The primary aim of ICU is to provide critical care. Eye care is usually neglected, thus resulting into poor visual outcome. In previous studies, the rate of exposure keratopathy ranged from 37.5% to 50% [1]. Exposure keratopathy is defined as dryness of cornea due to any abnormality in lid anatomy or function. The proper closure of lids and lubrication are two most important factors responsible for maintaining a healthy ocular surface [2]. The patients admitted under ventilator support/sedated lose their capacity to close their eyes or blink. Critically ill patients are particularly vulnerable to develop exposure keratopathy due to decreased tear formation, reduced blink rate, incomplete eye closure, decreased corneal reflex and altered vascular permeability [3-5]. Previous studies show association between various risk factors accounting to this condition in susceptible patients. They made certain interventions for the prophylaxis but an awareness programme had not been sought so far.
The aim of the present study was to evaluate the impact of eye care education to ICU staff for prevention of exposure keratopathy in ICU patients.
Materials and Methods
This was a prospective study undertaken at ICUs of a tertiary care rural hospital affiliated with Pramukhswami Medical College, Gujarat, India, after obtaining approval from the Institutional Ethical Committee of HM Patel Centre for Medical Care and education, Karamsad between October 2014-August 2015.
Patients were observed at all ICUs for a period of five months (October 2014-February 2015) for Ocular Surface Disease (OSD). Meticulous training regarding eye care was then given to the ICU staff including intensivists, residents and nursing staff. Post training, the data was collected for another five months. All patients admitted in Medical, Surgical and Paediatric ICU of Shree Krishna Hospital with Glasgow Coma Scale (GCS) of <10/15 and Riker Sedation Score (RSS) <=3 and admitted for at least 24 hours were included in the study. Patients with total corneal opacity, previous ocular surface disorder, who took discharge, Discharge Against Medical Advise (DAMA), Discharge On Request (DOR) or who died in less than 24 hours were excluded from the study. The data collected was divided into two groups such as pre training group and post training group which included patients from October 2014- February 2015 and April 2015- August 2015 respectively.
In the training period which was in the month of March 2015, the staff of all the three ICUs including nurses, residents and intensivists was made aware of the eye care problems in sedated patients. For each ICU, seminars were conducted twice to teach them about eye care. These seminars included the same staff in both the groups by conducting small sessions at all shifts. The seminar included photos of different manifestations of OSD which can occur in sedated patients and were briefed about early warning signs of OSD.
The patients’ basic demographic profiles were noted and then were assessed for mainly three headings- lid position, conjunctival chemosis and corneal exposure. The lids were graded as the extent of conjunctiva and cornea visible as following in which grade 1: only conjunctiva was exposed, Grade 2: also lower 1/4th of the cornea was exposed, Grade 3: lower ½ of the cornea was exposed, Grade 4: ¾th of the cornea exposed and Grade 5: the entire cornea was exposed [3,6,7].
The conjunctiva was assessed for the extent of conjunctival oedema in the following manner in which Grade 1 showed conjunctival oedema/chemosis without dellen formation and Grade 2 showed oedema with dellen formation [3,6,7].
Lastly, the corneal involvement was seen. The corneas were assessed by staining them with 1% fluorescein strip and cobalt blue filter of Heinz direct ophthalmoscope. Grade 1 showed Punctate Epithelial Erosions (PEE) involving the inferior third of the cornea. Grade 2 showed PEE involving more than the inferior third of the cornea. Grade 3 showed stromal whitening in the presence of epithelial defect. Grade 4 and 5 included scar formation and microbial keratitis respectively [3,6,7].
Statistical Analysis
The descriptive statistics were used to describe the quantitative data and qualitative data was presented using frequency and analysed using Chi-square test.
Results
The total numbers of patients were 146 in which 89 were in pre training period and 57 in post training period respectively. The total subjects trained were 47 including the staff of all the three ICUs- nurses, intensivists and residents.
The incidence of exposure keratopathy in ICU patients in the pre training period was 43.82% and post training group was 33.33%. The overall incidence was 39.72%.
The maximum number of cases who were included in the study was from surgical ICU (73/146). Maximum number of patients in which exposure keratopathy was noted was from paediatric ICU (21/35) [Table/Fig-1].
| Variables | Exposure Keratopathy | Total | p-value§ |
|---|
| Yes | No |
|---|
| MICU* | 13 | 25 | 38 | 0.076 |
| PICU† | 21 | 14 | 35 |
| SICU‡ | 31 | 42 | 73 |
| 65 | 81 | 146 |
*MICU- Medical Intensive Care Unit, †PICU- Paediatric Intensive Care Unit,
‡SICU-Surgical Intensive Care Unit
§- Chi-square test
There was a significant reduction in the amount of exposure keratopathy noted as the improvement in the grades of lagophthalmos, decreased chemosis and decreased corneal involvement after giving eye care education [Table/Fig-2].
Analysis of comparative variables of exposure keratopathy.
| Variables | Pre traininggroup | Post traininggroup | p-value‡ |
|---|
| Lid position |
| Lids completely closed | 63 | 45 | 0.001 |
| Only conjunctual exposure | 18 | 11 |
| Lower 1/4th of the cornea exposed | 7 | 1 |
| Cornea fully exposed | 1 | 0 |
| Chemosis |
| No conjuctival oedema | 71 | 53 | 0.001 |
| Conjuctival oedema without dellen | 15 | 4 |
| Conjuctival oedema with dellen | 3 | 0 |
| Exposure Keratopathy |
| No corneal involvement | 50 | 38 | 0.001 |
| PEE* involving lower third of cornea | 30 | 18 |
| PEE involving >inferior third of cornea | 9 | 1 |
| Incidence | 39 (43.82%) | 19 (33.33%) | |
| Riker sedation scale | 39 (43.82%) | 19 (33.33%) | 0.248 |
| Glasgow coma scale | 39 (43.82%) | 19 (33.33%) | 0.914 |
*PEE- Punctate Epithelial Erosions
‡- Chi-square test.
The level of sedation and the risk of exposure keratopathy were compared as patients having higher sedation level are at a greater risk of developing exposure keratopathy [Table/Fig-2].
The level of GCS according to the inclusion criteria showed two types of values. The patients who were intubated, their score were calculated from 10 as verbal response could not be considered in such patients. The score percentage was calculated to make common criteria to compare the GCS scores of all intubated and non-intubated patients. Accordingly, the value of less than 66% corresponded to poor GCS according to our inclusion criteria. The lower value of GCS score denoted the lower conscious level of the patient which directly affects the blinking capacity of the patient and hence leading to exposure keratopathy [Table/Fig-2].
The outcome of the stay of ICU patients was divided into three categories-died, discharge against medical advice or transfer to ward. This shows outcome had an adverse effect on eye care as the increased morbidity and mortality showed a direct relation with all the factors contributing to the development of exposure keratopathy [Table/Fig-3].
Relation between exposure keratopathy and mortality.
| Variables | Exposure Keratopathy | Total | p-value‡ |
|---|
| Yes | No |
|---|
| Mortality | 23 | 11 | 34 | 0.04 |
| Morbidity | DAMA* | 20 | 24 | 44 |
| Transfer | 22 | 47 | 68 |
| | 65 | 81 | 146 | |
‡- Chi-square test
Note: It shows patients who fulfilled inclusion criteria and stayed for 24 hours but then later on take Discharge Against Medical Advice (DAMA)* from the ICUs.
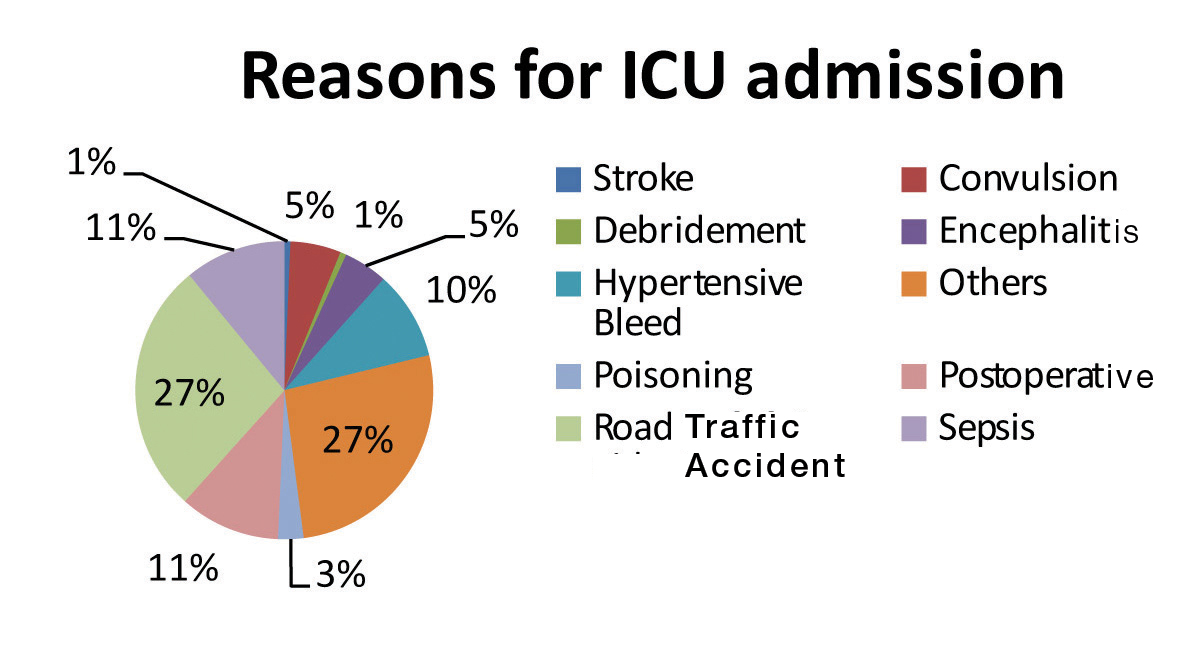
The distributions of diagnosis of all patients admitted in ICUs are described in the pie-chart where maximum cases were due to road-traffic accidents [Table/Fig-4].
Reasons for ICU admission.
Discussion
In the present study, the incidence of exposure keratopathy was 40%. The incidence of other findings like lagophthalmos was 26% and conjuctival oedema was 15%. A study by Grixti A showed the most common ocular surface disorders in the ICUs as exposure keratopathy (3.6% to 60%) followed by conjuctival chemosis (9% to 80%) and microbial keratitis [8]. Earlier studies reported an incidence of 20% to 40% [3,9,10]. Such a high rate of development of exposure keratopathy prompted the formation of eye care protocol. In the prospective study done by Kuruvilla S et al., 301 patients admitted to ICUs were assessed and a prevalence of recent plus old onset exposure keratopathy was 27.3% [11]. Study done by Jammal H et al., showed an incidence of 57% which was a prospective cohort study [12]. A study done by Imanaka H et al., showed a retrospective data analysis along with a prospective study showing the risk factors associated with corneal erosions, which showed a 20% positive cases in retrospective analysis and 60% in the prospective one [9]. A study by Mercieca F et al., evaluated 34 patients, prevalence noted was 8.7% in which eye care algorithm was followed [3]. A study done by Desalu I et al., showed an incidence of 55.4% for development of OSD [13].
The ICUs taken into consideration in our study were-Surgical, Medical and Paediatric. Out of total 146 patients included in the study, maximum numbers of patients were from surgical ICU i.e., 73. This was in accordance with the fact that surgical ICU had procured maximum of road traffic accident cases with head injury in which observation and ventilation support was necessary. Also, various postoperative patients in whom high risk surgery was undertaken were admitted there. This could be because of inadequate lid closure during operations done under general anaesthesia.
The most common diagnosis in the present study was road traffic accidents out of all the other conditions responsible for ICU admissions [Table/Fig-4].
After creating eye care awareness amongst the ICU staff following were observed:
The incidence of exposure keratopathy decreased from 44% in the pre training group to 33% in the post training group in all ICUs. Similar results were obtained from a study done by Azfar MF et al., [14].
The number of cases of lagophthalmos decreased from 26 in the pre training period to 12 in the post training period with incidence 40% in the pre training group to 21% after training (p-value=0.001). Lagophthalmos proved to be a major contribution to development of exposure keratopathy in various studies [6,9,12]. Present study showed cases with exposure keratopathy without lagophthalmos indicating several other factors could be responsible for its development in ICU patients. The ICU staff who was involved in patient care were educated regarding the lid closure as the foremost step in eye care. The algorithm defined as no treatment is required for patients with poor Glasgow coma scale scores with lids completely closed [Table/Fig-5] [3].
Algorithm for prophylaxis of exposure keratopathy.
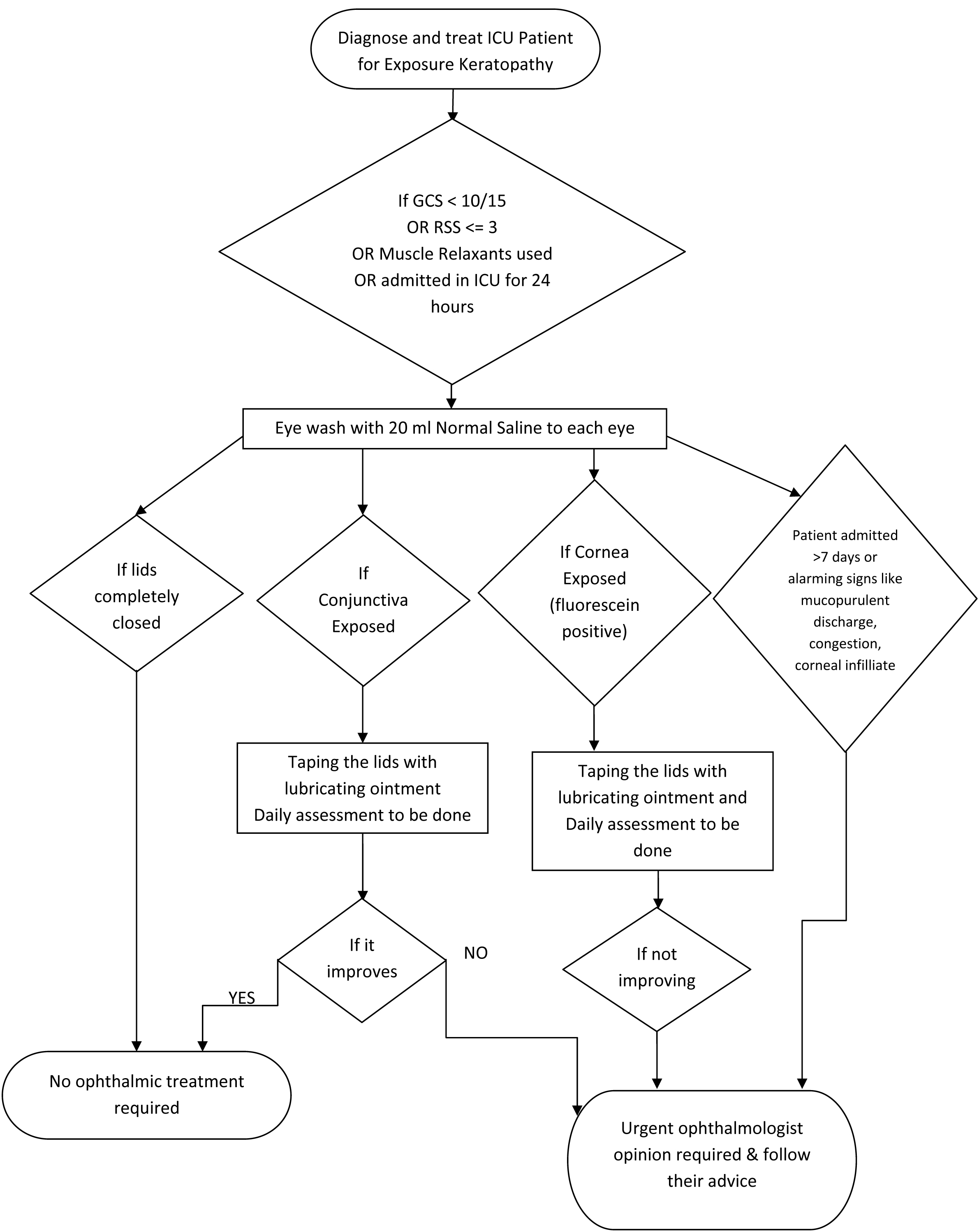
The number of patients with conjuctival chemosis significantly decreased from 18 to 4 from the pre training to post training period. The incidence of conjunctival involvement was 20% in the pre training period which decreased to 7% after the training (p-value=0.001). This shows conjuctival edema as a major contributory factor. [12]. The eye care algorithm stated that if conjunctiva is getting exposed then we should start lubricating drops or ointment as required [Table/Fig-5] [3].
Cornea is graded as the amount of its area stained with fluorescein dye. In present study, microbial keratitis was not found in any case. The numbers of patients with exposure keratopathy in pre training group were 39 which reduced to 19 in the post staining period. The incidence of exposure keratopathy decreased from 44% to 33% (p-value=0.001). Heightened awareness and control of precipitating factors leading to exposure keratopathy by the ICU staff lead to this significant decline in rate of exposure keratopathy after eye care programme [Table/Fig-2].
The present study showed an association between the sedation score and development of exposure keratopathy (p-value=0.017). Out of all patients included in the study whose Riker sedation scale was less than or equal to 3, 58 patients developed exposure keratopathy (39%). The association was not significant in the pre training group as compared to the post training group [Table/Fig-2]. On the contrary, several studies showed no association between sedation scale and exposure keratopathy [6,15].
The present study showed no association with Glasgow coma scale. Low conscious level leads to inability to close the eyes and decreased blinking which causes exposure keratopathy in ICU patients [13].
In the present study, 34 out of total 146 patients died from which 23 patients developed exposure keratopathy [Table/Fig-3]. Patients with poor outcome have associated cardiac, renal or respiratory problem which causes volume depletion or overload. Volume depletion causes decrease tissue perfusion whereas volume overload causes conjuctival oedema. Both the factors can interfere with maintenance of healthy ocular surface [13]. Hence, as proved statistically, poorer outcomes lead to exposure keratopathy in sedated and ventilated patients (p-value=0.04).
The dry and desiccated corneal epithelium along with general decreased immunity can result into secondary microbial keratitis in the ICU patients. There are increased chances of development of conjunctivitis and infectious keratitis in patients who have respiratory tract infections and require frequent suctioning [12]. In a study by Saritas T et al., there was presence of Pseudomonas aeruginosa and Acinobacter baumannii in the trachea and conjuctival smears. Pseudomonas is considered most virulent of all organisms causing rapid perforation [15]. These can lead to further complications due to infectious keratitis which can lead to permanent visual loss like perforation or scar. This can affect the social and economical life of patient if the patient is the sole bread winner of the family.
Nurses are the backbone of the critically ill patients in ICUs. If properly educated about eye care along with general care, can markedly reduce eye related complications which may cause blindness.
The strength of this study lies in the fact that it was performed in a tertiary care rural hospital which is accredited by National Accreditation Board for Hospitals and Healthcare Providers (NABH) board. It is the first study done so far in the Western province of India which includes the patients of three different ICUs of the hospital which has not been included in any study done so far.
Limitation
The limitations of this study were due to its small sample size, no follow up of patients were done, bias occurring as few surgeons would start lubricating drops after operation, non availability of portable slit lamp, humidity and temperature monitoring of all ICUs was not maintained.
Conclusion
One cannot act if one doesn’t know. Thus, creating awareness about eye care in ICU patients was important to prevent future eye problems in the patients who survived. Each ICU should monitor their patients at the primary level. Creating an Eye Care Algorithm would be beneficial according to the needs of a particular ICU. This study therefore concluded the importance of staff awareness in managing exposure keratopathy.
*MICU- Medical Intensive Care Unit, †PICU- Paediatric Intensive Care Unit,
‡SICU-Surgical Intensive Care Unit
§- Chi-square test
*PEE- Punctate Epithelial Erosions
‡- Chi-square test.
‡- Chi-square test
Note: It shows patients who fulfilled inclusion criteria and stayed for 24 hours but then later on take Discharge Against Medical Advice (DAMA)* from the ICUs.