Hydatid Cyst (HC) disease is a zoonotic infection caused by larval stage of Echinococcus granulosus. The disease poses an important public health hazard not only because it is endemic to many parts of the world but also because of migration and travel related spread. HC may develop in almost any part of the body, most commonly found in the liver, followed in frequency by the lung, kidney, brain and bone. Involvement of other organs is rare. In this case report, we describe a rare occurrence i.e., primary HC of pancreas along with review of literature and possible differential diagnosis. Pancreatic HC disease may be associated with complications such as jaundice, cholangitis, and pancreatitis which develop as a result of fistulization of the cyst content into pancreato-biliary ducts or external compression of those ducts by the cyst. Pancreatic HC may mimick pseudocyst or cystic neoplasm of pancreas such as cystadenoma, intraductal papillary mucinous neoplasm, cystic islet cell tumour etc.
Computed tomography, Echinococcus, Magnetic resonance imaging, Pancreas, Ultrasound
Case Report
A 30-year-old woman presented to outpatient department with a history of epigastric pain since 2 months, which was intermittent in nature and radiated to the back. It was associated with frequent episodes of nausea and vomiting. General physical examination was unremarkable. No mass was palpable per abdomen. Based on the clinical findings a provisional diagnosis of pancreatitis was suggested and patient was referred to Radiology Department for further evaluation. Serum amylase was done and was found to be raised (252 U/L).
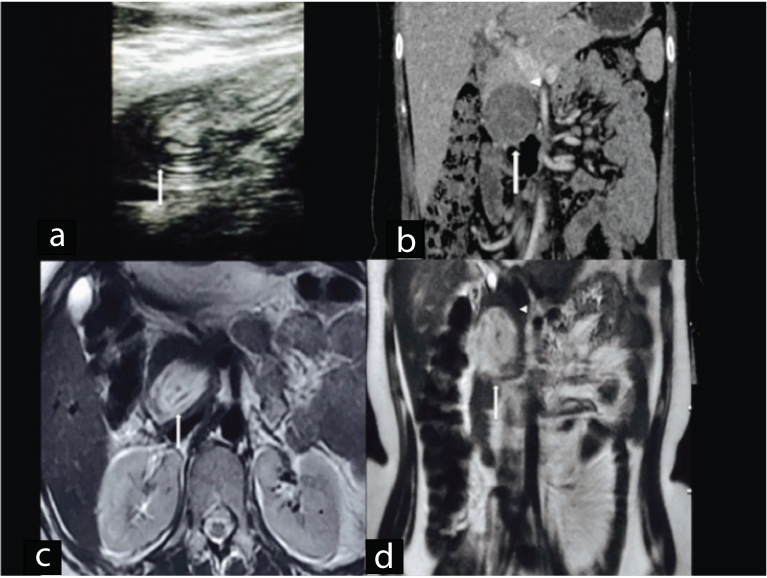
On ultrasound, there was a well defined ovoid heteroechoic lesion of size 5 x 6 cm occupying the head and uncinate region of pancreas with membranes like structure within it [Table/Fig-1a]. Based on the above findings a possibility of pseudocyst, cystic pancreatic tumour and HC of pancreas was kept. Thus, further evaluation with cross-sectional imaging was asked for as a next line of investigation Contrast Enhanced Computed Tomography (CECT) of abdomen was done and showed a well defined hypodense lesion with internal hyperdense contents in dependent part without peripancreatic free fluid or fat stranding [Table/Fig-1b]. Magnetic Resonance Imaging (MRI) displayed well defined ovoid T2 hyperintense, T1 hypointense cystic lesion with internal membranes within it [Table/Fig-1c,d]. Main Pancretic Duct (MPD) and Common Bile Duct (CBD) were unremarkable and no communication with cystic lesion was seen. Based on MRI findings pancreatic HC was suggested. ELISA serology for Hydatid Disease (HD) was positive (0.60 OD units). Patient was referred back to Surgery Department for excision of the HC. A cystopericystectomy was done followed by drainage of residual cavity. No communication with MPD or CBD could be seen during surgery. Histopathology confirmed the presence of hydatid membranes and scolices. Postoperative follow up is unremarkable.
a) Transverse high resolution sonographic image showed heterogeneously heteroechoic lesion with internal echogenic material (arrow); b) Coronal Contrast Enhanced Computed Tomography (CECT) reveals a well defined hypodense lesion with internal hyperdense contents (arrow); c) Axial; and d) coronal T2W magnetic resonance imaging revealed well defined oval lesion appearing hyperintense on T2W MRI with hypointense internal membrane like contents (arrow in ‘c’ and ‘d’).
Note the rim of normal pancreatic parenchyma surrounding the cyst (arrow head in ‘b’ and ‘d’).
Discussion
HD is a significant health problem in underdeveloped areas whereas in developed countries, HD is uncommon and is seen only in immigrants or persons with a history of travel to endemic areas [1]. HD can occur anywhere in body, however most common site is liver followed by lung, kidney, brain and bone. HD of pancreas is rare; with reported incidence varying from 0.1% to 2% of patients with HD [2].
It is a slowly growing cystic mass with varying imaging features. HC of pancreas may mimic various pancreatic cystic tumours and may cause complications like secondary pancreatitis, jaundice and cholangitis [3,4]. HC at such unusual locations may pose diagnostic difficulty; therefore early recognition may help in timely diagnosis and treatment.
HD is caused by four types of Echinococcus infections, most common being E. granulosis, whereas E. multilocularis is less common but invasive form, mimicking a malignancy [2]. Echinococcus vogeli or Polycystic HD (PHD) is the rarest clinical form. Recently, a new strain has been identified on the Tibetan plateau, Echinococcus shiquicus, but no human infection has been described uptil date [5].
Primary host is usually a dog and intermediate host may be sheep, cows or pigs and man being an accidental intermediate host [6]. After ingesting vegetables contaminated with infected dog’s faeces, ova hatch in the jejunum and embryos cross the intestinal mucosa into the portal system. In most cases, liver (59 to 75%) is the final destination of the intermediate host and lung is the second most frequently involved organ (27%). If the embryo continues through the pulmonary capillary bed, the HC may develop at any site in the body-kidney (3%), bone (1-4%), brain (1-2%) and pancreas (0.1-2%). The most probable route of pancreatic infestation is haematogenous dissemination. Other less common routes include migration of embryos down the bile duct into the pancreatic duct, via the lymphatic circulation from the intestinal mucosa to the pancreas, or by portal blood into pancreatic veins [2,6]. The most common location for HC within pancreas in descending order is the head (57%) followed by body (24%) and tail (19%) of pancreas [7].
A HC has three layers. The outer layer or pericyst, representing host response to the parasite, it is a rigid few millimeters thick layer, consisting of fibroblasts, modified host cells, eosinophils and giant cells. The middle laminated membrane is acellular, it permits the passage of nutrients and disruption of this membrane predisposes to infection. The inner germinal (or germinative) layer is thin. Scolices, develop from an outpouching of the germinal layer known as the brood capsule which are the infectious embryonic tapeworms [8,9]. The thickness of these layers depends on the location of the cyst. The layers tend to be thick in the liver, less developed in muscle, absent in bone and sometimes visible in the brain [8,9].
Clinically, presentation of pancreatic HC is variable, depending upon location and mass effect of cyst. However, HC in head of pancreas usually presents with jaundice due to external compression of CBD, while HC in body/tail of pancreas are usually asymptomatic or rarely present as portal hypertension and splenomegaly [10]. In the present case patient came with suspicion of acute pancreatitis with no jaundice, which is a rare presentation associated with pancreatic HC.
Serological tests that can be used for detection of HD are available such as serum IgG antibodies to Echinococcus sp. such as indirect haemagglutination test, Enzyme Linked Immunosorbent Assay (ELISA), latex agglutination test, complement fixation, agar gel diffusion. Reported sensitivity of these tests ranges between 85-98% for liver cysts, 50-60% for lung cysts and 90-100% for multiple organ cysts. Specificity of these serological tests is dependent upon cross reactivity of antigen with other cestode infections (Taenia solium), helminth diseases, malignancies, cirrhosis and presence of anti-P1 antibodies [7]. Cyst fluid analysis can also be done with markers such: 1) Amylase levels which are raised (more than thousand units per liter) in pseudocyst; and 2) Carcinoembryonic antigen whose values (more than 200 ng/ml) are raised in cystic pancreatic tumour particularly in mucinous epithelial lined cyst [11].
Various imaging modalities are available (USG, EUS, CT, MRI, MRCP, ERCP) that provide morphological information about cystic lesions. These help in delineating characteristic findings for HC such as floating membranes, daughter cyst, hydatid sand and also allow simultaneous guided aspiration cytology for biochemical and cytological analysis which help in differentiating HC from cystic lesions of pancreas [10].
Imaging features of HC involving any tissue may vary ranging from simple cyst to locally invasive mass mimicking malignancy, however imaging findings of liver hydatid have been classified by WHO and Gharbi [Table/Fig-2] [12].
WHO and Gharbi Classfication of HC of liver –US findings.
| WHO | Gharbi | US Characteristics |
|---|
| CE 1 | Type I | Pure fluid collection, unilocular non complicated cyst ± internal echogenicities. |
| CE 3 | Type II | Cyst with internal floating membranes, representing detached endocyst. |
| CE 2 | Type III | Cyst with internal daughter cyst and septations-Multivesicular, multiseptated cyst. |
| CE 4 | Type IV | Cyst with heterogenous solid pattern consisting on thick membranes ± few daughter cyst. |
| CE 5 | Type V | Calcified cyst with thick reflecting walls, non viable involuted cyst. |
*WHO- World Health Organisation; CE- Cystic Echinococcosis
Classical imaging findings of pancreatic HC published in the literature include-multivesicular cyst containing internal daughter cysts, hydatid sand-layering of scolices within cyst, water lily sign- floating internal membranes and cyst wall calcification along with positive hydatid serology [3,11,13]. In the present case, imaging revealed a large well-defined cystic lesion within head of pancreas with internal membrane like structure though not typical for diagnosis of HC but was possible because of high index of suspicion along with laboratory evidences.
Differentiation of cystic lesions of pancreas is important as 80% are pseudocysts and only 10% are the cystic neoplasms which requires surgical excision [2]. The differential diagnosis of cystic lesions of the pancreas is broad and is tabulated below [Table/Fig-3] [14-19].
Differential diagnosis of cystic pancreatic lesions.
| Neoplastic Lesions | Non Neoplastic Lesions |
|---|
| Cystadenoma–Serous/mucinous | Pseudocyst of pancreas. |
| Cystadenocarcinoma | Syndromic association with cysts (VHL), Autosomal dominant polycystic disease, Cystic fibrosis. |
| Intraductal papillary mucinous neoplasm | Infections: HC, Abscess. |
| Cystic islet cell tumour |
| Papillary cystic and solid tumours |
| Miscellaneous cysts: Cystic acinar cell carcinoma, Cystic teratoma, Epidermoid cystic metastasis, Vascular tumours (haemangioma, lymphangioma) etc. | Miscellaneous cysts: Lymphoepithelial cysts, duplication cysts, congenital epithelial cysts, cystic hamartoma etc. |
As primary HC of pancreas is rare and characteristic radiological findings are often not present, so differentiation of pseudocyst and cystic pancreatic lesions from HC is important for appropriate patient treatment [10].
The current definitive treatment of HD is surgical excision. If there is no communication between the cyst cavity and the bile or pancreatic ducts, scolicidal agents are injected to sterilize the cyst contents before excision. However, if the cyst is located in the vicinity of vital anatomical structures, removal of cyst contents with or without partial cystectomy is done [2]. PAIR (Puncture, Aspiration, Injection and Re-aspiration) is a minimally invasive technique used in the treatment of HC in the liver and other abdominal locations, indicated for inoperable patients and those who refuse surgery or in cases of relapse after surgery [20,21]. Complications such as pancreatic fistula may develop after partial cystectomy when there is communication between the cyst and the pancreatic duct. In such cases, a Roux-en-Y pancreaticojejunostomy is advisable [2].
Conclusion
HC can occur in pancreas and may lead to secondary pancreatitis. On imaging it may simulate pseudocyst or cystic pancreatic neoplasm. Strong imaging suspicion along with laboratory aid and high index of suspicion may help in early diagnosis and management so as to avoid fatal life threatening complications.
*WHO- World Health Organisation; CE- Cystic Echinococcosis
[1]. Bouree P, Hydatidosis: dynamics of transmissionWorld J Surg 2001 25:04-09. [Google Scholar]
[2]. Krige J, Mirza K, Bornman P, Beningfield S, Primary hydatid cysts of the pancreasS Afr J Surg 2005 43:37-40. [Google Scholar]
[3]. Lemmer ER, Krige JEJ, Price SK, Girdwood AH, Hydatid cyst in the head of the pancreas with obstructive jaundiceJ Clin Gastroenterol 1995 20:136-38. [Google Scholar]
[4]. Coskun T, Kama NA, Dener C, Gözalan U, Primary hydatid disease of the pancreasAm J Gastroenterol 1997 92:899-900. [Google Scholar]
[5]. Xiao N, Qiu J, Nakao M, Li T, Yang W, Chen X, Echinococcus shiquicus, a new species from the Qinghai – Tibet plateau region of China: Discovery and epidemiological implicationsParasitol Int 2006 55:S233-36. [Google Scholar]
[6]. Engin G, Acunas B, Rozanes I, Acunas G, Hydatid disease with unusual localizationEur Radiol 2000 10:1904-12. [Google Scholar]
[7]. Shah OJ, Robbani I, Zargar SA, Yattoo GN, Shah P, Ali S, Hydatid cyst of the pancreas. An experience with six casesJournal of the Pancreas 2010 11(6):575-81. [Google Scholar]
[8]. Pedrosa I, Saiz A, Arrazola J, Ferreiros J, Pedrosa CS, Hydatid disease: radiologic and pathologic features and complicationsRadiographics 2000 20(3):795-817. [Google Scholar]
[9]. Polat P, Kantarci M, Alper F, Suma S, Koruyucu M, Okur A, Hydatid disease from head to toeRadiographics 2003 23:475-94. [Google Scholar]
[10]. Ahmed Z, Chhabra S, Massey A, Vij V, Yadav R, Bugalia R, Primary hydatid cyst of pancreas: Case report and review of literatureInternational Journal of Surgery Case Reports 2016 27:74-77. [Google Scholar]
[11]. Basturk O, Coban I, Adsay NV, Pancreatic cysts: pathologic classification, differential diagnosis, and clinical implicationsArchives of Pathology & Laboratory Medicine 2009 133(3):423-38. [Google Scholar]
[12]. Dusak A, Onur MR, Cicek M, Firat U, Ren T, Dogra VS, Radiological imaging features of fasciola hepatica infection − a pictorial reviewJ Clin Imaging Sci 2012 2:2 [Google Scholar]
[13]. Alizadeh AH, Primary hydatid cyst of the pancreas: a reviewJ Pancreas (Online) 2016 17(3):250-56. [Google Scholar]
[14]. Le Borgne J, Cystic tumours of the pancreasBr J Surg 1998 85(5):577-79. [Google Scholar]
[15]. Astiz JM, Astiz L, Buzzi A, Primary hydatid cyst mistaken for carcinoma of the pancreasJ R Soc Med 1997 90:334 [Google Scholar]
[16]. Box JC, Douglas HO, Management of cystic neoplasms of the pancreasAm Surg 2000 66(5):495-501. [Google Scholar]
[17]. Martin I, Hammond P, Scott J, Redhead D, Carter DC, Garden OJ, Cystic tumours of the pancreasBr J Surg 1998 85:1484-86. [Google Scholar]
[18]. Panieri E, Krige JE, Bornman PC, Graham SM, Terblanche J, Cruse JP, Operative management of papillary cystic neoplasms of the pancreasJ Am Coll Surg 1998 186:319-24. [Google Scholar]
[19]. Worrall NK, Drebin JA, Pancreaticoduodenectomy for lymphoepithelial cyst of the pancreasAm Surg 2000 66:732-34. [Google Scholar]
[20]. Gupta N, Javed A, Puri S, Jain S, Singh S, Agarwal AK, Hepatic hydatid: PAIR, drain or resect?Journal of Gastrointestinal Surgery 2011 15(10):1829-36. [Google Scholar]
[21]. Corona M, Cannavale A, Bruni A, Boatta E, Allegritti M, Lucatelli P, Case report: Percutaneous treatment of multiple honeycomb-like liver hydatid cysts (type III CE2, according to WHO classification)The Indian Journal of Radiology & Imaging 2012 22(1):23 [Google Scholar]