Over the past three decades, Total Knee Replacement (TKR) has evolved as a successful procedure for the management of pain, deformity and motion restriction related to severe degenerative arthritis [1]. Advancement in technology in terms of design and building materials has made TKR a highly effective, safe, and predictable orthopaedic procedure [2-4].
The TKR procedure is rapidly gaining acceptance as a suitable treatment for relieving pain, restoring deformity, and restoring knee function in patients with arthritis [1]. As per the American Academy of Orthopaedic Surgeons (AAOS), the number of knee replacement in patients aged 45-64 years has tripled between the years 2000 and 2012; whereas it has increased by 95% for patients who were 65 years or above [5]. More than 75,000 to 80,000 knee replacement surgeries are performed every year in India [6].
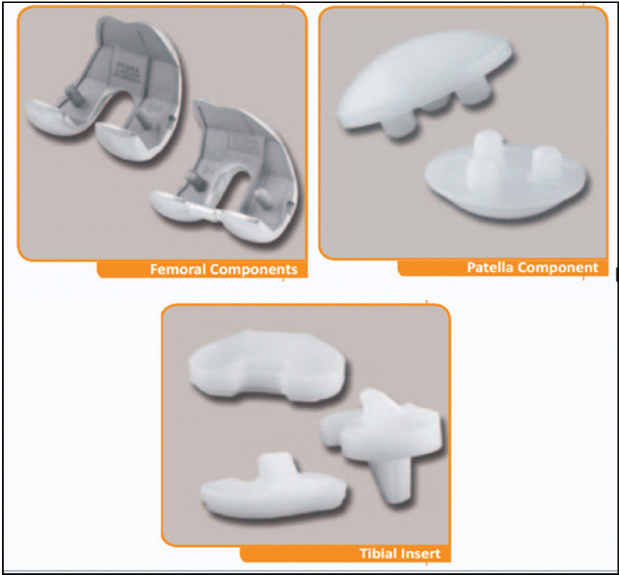
The Freedom Total Knee System is an artificial prosthetic device for total knee replacement. The advanced design engineering technologies, as well as the clinical experience of the development team, has allowed for the development of the implant design which caters to the anatomical, physiological, and lifestyle requirements of the patients. The system’s significant design advances for femoral, tibial, and patellar components along with its sizing innovations are meant to allow patients achieve optimal high-flexion motion.
The present study was conducted to retrospectively review the clinical outcomes for efficacy and performance of Freedom Total Knee System in TKR.
Materials and Methods
Study Design and Population
This was a retrospective, post-marketing study of patients who underwent total knee replacement, using the Freedom Total Knee System. Around 600 TKR surgeries are performed at the study centre annually. Patients pertaining to the inclusion and exclusion criteria were enrolled for this study from April 2011 to October 2012 and were followed up for three years. Clinical outcomes for performance and survivorship were analyzed in 158 patients treated for knee pain and limited movement caused by osteoarthritis, at a single-center in India.
The study was approved by the Institutional Ethics Committee. All the patients above the age of 18 years and who completed at least three years after TKR were observed for the study purpose. Only the osteoarthritis patients treated with TKR were included while the patients who received the implant for treatment of rheumatoid arthritis and traumatic injury were excluded. Obese patients defined by BMI of 35 or more were not evaluated for the study purpose.
Study Device and Interventional Procedure
The Freedom Total Knee System is an artificial prosthetic device for total knee replacement. Femoral components are made of Cobalt-Chromium-Molybdenum (CoCrMo) alloy and offer choice of Cruciate Retaining (CR) or Posterior Stabilized (PS) components using the same instrumentation. The thin anterior flange and six-degree patellar groove assure smooth patellar tracking and efficient bone preservation. Both the left and right femoral components are available in eight sizes that match with several tibial sizes to accommodate patient needs. The present study utilized All-poly tibial components only. The “All Poly-Fixed Bearing” tibial base plate is made from Ultra High Molecular Weight Polyethylene (UHMWPE) and is available in both CR and PS options. The All-poly tibial component of the Freedom Total Knee System is the first FDA-approved All-Poly tibial component knee implant for high flexion. The articular patellar components are made from UHMWPE and come with a central cement recess and three-peg design to ensure best bone interface and optimal stability. The Freedom Total Knee System is designed to provide high flexion while allowing substantial bone-conservation. The implant incorporates unique engineering where seven tangential radii accommodate changes in the degree of flexion across the whole range of motion without increasing the requirement for bone resection. The thin anterior flange of the femoral component minimizes overhanging over the anterior face of the femur, reduce overstuffing, reduce bone resection and prevent soft tissue impingement during extension. Furthermore, the femoral component sizing of the implant has been optimized to provide anthropomorphic fit as per the patient’s size and stature [7] [Table/Fig-1].
Different components of Freedom® Total Knee System.
*Courtesy: Maxx Orthopedics [7]
The operative procedure was conducted via the midvastus approach [8]. The gap technique was performed in all knee patients.
Postsurgical bleeding and oedema were restricted by using cryo-cuffs. Antithrombotic stockings were used to prevent deep venous thrombosis. The presence of thrombosis was determined by Doppler ultrasound measurement before and six weeks after surgery. The drainage tube was removed two to three days postsurgery, when drainage reached < 100 mL. The day after removal of the drainage tube, passive knee joint exercises using the continuous passive machine were initiated. Physical therapy for weight-bearing and walking, including active and passive joint motion exercise were conducted during hospitalization. Intravenous antibiotics in the first week were administered, followed by oral administration for the subsequent two weeks.
End-Point, Definitions, and Follow up
The performance endpoint was defined as the absence of any revision TKR, absence of aseptic loosening, and absence of implant failure at three-years follow up.
Primary efficacy endpoint was the maximum range of motion in patients observed at a minimum of three-year follow up after the index procedure. Secondary efficacy endpoint was to determine the clinical and social quality of life as per the American Knee Society Score [9]. It also included evaluation of pain relief following primary TKR as per modified WOMAC pain score and stiffness score [2].
At the end of three years after the index TKR procedure, all the 158 patients were contacted telephonically. Details about the requirement for revision procedure, if any, were taken. All the patients were asked to visit the clinic for clinical examination of efficacy and performance scores.
Statistical Analysis
Categorical data were presented as counts and percentages. Continuous variables were presented as a mean±standard deviation. All data were processed using the Statistical Package for Social Sciences, version 15.0 (SPSS, Chicago, IL, USA).
Results
3.1 Baseline and Demographic Characteristics
A total of 158 osteoarthritis patients requiring TKR were enrolled for the study. Total number of TKR performed was 191. The mean age of the patients was 67.67 years, and the group comprised of 43% men and 57% women. Mean BMI for the patients was 28.97±3.33 [Table/Fig-2]. The average length of follow up was 4.3 years (Range: 3.3 to 5.6 years).
Demographic and baseline characteristics.
| Variables | N = 158 |
|---|
| Age (mean±SD) | 67.67±7.87 |
| Gender (n%) | Female | 90 (57%) |
| Male | 68 (43%) |
| BMI (mean±SD) | 28.97±3.33 |
| Height (mean±SD) | 160.95±10.86 |
| Previous Joint Surgery (n %) | Yes | 0 |
| No | 158 (100%) |
3.2 Outcomes for Performance
A total of 191 implants were installed which comprised of 103 implants for left knee and 88 implants for the right knee. Telephonic follow up suggested that none of the 191 implants required a revision procedure at a minimum of three years follow up. Thus, the performance observed for the Freedom Total Knee System at a minimum of three years (range 3.3-5.6 years) was termed excellent [Table/Fig-3].
| Implant | 158 patients (191 implants) |
|---|
| Left | 103 implant (54%) |
| Right | 88 implant (46%) |
| Unilateral TKR | 125 patients (79%) |
| Bilateral TKR | 33 patients (21%) |
| Revision TKR | 0% |
3.3 Clinical and Functional Outcomes by AKSS and Range of Motion
Out of the 158 patients, immediate postoperative (day 2) follow-up was available for all 158 patients (191 implants). However, one-year follow up was available for 96 patients (129 implants) and three-year follow up was available in 35 patients (41 implants). These patients visited the clinic for clinical evaluation of the implant efficacy, using WOMAC pain and AKSS score.
Majority of the patients had severe pain and extensive stiffness on day 2 after surgery which is reflected in the low clinical AKSS scores (44.63±0.3) and functional AKSS scores (0). The clinical AKSS scored improved considerably at one-year follow up (90.0±3.04) and three-year follow up (93.0±4.10). The final outcomes at three-year follow up were significantly higher than the pre-operative scores (61.24±6.3) (p<0.5). The non-significant improvement in the clinical AKSS score between one-year follow up and three-year follow up suggest that the benefits of the TKR were sustained and even improved over the years. Functional AKSS scores also improved considerably at one-year follow up (90.13±4.60) and three-year follow up (95.24±23.39). Since weight bearing was not allowed immediately after the surgery, the postoperative functional AKSS score was 0 for all the patients. Complete clinical AKSS and functional AKSS scores are provided in the [Table/Fig-4].
American Knee Society Score.
| Variables | Pre-operative(N=191) | Postoperative(N=191) | 1-year followup (N=129) | 3-year followup (N=41) | p-value* |
|---|
| Clinical AKSS Score | 61.24±6.3 (23-79) | 44.63±0.3 (42-45) | 90.0±3.04 (57-98) | 93.0±4.10 (88-100) | <0.05 |
| Functional AKSS Score | 47±5.74 (20-45) | 0 | 90.13±4.60 (5-100) | 95.24±23.39 (15-100) | <0.05 |
| Range of motion (mean±SD) | 104±5.67° (range, 85°-119°) | 98±4.32° (92°-99°) | 120.78±4.18°(92°-121°) | 119.8±11.05° (98°-123°) | <0.05 |
*: comparison between preoperative and three-year follow up
The range of motion significantly improved from preoperative 104±5.67° (range, 85-119°) to 119.8±11.05° (98-123°) at follow up (p<0.05). The range of motion noted at other time intervals is given in [Table/Fig-4].
3.4 Pain and Stiffness Outcomes by WOMAC Scores
A significant improvement was noticed in the mean WOMAC pain and WOMAC stiffness scores at follow up as compared to the preoperative scores except at the two-day postoperative follow up [Table/Fig-5,6].
| WOMAC pain score |
|---|
| Score | Preoperative (N=191) | Postoperative(N=191) | 1-year follow up (N=129) | 3-year follow up (N=41) | p-value* |
|---|
| None (Score 0) | 0 | 0 | 62 (48%) | 25(61%) | <0.05 |
| Mild (Score 1) | 0 | 0 | 41 (31.8%) | 11(26.8%) | <0.05 |
| Moderate (Score 2) | 14 (7.3%) | 0 | 26 (20.2%) | 05(12.2%) | <0.05 |
| Severe (Score 3) | 121 (63.4%) | 2 (1%) | 0 | 00 (0%) | <0.05 |
| Extreme (Score 4) | 56 (29.3%) | 189 (99%) | 0 | 0 | <0.05 |
| WOMAC Score (mean±SD) | 3.2±0.57 (Range 2-4) | 3.8±0.2(Range: 3-4) | 1.02±0.75(Range 0-2) | 0.51±0.71 (Range 0-2) | <0.05 |
*: comparison between preoperative and three-year follow up
| WOMAC stiffness score |
|---|
| Score | Preoperative (N=191) | Postoperative(N=191) | 1-year follow up (N=129) | 3-year follow up (N=41) | p-value* |
|---|
| None (Score 0) | 0 | 0 | 71 (55%) | 36 (88%) | <0.05 |
| Mild (Score 1) | 0 | 0 | 44 (34.1%) | 03 (7%) | <0.05 |
| Moderate (Score 2) | 14 (7.3%) | 0 | 14 (10.8%) | 02 (5%) | <0.05 |
| Severe (Score 3) | 140 (73.2%) | 0 | 0 | 0 | <0.05 |
| Extreme (Score 4) | 37 (19.4%) | 191 (100%) | 0 | 0 | <0.05 |
| WOMAC Score (mean±SD) | 3.1±1.43 (Range 2-4) | 4.0±0 | 0.8±0.7(Range 0-2) | 0.16±0.48 (Range 0-2) | <0.05 |
*: comparison between preoperative and three-year follow up
The results of WOMAC pain score showed that at three-years follow up, 61% of patients were free from pain, while the prevalence of mild and moderate pain was observed in 26.8% and 12.2% patients respectively. No patient had severe pain at three-year follow up. About, 88% of the patients experienced good or excellent outcomes in terms of the absence of stiffness in the treated knee. A significant improvement was noticed for mean WOMAC pain and WOMAC stiffness scores at follow-up as compared to the preoperative scores.
Discussion
Reduction in pain, improving range of motion, and elevating life quality are the main aims of total knee replacement surgery. The current medical science is witnessing excellent outcomes with TKR because of the recent advancement in this field [9]. The state-of-the-art design of the Freedom Total Knee System has endorsed it as an excellent knee implant, which can be observed in the present study. Freedom Total Knee System has quickly gained a reputation of effective and safe knee implant among the orthopaedic community since its introduction in 2009 in India. The prime reason for the widespread appeal for the implant is because of its unique high-flexion design which also allows bone preservation. Furthermore, the implant is designed specifically as per the defined aspect ratio of the Pan-Asian knee anatomy and therefore provides smaller implants with different proportions [7].
Method of Fixation: Cemented, Uncemented Compon-ents vs. Hybrid
Implant fixation method holds a crucial role in predicting the sustainability of any knee implant since loosening is the most common reason for implant failure. Cemented technique allows secure fixation, fills gaps in the bone-implant interface, and resists compressive forces [10]. Radiostereometry Analyses (RSA) have made it possible to understand the different migration patterns shown by the TKR components with the two different fixation methods. Cementless tibial base plates have been observed to migrate from its position within three months of surgery while cemented implants show minute migration over 60 months postoperatively [11]. Furthermore, cementation of patellar components is highly crucial since cementless patellas are found to be associated with a high risk of failure due to early loosening of the component [12]. No differences have been demonstrated in the migration pattern of cemented with respect to cement-less femoral components. However, cementless femoral components reduce the risk of aseptic loosening due to defragmentation of the cement because of excessive wear and tear [12,13].
The Freedom Total Knee System implant requires hybrid fixation which means that cemented tibial and patellar components are combined with cementless femoral component (press-fit) and showed no cases of aseptic loosening, implant failure, and revision surgery. Similar, excellent performance of such hybrid fixation implants at three-year follow up is well established and reported in the literature [14,15].
Surgical Approach: Posterior Stabilized and Cruciate Retaining Approach
Debates continue on whether the posterior cruciate ligament should be retained or removed during the surgery. The cruciate retaining prosthetic offers improved bone preservation, more normal knee kinematics, increased proprioception, femoral rollback on the tibia during flexion, and greater stabilization of the prosthesis since the Posterior Cruciate Ligament (PCL) prevents anterior translation of the femur on the tibia [16]. Posterior stabilized implants replace the role of PCL using a polyethylene post and femoral cam which interact to inhibit anterior translation of femur on the tibia. Important advantages of this design are a less complicated procedure, a better and stable component interface [17,18] and improved range of motion [17,19,20].
The biggest advantage of using Freedom Total Knee System is that both the PS and CR freedom implants can be inserted using same instrumentation. This allows the interventional orthopedic to select the most suitable implant type for the patient without using different instrumentations.
All-Poly Fixed Bearing Tibial Component
Although Freedom Total Knee System implant are available in both All-poly as well as metal-backed tibial components, the present study only used the All-poly tibial implants. Extensive research in forms of meta-analysis which compared the mobile and fixed bearing tibial components have found no significant difference in regard to radiolucent lines, osteolysis, aseptic loosening [21], and survivorship [22]. Instead, the All-poly tibial components have been reported to reduce the cost of TKR procedure 24%-48% as compared to the metal-backed components [23]. Using All-poly tibial component thus allowed for cost saving to the patients without compromising on the performance.
Improved range of motion and relief from pain are the two most important measures of a successful total knee replacement [24-26]. Patient satisfaction is highly dependent on the range of motion as well as improved physical activity without pain [27]. Average flexion required for daily activities is 67° for swing phase of gait, 83° for climbing the stairs, 90° for descending stairs, and 93° for standing up from a chair [28]. Freedom Total Knee System evaluated by this study showed very good results in terms of the range of motion (119.8°±11.05), no pain (61%), and no stiffness (88%). The excellent outcomes for the range of motion are attributed to the high-flexion design of the femoral component with seven radii.
The postoperative knee functional score for Freedom Total Knee System was 95.24±23.39, and it was better than the well-recognised Buechel and Pappas Knee system (93.4) and NexGen-LPS (86.3) [9].
The study established the effectiveness and performance of the Freedom Total Knee System for total knee replacement in patients with osteoarthritis. The implant is most suitable for the Asian population, especially the Indian population who has social and philosophical needs for high knee flexion. High knee flexion is needed for daily activities such as using Indian style toilet, sitting cross legged while eating and at social gatherings, and performing religious activities such as reading namaz. Furthermore, the implant is designed with a background research of Pan-Asian knee anatomy aspect ratios and thus the implant is supposed to adequately fit the smaller and variably proportionate Indian patients. The All-poly tibial component allows for treatment cost reduction and therefore is suitable for young patient with active lifestyle who may require revision surgeries in future. The thin anterior flange of the femoral component minimizes overhanging over the anterior face of the femur, reduces overstuffing, reduces bone resection and prevents soft tissue impingement during extension and therefore is most suitable for patients with degenerative knee conditions such as osteoarthritis and rheumatoid arthritis.
Limitation
Small patient population and a relatively medium-length follow up period were the main limitations of the study. A study with a larger patient population followed up for longer duration of 10-15 years is required to establish long term efficacy, performance and survivorship of the knee implant.
Conclusion
The evaluation of Freedom® Total Knee System at a minimum of three years follow up showed good results in regard to the range of motion, reduced postoperative stiffness and pain, and improved functionality.