstrated a nodular mass covered by partially ulcerated mucosa, composed of a well-circumscribed zone of myxomatous stroma surrounded by denser collagenous connective tissue. The cells in myxomatous area were ovoid, fusiform, or stellate without atypia [Table/Fig-3,4]. These microscopic features were consistent with the diagnosis of oral focal mucinosis (OFM). On follow up, the patient was disease free for 3 years.
A large ulcerated submucosal mass originated from palatal gingiva of teeth 17 and 16 and extended towards the palate.
The gross specimen showing a circumscribed mass with solid, creamy-white and glisten cut surface.

Microscopic section showing myxomatous connective tissue intermixed with collagen fiber (black arrows) covered by oral mucosa 10X.
High-power view showing myxomatous stroma with fusiform (black arrow) or stellate-shaped (dotted arrow) fibroblasts 40X.
Discussion
OFM is a rare tumour-like lesion considered as an oral counterpart of cutaneous focal mucinosis. This mass may be a direct consequence of increased production of hyaluronic acid by fibroblasts [1]. Since the original report by Tomich, about 63 cases were reported in English literature. The most common location is gingiva (80%) followed by the palate [1,2]. Tongue involvement was also reported [1]. It shows a 2:1 female-to-male predilection [1-3] with peak incidence during the fourth or fifth decade of life [1]. It was rarely reported in children [3]. OFM usually appears as a painless nodular mass with the same colour of normal mucosa and uncommonly represents a secondary ulceration [1,3]. The lesion often existed for many months before the diagnosis [1,3]. Our case presented as an ulcerated mass. The ulceration may have been due to the chewing interference. It has no distinguishing clinical characteristics and clinical differential diagnosis most often is fibroma, PG, PGCG, POF, and peripheral odontogenic fibroma [1,3]. Bimaxillary involvement was also reported [1]. The size varies from a few millimeters to 2 cm in diameter [1]. The present lesion had a large size, approximately 3 cm. Many reports have substantiated that the structures adjacent to OFM remain intact [1,2]. A case of OFM associated with cervical root resorption was also reported [3]. The OFM is diagnosed only based on microscopic analysis [1-3]. Histopathologically, OFM demonstrates a well-circumscribed but non-encapsulated zone of loose, myxomatous stroma surrounded by denser collagenous connective tissue [1-3]. The mass frequently causes flattening of the rete ridges. The fibroblasts in myxomatous area are ovoid, fusiform or stellate in appearance [1,2]. The main microscopic differential diagnosis is soft tissue myxoma, odontogenic myxoma, nerve sheath myxoma and myxoid neuro fibroma. Soft tissue myxoma is not encapsulated and may exhibit infiltration into the surrounding soft tissue [4]. Odontogenic myxoma primarily is a bone tumour albeit; cortical perforation can also be possible [1]. Nerve sheath myxoma (neurothekeoma) is more circumscribed, shows fibrous septa between multiple myxoid nodules and more number of plump stromal cells. It typically exhibits lobulation and condensed connective tissue around the lesion. Occasionally, neurofibroma displays abundant myxoid change and mimics neurothekeoma. Clue to this diagnosis include the distinctive collagen pattern of neurofibroma [5]. Neural tumours are S-100 positive [3]. OFM is treated by surgical excision and recurrence is not reported [1-4]. In conclusion, this article points out another case of OFM with large size and ulcerated surface.
[1]. Yadav S, Malik S, Mittal HC, Singh G, Kamra H, Bimaxillaryoral focal mucinosisJ Craniofac Surg 2016 27(7):e665-67. [Google Scholar]
[2]. Joshi CP, Dani NH, Mahale SA, Patel NR, A case of oral focal mucinosis of gingiva: Lesion in disguiseJ Indian Soc Periodontol 2015 19(5):586-88. [Google Scholar]
[3]. Gabay E, Akrish S, Machtei EE, Oral focal mucinosis associated with cervical external root resorption: a case reportOral Surg Oral Med Oral Pathol Oral Radiol Endod 2010 110(4):e75-78. [Google Scholar]
[4]. Neto JR, Sendyk M, Uchida LM, Nunes FD, de Paiva JB, Oral focal mucinosis associated with surgically assisted rapid maxillary expansionAm J Orthod Dentofacial Orthop 2014 145(4):534-38. [Google Scholar]
[5]. Folpe AL, Inwards CY, Bone and soft tissue pathology 2010 1st edPhiladelphiaWB Saunders Co:225 [Google Scholar]