Diagnostic Dilemma of Cytology in Salivary Gland Neoplasm: Case Report of a Rare Diagnosis with Brief Review of Literature
Aruna Chhikara1, Preeti Rai2, Manjula Jain3, Brijnandan Gupta4, Sunil Kumar5
1 Senior Resident, Department of Pathology, Lady Hardinge Medical College, New Delhi, India.
2 Associate Professor, Department of Pathology, Lady Hardinge Medical College, New Delhi, India.
3 Director Professor, Department of Pathology, Lady Hardinge Medical College, New Delhi, India.
4 Senior Resident, Department of Pathology, All India Institute of Medical Sciences, New Delhi, India.
5 Professor, Department of Ear Nose and Throat, Lady Hardinge Medical College, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Brijnandan Gupta, Senior Resident, Room No. 1063, Department of Pathology, First Floor, Teaching Block, All India Institute of Medical Sciences, New Delhi-110023, India.
E-mail: brij9890470@gmail.com
Carcinoma ex Pleomorphic Adenoma (Ca ex PA) is a rare malignancy accounting for 3.6% of all salivary gland neoplasms. Malignant component of Ca ex PA is most often adenocarcinoma, Not Otherwise Specified (NOS). Myoepithelial carcinoma is a rare subtype of Ca ex PA. We present a case of myoepithelial Ca ex PA, firstly, due to its low prevelance and secondly, due to the frequent diagnostic conundrum it poses to the clinicians and pathologists.
Carcinoma ex pleomorphic adenoma, Myoepithelial carcinoma, Parotid region
Case Report
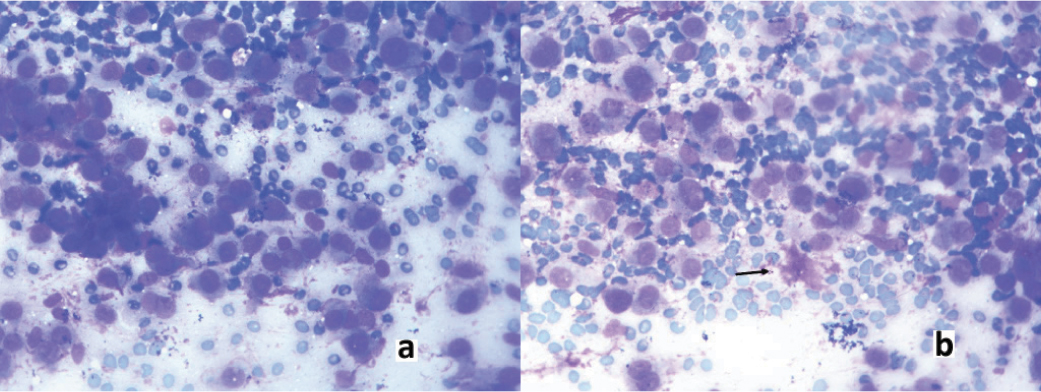
We present a case of 44-year-old female who presented with a swelling in the left parotid region. She had a painless swelling in the left parotid region 10 years back. Her FNAC at that time was reported as monomorphic adenoma and debulking surgery was performed. She had an uneventful course unless seven years later, when she again developed swelling in the left parotid region which gradually increased to a size of 7.4 cm × 4.8 cm x 3.4 cm. FNAC was performed which revealed highly cellular smears with tumour cells arranged in clusters, sheets as well as singly lying along with abundant basement like material [Table/Fig-1a,b]. The cells were round to oval with centrally placed round nucleus showing mild to moderate anisonucleosis and fine chromatin. Possibilities of monomorphic adenoma/adenoid cystic carcinoma were suggested and urgent excision was advised.
a) FNAC showed tumour cells arranged in clusters and also in sheets (Giemsa 40X); b) Among the tumour cell population, basement membrane like material (arrow) was also identified (Giemsa 40X).
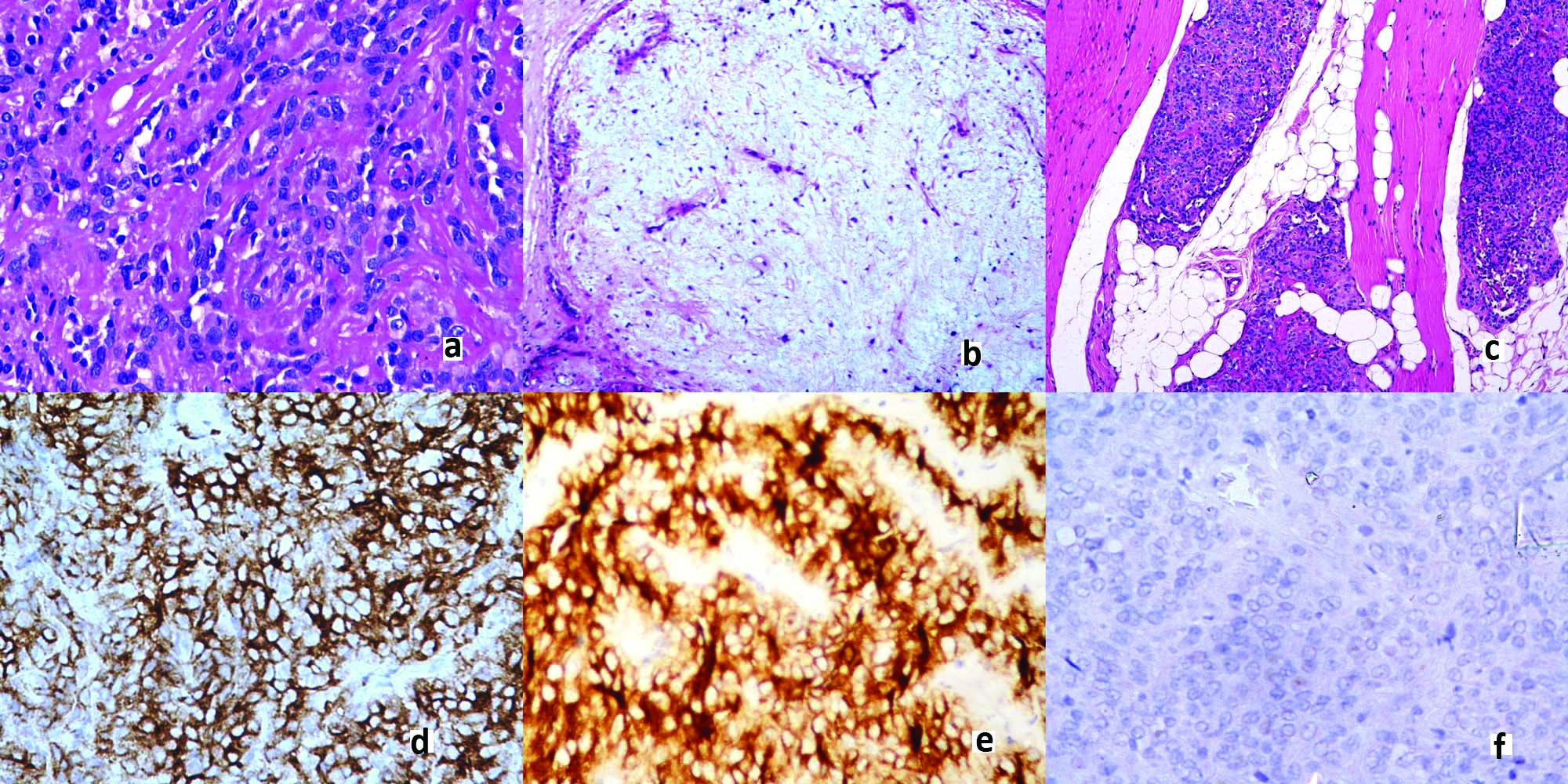
The patient underwent a total parotidectomy. We received the tumour in multiple fragments, which measured 7.4 cm x 4.8 cm x 3.4 cm. The tumour was predominantly solid, grey white with few cystic areas. The histopathological sections revealed an infiltrative growth pattern with a multinodular architecture. The cells were oval to spindle shaped arranged in lace-like pattern, forming trabecular and fascicles with interspersed abundant hyaline material [Table/Fig-2a]. A focus of chondromyxoid stroma was also noticed [Table/Fig-2b]. The tumour invaded into the adjacent salivary gland and fat and muscle in form of variable sized nodules with pushing borders [Table/Fig-2c-f]. However, no lymphovascular invasion and perineural invasion were noticed. Immunohistochemistry panel to establish the nature of tumour was put up. The tumour cells showed positivity for pan-CK, CD10, S-100 and calponin while they were negative for CEA and EMA. The Ki67 index was found to be low. Based on the myoepithelial nature of tumour cells established on immunohistochemistry and presence of chondromyxoid foci as a remnant of previous existing salivary gland pleomorphic adenoma a final diagnosis of myoepithelial Ca ex PA was given. The patient underwent first cycle of radiotherapy but was subsequently lost to follow up.
a) Tumour cells in lace-like pattern, forming trabeculae and fascicles with interspersed abundant hyaline material (H&E 40X); b) Focus of chondromyxoid stroma (H&E, 4X); c) Invasion of tumour into adjacent salivary gland, fat and muscle in form of variable size nodules (H&E, 4X); d) Strong cytoplasmic positivity of Calponin (IHC, 40X); e) Strong CD10 positivity (IHC 40X); f) EMA was completely negative (IHC, 40X).
Discussion
Ca ex PA can be carcinomatous transformation of a primary (de novo) pleomorphic adenoma or can occur in background of recurrent pleomorphic adenoma. It predominantly affects the major salivary glands; the parotid gland being most common followed by submandibular gland [1]. Myoepithelial carcinoma of the salivary glands is a neoplasm composed of tumour cells with myoepithelial differentiation and is characterized by its infiltrative growth and its potential for metastasis. Myoepithelial carcinomas comprise only about 1% of all salivary gland carcinomas. All grades between benign myoepithelioma and myoepithelial carcinoma can be seen. Approximately, half of the cases arise from pre-existing pleomorphic adenoma or myoepithelioma, particularly in recurrence. It accounts for 3.6% of all salivary gland neoplasms and is 6.2% of all cases of PA [2,3].
Myoepithelial carcinoma at times remains challenging, both in establishing a diagnosis and in predicting a patient’s prognosis. Factors that contribute to these difficulties include a history of a pre-existing benign lesion, wide variability of the histopathological features and heterogeneous myoepithelial cell cytomorphology, a wide spectrum of tumour grade with cytological abnormalities that vary from benign to equivocal to the subtle and no well defined prognostic parameters. Myoepithelial carcinoma is a difficult diagnosis on cytology as its morphological features are variable and it may lack overt features of malignancy [4]. The present case showed predominant population of cuboidal to oval cells with moderate anisonucleosis and abundant basement like features. Adenoid cystic carcinoma also shows similar features and hence histopathological findings are mandatory for diagnosis. Our patient had a protracted course of three years. The present case posed a diagnostic challenge as the resected tumour post recurrence demonstrated a relatively low mitotic index not exceeding 2 mitoses per 10 high-power fields, a rate not significantly different from that seen in benign myoepithelial lesions, which are reported to have between 1-5 mitoses per 10 high-power fields [4]. Many researchers believe that a finding of infiltration through a nodular growth pattern or through single cell files into the surrounding tissue is a minimum requirement for establishing a histopathologic diagnosis of malignancy [5,6]. A nodular growth pattern is seen in many myoepithelial carcinomas, but a diffuse pattern has also been described [6,7]. Multinodular infiltration into the surrounding tissue was found in our patient. Some forms of benign salivary gland neoplasia may recur after attempted surgical resection as multiple tumour nodules. PA is widely known to have such a pattern of recurrence [5]. The microscopic distinction between a benign tumour with only nodular recurrence and a salivary gland malignancy exhibiting a nodular growth pattern is dependent on the finding of tumour cell infiltration into surrounding structures. The margins of the surgically resected specimen in our case were positive hence the patient was referred for radiotherapy and has received her first cycle.
Conclusion
Ca ex PA is an uncommon lesion arising in a common lesion. The lesion is a diagnostic challenge for pathologist. Clinical behaviour of “de novo” myoepithelial carcinomas and of that arising in PAs and benign myoepitheliomas is similar. The invasive tumours behave in an aggressive fashion with death occurring in one-third of patients, recurrences in another one-third. Only one third of patients have disease free survival. Thus, an early and accurate diagnosis with close follow up is must for survival of patient.
[1]. Gnepp DR, Wenig BM, Malignant mixed tumours. Ellis GL, Auclair PL, Gnepp DRSurgical pathology of salivary the glands 1991 PhiladelphiaSaunders:350-68. [Google Scholar]
[2]. Gnepp DR, Malignant mixed tumours of the salivary glands: a reviewPathol Annu 1993 28:279-328. [Google Scholar]
[3]. Nouraei SA, Hope KL, Kelly CG, McLean NR, Soames JV, Carcinoma ex benign pleomorphic adenoma of the parotid glandPlast Reconstr Surg 2005 116:1206-13. [Google Scholar]
[4]. Sehgal S, Goyal P, Singh S, Kumar A, Fine needle aspiration cytology of Myoepithelial carcinoma of salivary gland: diagnostic challenge to cytopathologistJcytol 2013 30:207-10. [Google Scholar]
[5]. Ellis G L, Auclair P L, Tumours of salivary glandsAtlas of tumour pathology 1995 3rd series, fascicle 17Washington D CArmed forces institute of pathology:337-43. [Google Scholar]
[6]. Sevara A T, Sloman A, Huvos AG, Klimstra DS, Myoepithelial carcinoma of salivary glands: a clinicopathological study of 25 patientsAm J surg Pathol 2000 24:761-74. [Google Scholar]
[7]. Nagao T, Sugano I, Ishida Y, Tajima Y, Matsuzaki O, Konno A, Salivary gland malignant myoepithelioma: a clinicopathologic and immunocytochemical study of ten casesCancer 1998 83:1292-99. [Google Scholar]