Multidisciplinary Clinical Management of Paraneoplastic Pemphigus – A Case Report
Sadaksharam Jayachandran1, M Preethi2
1 Professor and Head, Department of Oral Medicine and Radiology, Tamil Nadu Government Dental College and Hospital, Tamil Nadu Dr. M.G.R Medical University, Chennai, Tamil Nadu, India.
2 Postgraduate Student, Department of Oral Medicine and Radiology, Tamil Nadu Government Dental College and Hospital, Tamil Nadu Dr. M.G.R Medical University, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sadaksharam Jayachandran, Professor and Head, Department of Oral Medicine and Radiology, Tamil Nadu Government Dental College and Hospital, Tamil Nadu Dr. M.G.R Medical University, Chennai-600032, Tamil Nadu, India.
E-mail: drsjayachandranmds@yahoo.com
Paraneoplastic pemphigus is a rare immunobullous disorder commonly associated with lymphoproliferative neoplasms and less commonly in carcinomas with a poor prognosis. The neoplasms produce autoantibodies that react with members of plakin family to produce a suprabasilar split and varied clinical presentations in the skin and mucous membrane. Oral erosions are the first manifestation most resistant to treatment and persist even after the underlying tumour has been resected or treated. We report here a rare case of paraneoplastic pemphigus with an underlying squamous cell carcinoma of the oesophagus that constitutes only 8% of the neoplasms associated with this condition. It was successfully managed by a multidisciplinary approach involving the Departments of Dermatology, Surgical Oncology and Oral Medicine. The oral erosions were resistant to treatment however, a patient-tailored treatment was advocated using professionally administered debridement with hydrogen peroxide diluted with hypotonic saline, high potency topical steroids, analgesic oral rinses and topical anaesthetics with systemically administered immunomodulators. Hence, management of such cases exhibiting systemic and oral manifestations require a multidisciplinary team approach to improve the quality of life of the patients.
Immunobullous disorders, Immunomodulators, Lymphoproliferative neoplasms, Squamous cell carcinoma
Case Report
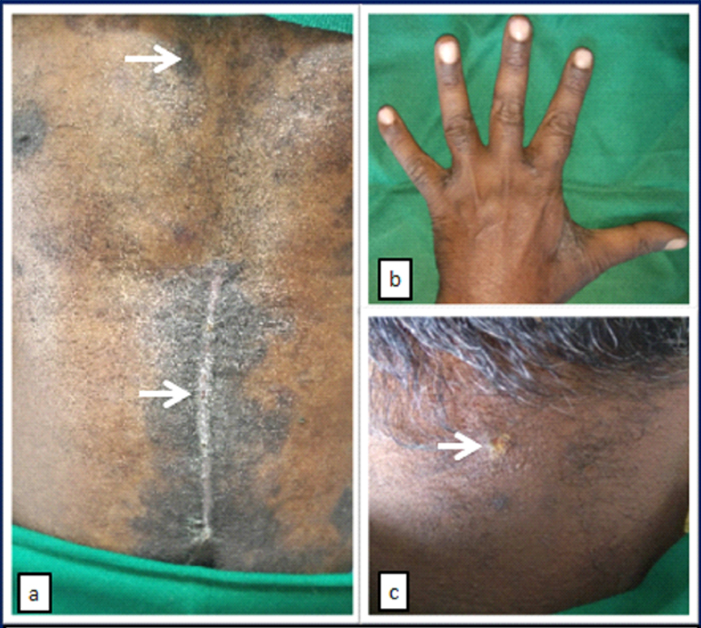
A 52 year-old-male patient, chronic smoker and alcoholic, was referred from the Department of Dermatology to the Department of Oral Medicine and Radiology for persistent oral erosions and inability to consume solids and liquids for six months. History revealed that he developed oral erosions six months back with constant remission and exacerbation followed by skin eruptions. He was subsequently diagnosed with an infiltrating poorly differentiated carcinoma of the oesophagus for which he was treated with oesophagectomy by surgical oncologists. He had concomitant polymorphous skin eruptions for which he was given prednisolone 15 mg/day and azathioprine 50 mg/day systemically with saline and potassium permanganate soaks. Crusted erosions of varying sizes and bulla with postinflammatory hyperpigmentation, dyskeratotic nails and genital ulcers were seen [Table/Fig-1a-c]. Dermal biopsy of a lesion showed a suprabasal bulla with acantholytic and dyskeratotic cells forming a net-like appearance within the bulla cavity with dense mononuclear infiltrate in the upper dermis.
a) Postinflammatory hyperpigmentation and surgical scar of oesophagectomy. b) dystrophic nails. c) ruptured bulla over nape of neck.
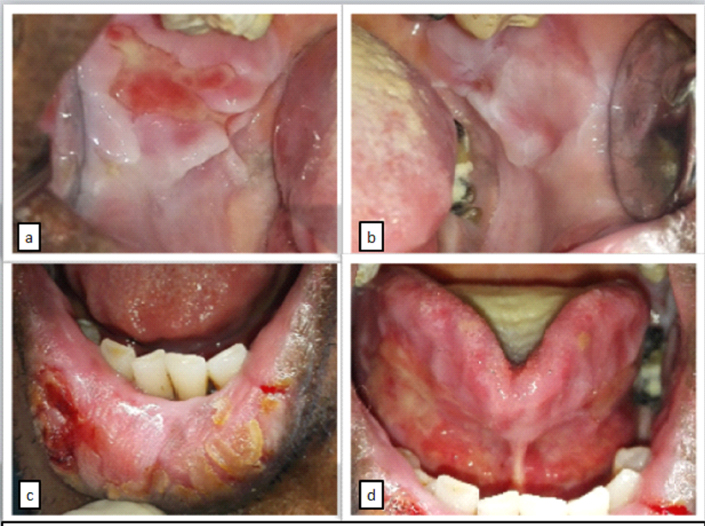
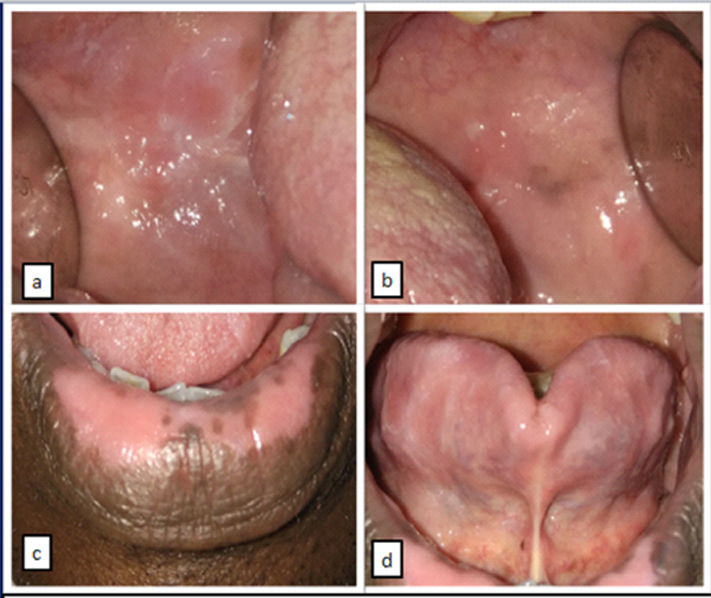
On oral examination, patient had extensive erosions of varying sizes of the buccal mucosa, floor of the mouth and the ventral surface of tongue covered by slough with crusting of lower lips [Table/Fig-2a-d] which were preceded by bullae.
a) Erosions over right buccal mucosa. b) erosions over left buccal mucosa. c) crusting of lower lips. d) erosions over floor of mouth and ventral surface of tongue.
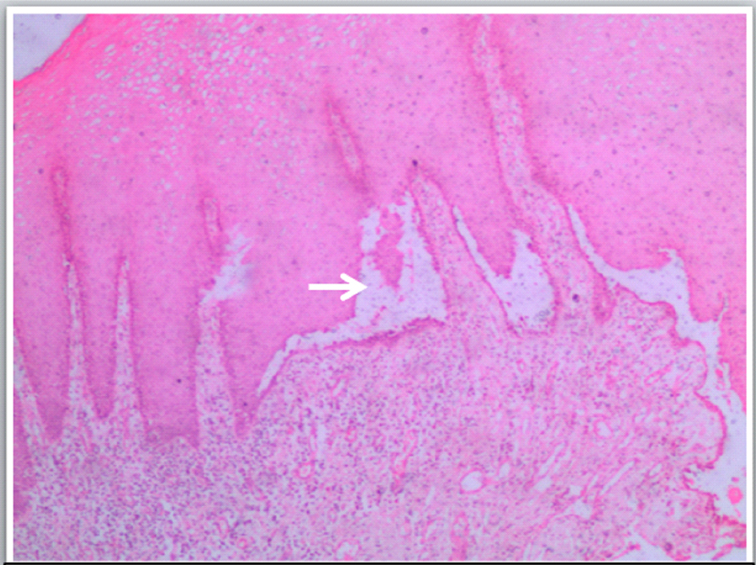
Local debridement with hydrogen peroxide solution IP (20 vol) diluted with hypotonic saline (20% w/v) in ratio of 1: 4 was done to remove the slough and crust from the oral lesions. Blood investigations were normal. An incisional biopsy from the lesional mucosa showed a stratified squamous epithelium exhibiting suprabasilar split containing acantholytic cells with dense infiltration of chronic inflammatory cells in the connective tissue [Table/Fig-3].
Photomicrograph of H&E stained histological section under 4X magnification showing acantholysis and suprabasilar split.
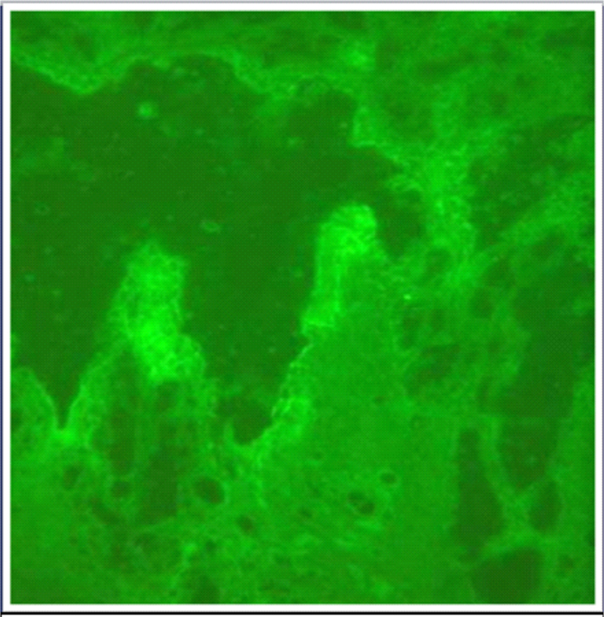
Direct immunofluorescence of perilesional mucosa showed a well oriented stratified squamous epithelium exhibiting intercellular deposits for IgG and C3C [Table/Fig-4]. As the clinical and histological findings fulfilled the criteria proposed by Camisa C and Helm TN [Table/Fig-5] [1], a diagnosis of paraneoplastic pemphigus was made.
Photomicrograph of direct immunofluorescence showing well-oriented stratified squamous epithelium exhibiting intercellular and basement member deposits for IgG
Modified diagnostic criteria proposed by Camisa C and Helm TN [1]. A diagnosis is made if all three major or two major and two or more minor criteria are met.
| Modified diagnostic criteria proposed by Camisa and Helm (1993) | Satisfaction of criteria in the case |
|---|
| Major criteria |
| • Polymorphous mucocutaneous eruptions. | + |
| • Concurrent internal neoplasia. | + |
| • Characteristic serum immunoprecipitation findings. | - |
| Minor criteria |
| • Positive staining of rat bladder epithelium by indirect immunofluorescence. | - |
| • Intercellular and basement membrane immunoreactants on direct immunofluorescence of perilesional tissue. | + |
| • Acantholysis of biopsy specimen from atleast one anatomic site of involvement. | + |
The patient was counselled regarding habits, diet, nature of the disease and the following local and systemic regimens were advocated. Topical application of a medium potency steroid ointment 0.1% triamcinolone acetonide 4 times/day, 20% benzocaine local anaesthetic ointment 4 times/day and 0.12% chlorhexidine mouth rinse twice daily were prescribed. A 45-day follow up showed the patient responding with symptomatic relief and reduction in the size of the oral erosions until the systemically administered 50 mg/day of azathioprine was discontinued and prednisolone tapered to 5 mg/day by the dermatologists. This was followed by an acute exacerbation with new erosions developing over the left buccal mucosa. An altered approach with a high potency 0.05% clobetasol propionate topical steroid ointment twice daily [2], 0.15% benzydamine oral rinse twice daily and systemic prednisolone increased to 30 mg/day. Levamisole, an immunomodulator was prescribed at 150 mg/day for 3 days a week for 2 weeks [3]. Patient responded to treatment and was constantly reviewed. A 10-month follow up showed complete healing of erosions [Table/Fig-6]. Current treatment regimen includes topical 20% benzocaine gel 4 times/day, 0.05% clobetasol propionate ointment twice daily, 0.15% benzydamine mouth rinse twice daily, prednisolone 5 mg/day and nutritional supplements.
10-month follow up showing healing in. a) right buccal mucosa. b) left buccal mucosa. c) lower lips. d) floor of mouth and ventral surface of tongue.
Discussion
Paraneoplastic pemphigus is an immunobullous disorder that has clinical, histologic and immunopathologic features distinct from pemphigus vulgaris and foliaceous. A total number of 200 cases have been reported in literature since its observation in 1990 by Anhalt GJ [4]. It affects men and women equally with mean age of 64.7 years, however, it can also occur in children too [5]. It is associated with an underlying malignancy, the most common being lymphoproliferative disorders (84%) such as non – Hodgkin’s lymphoma, chronic lymphocytic leukaemia and Castlemann’s disease. The lesser associated neoplasms (16%) include carcinomas, sarcomas and malignant melanomas out of which the patient falls into the rarer associated carcinomas that comprise only 8% of the reported cases [6]. The underlying tumour produces autoantibodies that cross react with plakins of the cytokeratin family found in desmosomes and hemidesmosomes that anchor the epithelium with basement membrane causing a suprabasilar split. Cutaneous lesions are polymorphic ranging from papules to pustules appearing after the onset of oral lesions that commonly involve the upper trunk, head, neck, extremities and rupture to form erosions. Histologically, the presence of dyskeratotic keratinocytes in a suprabasal acantholytic lesion is a characteristic feature. Direct immunofluorescence of perilesional mucosa shows deposition of IgG with or without IgA and C3 in a combined granular linear complement deposition along the basement membrane and epithelial intercellular spaces. Indirect immunofluorescence shows positivity for transitional epithelia. Immunoprecipitation of serum reveals characteristic banding at 190, 210kd protein correlating to periplakin, envoplakin proteins [7]. The original criteria for the diagnosis of paraneoplastic pemphigus was proposed by Anhalt GJ et al., and was later modified by Camisa C and Helm TN in 1993 [Table/Fig-5], [1]. Treatment includes the use of immunomodulating and immunosuppressive agents, intravenous immunoglobulins and plasmapheresis. Paraneoplastic pemphigus has a poor prognosis due to sepsis, respiratory failure and from the underlying neoplasm itself. All cases of paraneoplastic pemphigus need a multidisciplinary clinical approach for its efficient management.
Oral erosions is a constant feature of paraneoplastic pemphigus that severely impairs the quality of life of the already debilitated patient. These oral erosions are extremely resistant to treatment and persist even after the underlying tumour has been treated. A combined systemic and topical regimen is necessary to achieve symptomatic relief. Different drugs in varying combinations have been used to treat immunobullous disorders with oral manifestations. For refractory oral erosions as in paraneoplastic pemphigus, a patient specific treatment modality is needed to achieve symptomatic relief. The use of professionally administered hydrogen peroxide diluted with normal saline has been substantiated by studies where very few subjects have experienced irritant effects due to hydrogen peroxide only when mixed with hypertonic saline [8]. The combined use of a local debridement agent, local anaesthetic, steroid ointment along with systemically administered immunomodulators and immunosupressants can together bring about a successful remission of the lesion.
Conclusion
Patients with paraneoplastic pemphigus need oral hygiene and management of the resistant vesiculobullous eruptions of the oral cavity which compromises the nutritional status of the patient. Oral medicine specialists play a pivotal role in maintaining oral hygiene, management and monitoring of lesions in patients with such systemic manifestations and timely referral to other disciplines. This patient was managed with a multidisciplinary approach involving oncologists, dermatologists with the specialists in Oral Medicine managing the most constant and incapacitating manifestations to improve the quality of life.
[1]. Camisa C, Helm TN, Paraneoplastic pemphigus is a distinct neoplasia induced autoimmune diseaseArch Dermatol 1993 129(7):883-86. [Google Scholar]
[2]. González-Moles MA, Scully C, Vesiculo-erosive oral mucosal diseases – Management with topical corticosteroids: fundamental principles and specific agents availableJ Dent Res 2005 84(4):294-301. [Google Scholar]
[3]. Scheinfeld N, Rosenberg JD, Weinberg JM, Levamisole in dermatologyAmerican Journal of Clinical Dermatology 2004 5(2):97-104. [Google Scholar]
[4]. Anhalt GJ, Kim SC, Stanley JR, Korman NJ, Jabs DA, Kory M, Paraneoplastic Pemphigus: An autoimmune mucocutaneous disease associated with neoplasiaN Engl J Med 1990 323:1729-35. [Google Scholar]
[5]. Sehgal VN, Srivastava G, Paraneoplastic pemphigus/ Paraneoplastic autoimmune syndromeInt J Dermatol 2009 48:162-69. [Google Scholar]
[6]. Kaplan I, Hodake E, Ackerman L, Mimouni D, Anhalt GJ, Calderon S, Neoplasms associated with paraneoplastic pemphigus: A review with emphasis on non-hematologic malignancy and oral mucosal manifestationsOral Oncol 2004 40:553-62. [Google Scholar]
[7]. Yong A A, Tey H L, Paraneoplastic pemphigusAustralasian Journal of Dermatology 2013 54:241-50. [Google Scholar]
[8]. Walsh LJ, Safety issues relating to the use of hydrogen peroxide in dentistryAust Dent J 2000 45(4):257-69. [Google Scholar]