Non Iodine Avid Bone Metastasis from Differentiated Thyroid Cancer: A Case Series
Sudheesh Manoharan1, Sajith Babu Thavarool2, Sivakumar Thiagarajan3, Satheesan Balasubramanian4, Atul Singh5
1 Senior Resident, Department of Surgical Oncology, Malabar Cancer Centre, Kannur, Kerala, India.
2 Associate Professor, Department of Surgical Oncology, Malabar Cancer Centre, Kannur, Kerala, India.
3 Assistant Professor, Department of Surgical Oncology, Tata Memorial Hospital, Mumbai, Maharashtra, India.
4 Professor, Department of Surgical Oncology, Malabar Cancer Centre, Kannur, Kerala, India.
5 Senior Resident, Department of Surgical Oncology, Malabar Cancer Centre, Kannur, Kerala, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sudheesh Manoharan, Senior Resident, Department of Surgical Oncology, Malabar Cancer Centre, Kannur-670103, Kerala, India.
E-mail: drsudheesh.omfs@gmail.com
Differentiated Thyroid Carcinoma (DTC) constitute up to 90 per cent of all thyroid malignancy. The overall prognosis of patients with DTC is good, but when bone metastases are present, the overall survival at 10 years ranges from 13 to 21%. Treatment of metastatic thyroid cancer that are non iodine avid offers a surgical challenge. This paper reviews a series of three cases of DTCs with bone metastasis treated by surgery.
Follicullar carcinoma, Papillary carcinoma, Radioiodine ablation
Introduction
Metastatic lesions from differentiated thyroid malignancies are usually treated by radioiodine ablation. But when the lesions are non iodine avid, iodine ablation is not possible. Metastatectomy is the option when a non iodine avid lesion becomes symptomatic. In this paper, we are reviewing our experience in surgical management of thyroid malignancy with isolated bone metastasis.
Three cases of thyroid carcinoma with isolated bone metastasis were surgically treated. Of these, two cases were follicullar carcinoma and one was follicular variant of papillary carcinoma. A summary of data is given in [Table/Fig-1].
| Age/Sex | Complaint | Duration(months) | Site of Metastasis | Histopathology | Treatment forMetastasis | Current Status | Disease FreeInterval (months) |
|---|
| 48/M | Back pain | 12 | RibVertebra | Follicular variant of papillary carcinoma | Rib resectionExcision of vertebral mass | Disease free | 69 |
| 59/F | Pain and swelling over scalp | 12 | Skull | Follicular carcinoma | Scalp metastatectomy | Disease free | 59 |
| 65/F | Back pain | 2 | Iliac bone | Follicular carcinoma | Hemipelvectomy | Disease free | 55 |
Pain at the metastatic site was the presenting complaint in all cases. MRI and CT guided biopsy were the primary mode of evaluation of metastatic disease. These cases were considered for surgery because the patients were symptomatic, lesions were not responding to radio iodine ablation and there were no extraskeletal metastasis. Postsurgery iodine scan showed good response. All patients are still under follow up and are disease free.
Case 1
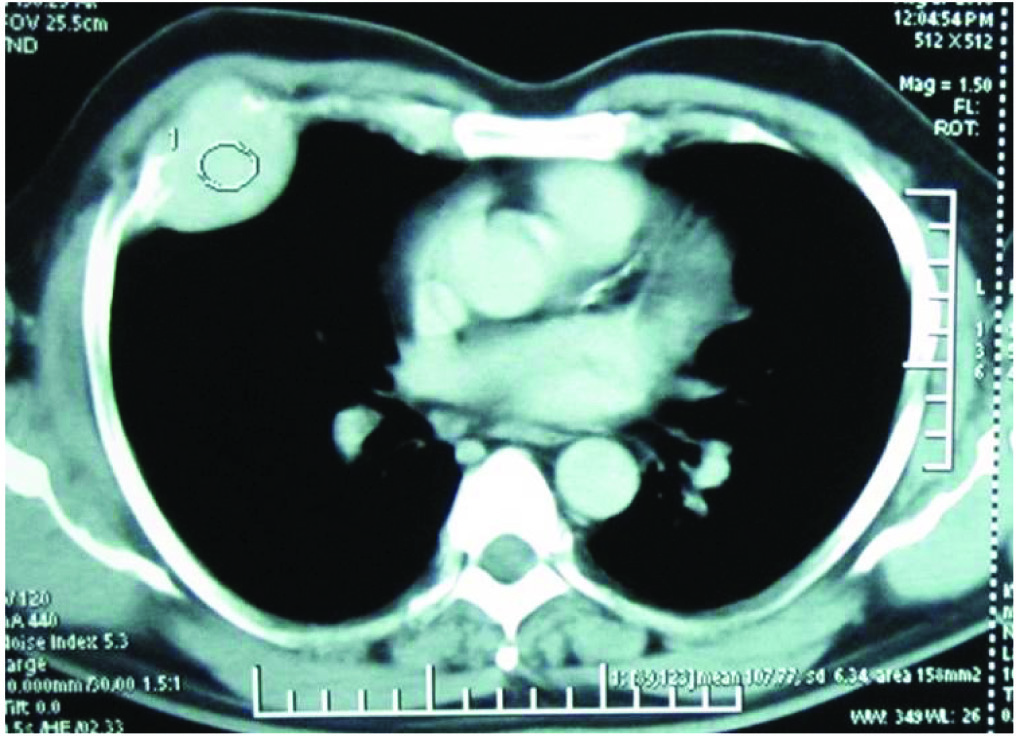
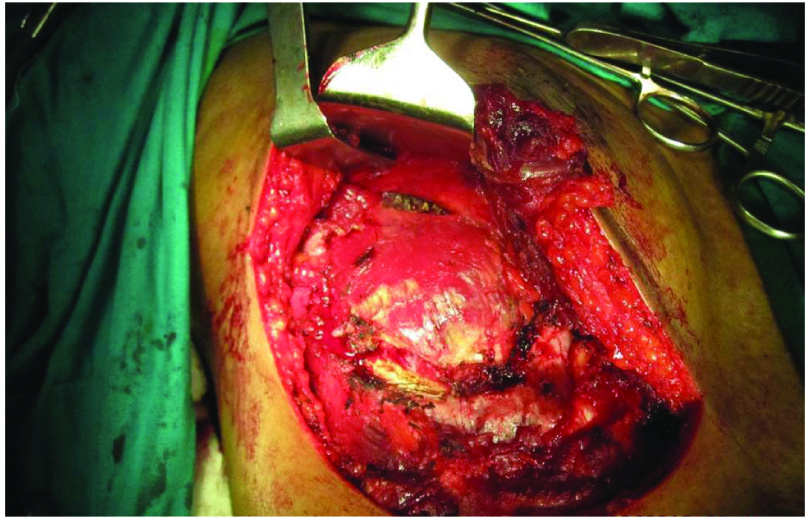
A 48-year-old male patient reported at the local hospital for back pain of one year duration. MRI scan suggested an expansile lesion in D12 vertebra involving the right pedicle and adjacent portion of lamina, compressing the spinal cord. He underwent excision of mass lesion at local hospital in October 2009. Histopathology revealed that the lesion was metastasized from papillary carcinoma thyroid. He was referred to our institution for expert management. Thorough clinical examination revealed a solitary nodule in the left lobe of thyroid, FNAC suggesting papillary carcinoma. For symptomatic relief, radiotherapy (30 Gy/10 fractions) was given for spinal metastasis. A subsequent bone scan showed postsurgery reactive changes in the D12 vertebra and another sclerotic lesion in the right fourth rib. He was treated by total thyroidectomy followed by adjuvant radioiodine ablation. The metastatic mass in fourth rib showed incomplete response to iodine ablation [Table/Fig-2]. Since the patient was symptomatic, resection of fourth rib was done [Table/Fig-3]. Histopathology suggested metastasis from follicular variant of papillary carcinoma thyroid. Postsurgery, post ablation iodine scan showed no evidence of residual disease. The patient is asymptomatic for last 69 months.
Metastatic mass in fourth rib showed incomplete response to iodine ablation.
Case 2
A 59-year-old female patient presented with a scalp swelling and pain of one year duration that was progressing. She was a known case of follicular carcinoma thyroid, treated by total thyroidectomy followed by adjuvant radioiodine ablation at local hospital one year back. Examination revealed a 12X9 cm swelling over the right frontoparietal region. No evidence of residual thyroid in neck was seen. FNAC from the scalp swelling suggested metastasis from DTC. She was treated by radioiodine ablation, but showed only partial response. Post ablation MRI scan revealed a heterogenous lesion of size 9.4X4.3 cm in the right frontoparietal region causing destruction of underlying bone and minimal compression of brain parenchyma. She was treated by scalp metastatectomy. Postsurgery post ablation iodine scan showed no fresh uptake. The patient is on follow up and is asymptomatic for last 59 months.
Case 3
A 65-year-old female patient presented with chronic, diffuse, intermittent back pain of two months duration. There was no obvious lesion clinically. MRI revealed a mass lesion in the left iliac bone with extraosseous component. CT guided biopsy showed metastasis from follicular carcinoma thyroid. USG of neck demonstrated multiple nodules with microcalcification in both lobes of thyroid. Total thyroidectomy was done followed by radioiodine ablation. Post ablation scan showed focal areas of uptake in the left iliac bone. She was taken up for surgery as she was symptomatic. Left hemipelvectomy was done. Postsurgery post ablation iodine scan was normal. She is asymptomatic for last 55 months.
Discussion
Skeletal metastasis from thyroid carcinoma is more common in patients over 45 years of age and is usually symptomatic [1,2], which was true in all the three cases presented here. Bone metastases from DTC occur in 2–13% of patients. When bone metastases are present, the overall survival at 10 years has been reported to range from 13 to 21%. Pittas AG et al., has described the clinical characteristics in patients with bone metastases from thyroid carcinomas [2]. Bone metastases were present at the initial diagnosis in 47% of patients. Vertebrae (29%), pelvis (22%), ribs (17%), and femur (11%) were the most common sites of metastases. Multiple lesions were present in 53% of the cases. In our series also there was one case each of metastasis to skull, rib and iliac bone.
Pain often presents as the principal symptom of metastatic bone involvement and progressively becomes more severe and resistant to commonly used non opioid analgesics [3]. Pathologic fractures and spinal cord compression are other frequent findings in such cases [3-5]. In our series, pain was the consistent symptom.
Diagnosis is established by correlating clinical findings with imaging. CT scan can evaluate the extent of metastatic lesions and is particularly useful for sites that are difficult to evaluate, i.e., the spine and pelvis. Literature shows variable data on the sensitivity and specificity of CT and whole-body MRI in screening for bone metastases from DTC, but when bone involvement is suspected (aggressive tumour behaviour, metastases at other sites, clinical data), whole body MRI or non enhanced CT must be employed [6]. MRI and CT scan was used for diagnosis in all our cases and the results were good. Bone scintigraphy was done in one patient with vertebral metastasis for post radiation evaluation.
Bone scintigraphy is based on the detection of osteoblastic reaction. In thyroid cancer, bone metastases are mainly osteolytic, so the proportion of false-negative and false-positive results is high [7]. A 131I or 123I whole body scan is more specific and sensitive for well differentiated thyroid cancers [8]. PET imaging is useful in metastatic lesions with high Thyroglobulin (Tg) levels and negative iodine scan [9].
Bone metastases are generally resistant to commonly used activities of 131I and may require other approaches [10]. The low remission rate (29–35%) could be related to the large extent of disease at presentation and the dose delivery to bone metastases [11]. Proye CA et al., reported less than 17% cure rate in bone metastasis by iodine therapy alone [12]. The main indications for surgery are persistent pain refractory to medical therapy, tumours with poor radioactive uptake, and spinal instability with or without neural compression [2,13]. Surgical removal of up to five bone metastases are associated with improved survival and quality of life when there are no extraskeletal lesion [13].
All the patients in our series were symptomatic as well as not completely responding to radioiodine ablation. Hence meta-statectomy was the only option for them. Radiotherapy as a palliative treatment is indicated only when pain, risk for fracture, and neurological complications of spinal cord compression are present. Complete or partial pain relief is obtained in more than 80% of patients for at least six months in 50% of cases [14]. One patient in our series with vertebral lesion was treated initially by radiotherapy for symptomatic relief.
Conclusion
The presence of bone metastases alters the prognosis of patients with DTC. Radioiodine is the first line treatment for iodine avid lesions. Literature suggests improved survival rate with surgery in selected cases. Resection of metastasis is also found to have an effect on improved response to radioiodine ablation. Hence, surgical treatment of metastases is justified by the favorable effect it has on prognosis and on the patient’s quality of life.
[1]. McCormack KR, Bone metastases from thyroid carcinomaCancer 1966 19:181-84. [Google Scholar]
[2]. Pittas AG, Adler M, Fazzari M, Tickoo S, Rosai J, Larson SM, Bone metastases from thyroid carcinoma: clinical characteristics and prognostic variables in one hundred forty-six patientsThyroid 2000 10:261-68. [Google Scholar]
[3]. Coleman RE, Metastatic bone disease: clinical features, pathophysiology and treatment strategiesCancer Treatment Reviews 2001 27:165-76. [Google Scholar]
[4]. Coleman RE, Clinical features of metastatic bone disease and risk of skeletal morbidityClinical Cancer Research 2006 12:6243s-6249s. [Google Scholar]
[5]. Bernier MO, Leenhardt L, Hoang C, Aurengo A, Mary JY, Menegaux F, Survival and therapeutic modalities in patientswith bone metastases of differentiated thyroid carcinomasJournal of Clinical Endocrinology and Metabolism 2001 86:1568-73. [Google Scholar]
[6]. Muresan MM, Olivier P, Leclère J, Sirveaux F, Brunaud L, Klein M, Bone metastases from DTCEndocrine-Related Cancer 2008 15:37-49. [Google Scholar]
[7]. Ito S, Kato K, Ikeda M, Iwano S, Makino N, Tadokoro M, Comparison of 18F-FDG PET and bone scintigraphy in detection of bone metastases of thyroid cancerJournal of Nuclear Medicine 2007 48:889-95. [Google Scholar]
[8]. Schirrmeister H, Buck A, Guhlmann A, Reske SN, Anatomical distribution and sclerotic activity of bonemetastases from thyroid cancer assessed with F-18 sodium fluoride positron emission tomographyThyroid 2001 11:677-83. [Google Scholar]
[9]. Robbins RJ, Wan Q, Grewal RK, Reibke R, Gonen M, Strauss HW, Real-time prognosis for metastatic thyroid carcinoma based on 2-[18F] fluoro-2-deoxy-D-glucose-positron emission tomography scanningJournal of Clinical Endocrinology and Metabolism 2006 91:498-505. [Google Scholar]
[10]. Schlumberger M, Challeton C, De Vathaire F, Travagli JP, Gardet P, Lumbroso JD, Radioactive iodine treatment and external radiotherapy for lung and bone metastases from thyroid carcinomaJournal of Nuclear Medicine 1996 37:598-605. [Google Scholar]
[11]. Pacini F, Cetani F, Miccoli P, Outcome of 309 patients with metastatic differentiated thyroid carcinoma treated with radioiodineWorld Journal of Surgery 1994 18:600-04. [Google Scholar]
[12]. Proye CA, Dromer DH, Carnaille BM, Gontier AJ, Goropoulos A, Carpentier P, Is it still worthwhile to treat bone metastases from differentiated thyroid carcinoma with radioactive iodine?World J Surg 1992 16(4):640-45. [Google Scholar]
[13]. Zetting G, Fueger BJ, Passler C, Kaserer K, Pirich C, Dudczak R, Long-term follow up of patients with bone metastases from differentiated thyroid carcinoma - surgery or conventional therapy?Clin Endocrinol 2002 56(3):377-82. [Google Scholar]
[14]. Muresan MM, Olivier P, Leclère J, Sirveaux F, Brunaud L, Klein M, Bone metastases from differentiated thyroidcarcinomaEndocr Relat Cancer 2008 15:37-49. [Google Scholar]