Takayasu arteritis is an entity resulting in pan-endarteritis. It involves the principal arteries resulting in ischaemia and persistent hypertension. Hypertension affects the anaesthetic management where the principal goal is to control the haemodynamic stability during the induction and for the entire course of anaesthesia preventing damage to the end organs. We present two cases, one paediatric with hypertension refractory to medical management posted for nephrectomy and one adult patient posted for diagnostic hysterolaparoscopy. Both the cases were administered dexmedetomidine, an alpha 2 agonist during the pre-induction period. Sympatholysis caused by infusion dexmedetomidine was effectively utilized in both the cases hence, pre-induction infusion of dexmedetomidine can be utilized to obtund the haemodynamic response to intubation.
Case Report
Case 1
A 12-year-old, 40 kg female child a known case of Takayasu’s arteritis with severe left renal artery stenosis and hypertension, refractory to medical management for the past three years was scheduled for elective nephrectomy. Three years prior to presentation, she developed generalized tonic clonic seizures with loss of consciousness; she also gave history of headaches, pedal oedema, vomiting, pain abdomen, and claudication in the upper limbs since past 2 years. She was on multiple anti-hypertensives (Carvedilol 3.125 mg BD, Prazosin 2.5 mg OD, Amlodipine 5 mg BD) and Immunosuppressants (prednisolone 25 mg OD, methotrexate 20 mg once a week).
On examination, patient had pallor with cushingoid features; Upper limb arteries were not palpable bilaterally. Lower limb arteries were palpable bilaterally, with both dorsalis pedis artery feebly felt. Blood pressure recorded in both the lower limbs was greater than 180/110 mmHg. Her respiratory and central nervous system examination was normal. Cardiovascular system examination revealed a grade III systolic murmur and a carotid thrill and a bruit. ECG revealed left ventricular hypertrophy. Echocardiography had impression of concentric left ventricular hypertrophy, grade I left ventricular diastolic dysfunction, with ejection fraction of 55-60%. Catheter angiography revealed 90% stenosis of right common carotid artery, 75% stenosis of Left Common carotid artery, 85% stenosis of left vertebral artery, bilateral subclavian artery stenosis of 100%, right renal artery stenosis of 90% and the left renal artery was 100% blocked. DiethyleneTetramine Penta Acetate (DTPA) Scan revealed 95% functioning right kidney with only 5% functioning left kidney. Tuberculosis workup was negative with normal fundus examination. Her routine investigations were within normal limits with Hb of 10 gm%.
On the day of surgery, all routine medications were continued. Her baseline heart rate was 92 beats/min and BP prior to the induction in the Right lower limb was 156/88 mmHg. Standard monitoring included ECG (lead II and V), non invasive blood pressure in the right lower limb, pulse oximetery, temperature, and end-tidal CO2. Cardio-protective drugs were kept ready in view of any haemodynamic instability.
In the Operation Theatre (OT), Inj. Dexmedetomidine 0.5 μg/kg/hr infusion was given over 10 min followed by induction with Inj. fentanyl 60 μg IV and Inj. propofol 80 mg IV administered in a graded fashion. Intubation was performed with an adequate size endotracheal tube utilizing vecuronium 4 mg IV. After securing the airway with no stress response, an epidural catheter was introduced in T12-L1 space utilizing saline for identification of the epidural space. A 3-mL epidural test dose of 2% lignocaine with adrenaline 1:200000 was given. Dexmedetomidine infusion was discontinued after the placement of epidural catheter. Epidural infusion of 0.2% ropivacaine at the rate of 4 ml/hr was started during the surgical procedure. Anaesthesia was maintained with O2 (40%), N2O (55%) and Sevoflurane (MAC 1.1).
The course of anaesthesia was uneventful. Intraoperatively, the blood pressure at no stage went above 136/76 mm Hg. Patient was reversed with inj Neostigmine (0.05mg/kg) and Glycopyrrolate (0.01mg/kg). Post operative period was uneventful with epidural infusion continued at 5ml/hr (0.2% Ropivacaine) till 48 hour.
On the second postoperative day, patient developed non-oliguric renal failure with progressively rising serum creatinine from preoperative levels of 1 mg/dl to a maximum level of 5.6 mg/dl with hyperkalemia (5.9 mg/dl), and was started on Tab. torasemide 40 mg once daily. Renal replacement therapy was initiated on third post operative day and received total of eight cycles of haemodialysis within the duration of one month postoperatively.
Case 2
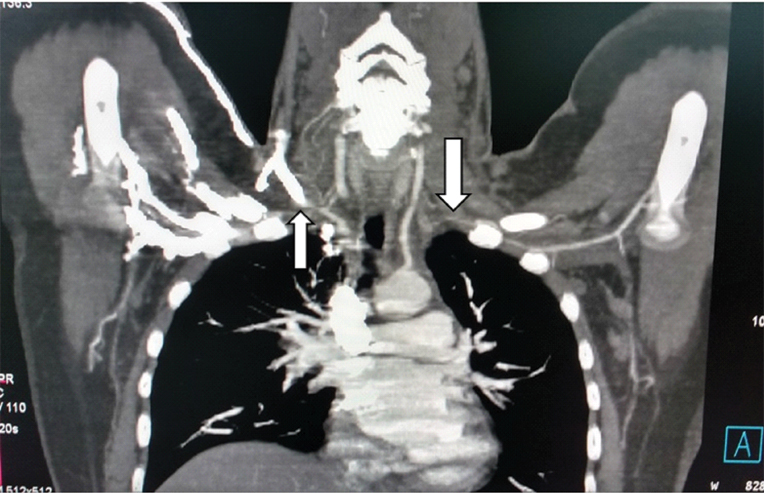
A 26-year-old lady weighing 70 kg, a known case of hypothyroidism and primary infertility was scheduled for diagnostic Hysterolaparoscopy. During Pre-Anaesthesia (PA) checkup she was observed to have non-palpable bilateral radial pulses and Blood Pressure (BP) not recordable on both upper limbs. Further investigations diagnosed her as a case of Takayasu Arteritis. Computed Tomography (CT) angiography showed bilateral subclavian artery occlusion [Table/Fig-1]. She was started on steroids and azathioprine. Elective surgery was postponed to a later date. The steroids were gradually tapered off in next six months while azathioprine 50 mg OD was continued along with Eltroxin 50 mcg OD for hypothyroidism.
Computed Tomography (CT) angiography shows bilateral Subclavian artery stenosis as being demonstrated by the arrows in the figure.
On the day of operation, all the routine medications were given orally four hours preoperatively. Standard monitoring was done along with invasive right femoral arterial blood pressure. Baseline heart rate was 80 beats/min and BP in the right lower limb was 151/80 mmHg. The patient was started on infusion Dexmedetomidine 0.5 μg/kg/hr for 10 minute followed by standard General Anaesthesia (GA) with no change in the haemodynamics.
The perioperative period was uneventful. Intraoperatively, the blood pressure at no stage went above 150/100 mmHg. However, there was a disparity between the BP recorded in the right upper limb and the right lower limb. Patient had uneventful recovery after reversal.
Discussion
Takayasu arteritis is characterized by occlusion of the principal arteries arising from the aortic arch. Young females are affected more than males. This disease is also referred as pulseless disease, aortic arch syndrome, young female arteritis, and idiopathic aortitis [1,2]. The major clinical finding is loss of palpable pulses in the upper limbs and neck. The unsuspected ischemia in vital regional vascular beds may be associated with high anaesthetic risks for these patients. Ischaemia and renovascular hypertension follow involvement of the renal arteries. Renovascular lesions come second only to the renal parenchymal diseases as a cause of persistent severe hypertension of childhood [3]. Hypertension, the major complication affecting anaesthetic management in patients with TA, is commonly renovascular, and Takayasu’s Arteritis (TA) is the most common cause of renovascular hypertension in India [4].
A few reports exist in the literature in respect of anaesthetic management of Takayasu’s Arteritis in paediatric age groups [5,6]. Paediatric cases have presented with uncontrolled hypertension with compromised renal function for renal transplantation or for adrenalectomy as a cause of Cushing syndrome [7,8].
TA can present for surgery either incidentally as in our second case, or more frequently for correction of the consequences of vascular occlusive disease as in our first case. During the preoperative visit, evaluation should focus for the clinical features suggestive of carotid involvement, like dizziness and syncope on head extension and check for carotid bruit. It is always best to keep the head in the neutral position in all cases, avoiding the hyperextension of the head during the laryngoscopy as it can lead to postoperative visual disturbances, vertigo, hemiparesis and seizure [7].
Monitoring cardiovascular status and function is extremely important in these cases and may be complicated if no peripheral pulses are present, particularly in children. In the cases described here, both the upper extremities were pulseless, so haemodynamic monitoring did not present any special problems as it was measured in the lower limbs. Direct arterial cannulation was not performed in the child due to its potential risk of inflicting trauma to the child with a progressive arteritis precipitating an occlusion and aneurysm formation in the blood vessel following cannulation [5,9]. Perioperative steroid replacement was given to prevent the occurrence of Addisonian hypotensive crisis, as these patients are on long term steroid replacement [10].
Blood pressure control is of paramount importance as these patients may have arterial aneurysm and cerebral dysfunction from carotid occlusion. Because of cardiac involvement the cardioprotective drugs were kept ready. All anti-hypertensive drugs were continued until the morning of surgery. Slow infusion of Dexmedetomidine was initiated as a pre-induction sequence to facilitate a stress free induction and intubation. Dexmedetomidine has been known for the sympatholysis as being an alpha 2 agonist with remarkable property of providing sedation, analgesia, with intact airway reflexes. Remarkably, the child’s previously intractable hypertension settled following infusion of Inj. dexmedetomidine and remained stable during the course of anaesthesia [11].
The choice of anaesthetic technique should always take into consideration the maintenance of blood pressure in the intraoperative and postoperative periods and adequate blood flow to the vital organs because of the stenosed vessels. Sympathetic block following regional anaesthesia and a subsequent decrease in blood pressure can be deleterious in a patient with stenosed arteries compromising regional circulation [12,13]. Slow administration of local anesthetics and titration of the local anesthetic to the desired level of block as done in our first case prevented a precipitous decrease in blood pressure and allow enough time to adjust for the development of sympathetic block.
General anaesthesia as a technique alone may be associated with hypertensive episodes during laryngoscopy, intubation and extubation that can lead to cerebral haemorrhage and infarction or cardiac dysfunction in a patient with TA. We opted for GA with pre induction with infusion Dexmedetomidine over 10 min in both the cases and maintenance with graded epidural for our first patient because of the site involved in the surgery and for the adequate pain relief in the post operative period. Gozal et al., and Thorburn and James et al., used epidural anesthesia and analgesia as an adjuvant to general anesthesia for hysterectomy and kidney transplantation, respectively [14,15]. Literature review confirms that both regional and general anaesthesia have been used successfully in the cases of Takayasu’s Arteritis [9].
Neurological monitoring is recommended in the patients of TA with carotid artery involvement undergoing general anesthesia. This was however not done in both our patients as it was not available and both our patients recovered with normal neurological functions.
Conclusion
TA is a progressive disorder with varied clinical features indicative of vascular involvement, some of which may fluctuate in severity.
We successfully managed two cases of Takayasu’s Arteritis under GA with pre-induction with infusion dexmedetomidine preventing stress response to intubation and minimizing the haemodynamic alterations associated with this clinical entity.
[1]. Lupi-Herrera E, Sanchez-Torres G, Marcushamer J, Mispireta J, Horwitz S, Vela JE, Takayasu’s arteritis. Clinical study of 107 casesAm Heart J 1977 93(1):94-103. [Google Scholar]
[2]. Ishikawa K, Natural history and classification of occlusive thromboaortopathy (Takayasu’s disease)Circulation 1978 57(1):27-35. [Google Scholar]
[3]. Wiggelinkhuizen J, Cremin BJ, Takayasu’s arteritis and renovascular hypertension in childhoodPaediatrics 1978 62(2):209-17. [Google Scholar]
[4]. Sharma BK, Sagar S, Singh AP, Suri S, Takayasu arteritis in IndiaHeart Vessels Suppl 1992 7:37-43. [Google Scholar]
[5]. Rozwadowski MA, Downing JW, Anesthetic management for nephrectomy in a child with Takayasu’s arteritis and severe renovascular hypertensionSAMJ 1985 67(22):898-900. [Google Scholar]
[6]. Eleftheriou D, Varnier G, Dolezalova P, Mc Mohan AM, Al-Obaidi M, Brogan PA, Takayasu arteritis in childhood: retrospective expierence from a tertiary centre in the United KingdomArthiritis Research & Therapy 2015 17(1):36 [Google Scholar]
[7]. Saravanan PA, Jacob R, Sahajanandan R, Joselyn AS, Paediatric auto renal transplantation-anaesthetic challengeIndian J Anaesth 2009 53(4):489-91. [Google Scholar]
[8]. Hemlata Kishore K, Concomitant Takayasu arteritis and cushing syndrome in a child undergoing open adrenalectomy: an anaesthetic challengeIndian J Anaesth 2014 58(4):467-69. [Google Scholar]
[9]. Kathirvel S, Chavan S, Arya VK, Rehman I, Babu V, Malhotra N, Anesthetic management of patients with Takayasu’s arteritis: A case series and reviewAnesth Analg 2001 93(1):60-65. [Google Scholar]
[10]. Goel N, Gupta K, Wardhawan S, Suchdeva P, Anand R, Undiagnosed Takayasu arteritis: An anaesthetic challengeJ Anaesth Clin Pharmacol 2009 25(4):505-06. [Google Scholar]
[11]. Sulaiman S, Karthekeyan RB, Vakamudi M, Sundar AS, Ravullapalli H, Gandham R, The effects of dexmedetomidine on attenuation of stress response to endotracheal intubation in patients undergoing elective off-pump coronary artery bypass graftingAnn Card Anaesth 2012 15(1):39-43. [Google Scholar]
[12]. Ishikawa K, Matsuura S, Occlusive thromboaortopathy and pregnancy: clinical course and management of 33 pregnancies and deliveriesAm J Cardiol 1982 50(6):1293-300. [Google Scholar]
[13]. Wiebers DO, Ischemic cerebrovascular complications of pregnancyArch Neurol 1985 42(11):1106-13. [Google Scholar]
[14]. Gozal Y, Ginosar Y, Gozal D, Combined general and epidural anesthesia for a patient with Takayasu’s arteritisReg Anesth 1995 20(3):246-48. [Google Scholar]
[15]. Thorburn JR, James MF, Anaesthetic management of Takayasu’s arteritisAnaesthesia 1986 41:734-38. [Google Scholar]