Intraductal Tubulopapillary Neoplasm: A New Entity in the Spectrum of Pancreatic Intraductal Neoplasms
Houcine Maghrebi1, Amin Makni2, Rami Rhaeim3, Alia Zehani4, Zoubeir Bensafta5
1 Consultant, Department of Surgery, Rabta Hospital, Tunis, Tunisia.
2 Professor, Department of Surgery, Rabta Hospital, Tunis, Tunisia.
3 Consultant, Department of Surgery, Rabta Hospital, Tunis, Tunisia.
4 Consultant, Department of Pathology, Rabta Hospital, Tunis, Tunisia.
5 Professor, Department of Surgery, Rabta Hospital, Tunis, Tunisia.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Houcine Maghrebi, 1007, Rue Djebel lakhdhar Tunis Service Dechirurgie, A-Hopital La Rabta, Tunis, Tunisia.
E-mail: dr_houcine@yahoo.fr
Intraductal Tubulopapillary Neoplasms (ITPN) is a rare and new entity defined as an intraductal, grossly visible, tubule-forming epithelial neoplasm with high- grade dysplasia and ductal differentiation without overt production of mucin. Its clinical presentation can be varied, which makes the diagnosis quite challenging. In this report, we present a case of pancreatic ITPN and review the published work to learn clinicopathological, radiological features and treatment strategies of this recently proposed pancreatic neoplasm.
Neoplasm, Oncology, Pancreas, Surgery
Case Report
A 62-year-old male patient with no previous medical history, presented to the emergency Department with epigastric pain associated with nausea and vomiting. Epigastric tenderness was noticed on physical examination. Routine laboratory tests were remarkable for the following abnormalities: Lipase 958 UI/l, Pancreatic amylase 1220 UI/l, Bilirubin 5 mg/l, Alanine aminotransferase 120 UI/l and C-reactive protein 25 mg/l. Abdominal ultrasound showed gallbladder microcalculi and a dilated main pancreatic duct. With these findings, biliary acute pancreatitis was diagnosed. CT scan revealed enlargement of the pancreatic gland. The main bile duct was slightly enlarged at its distal portion. The patient was discharged and scheduled for an Magnetic Resonance Cholangiopancreatography (MRCP). No treatment was given as the patient was not willing.
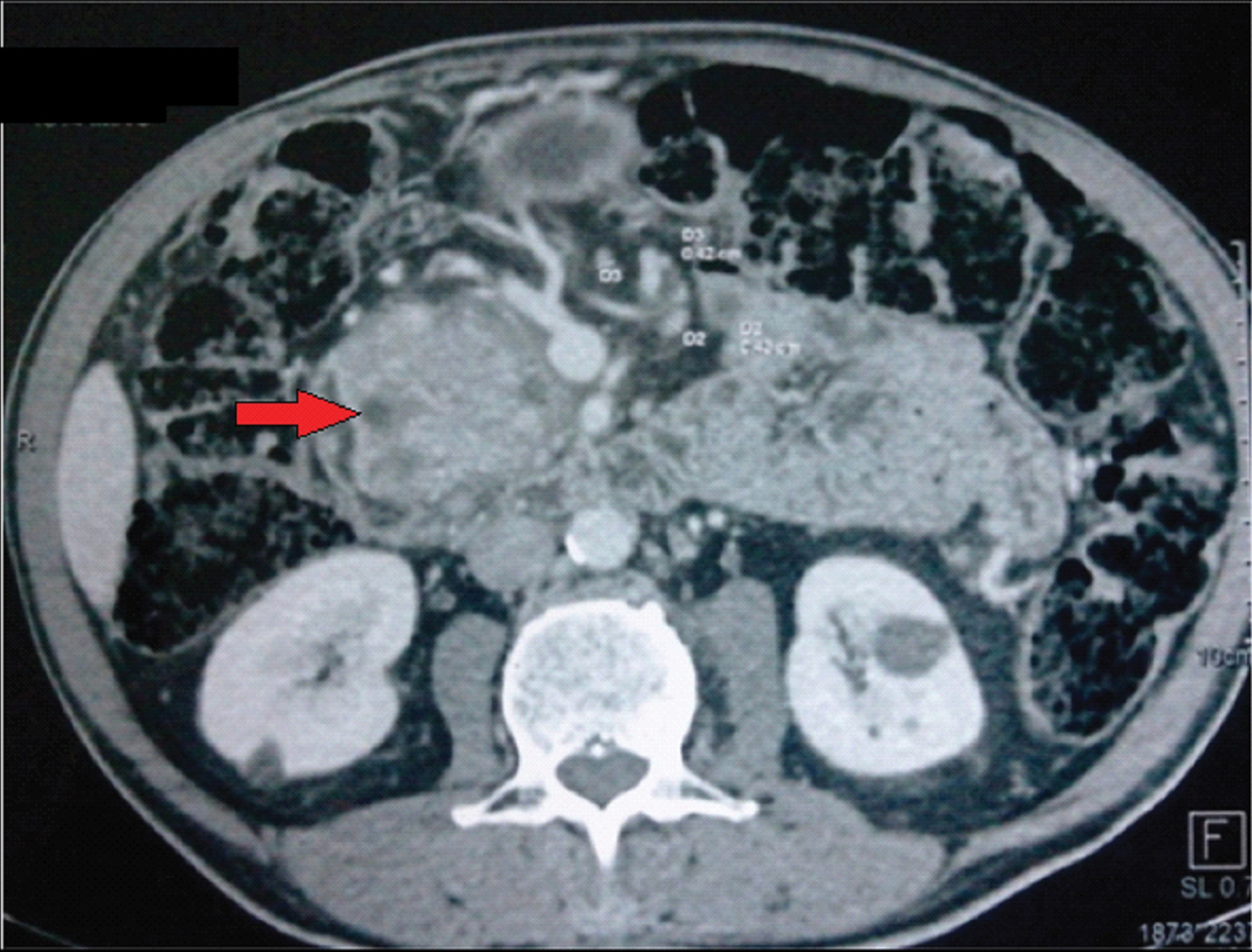
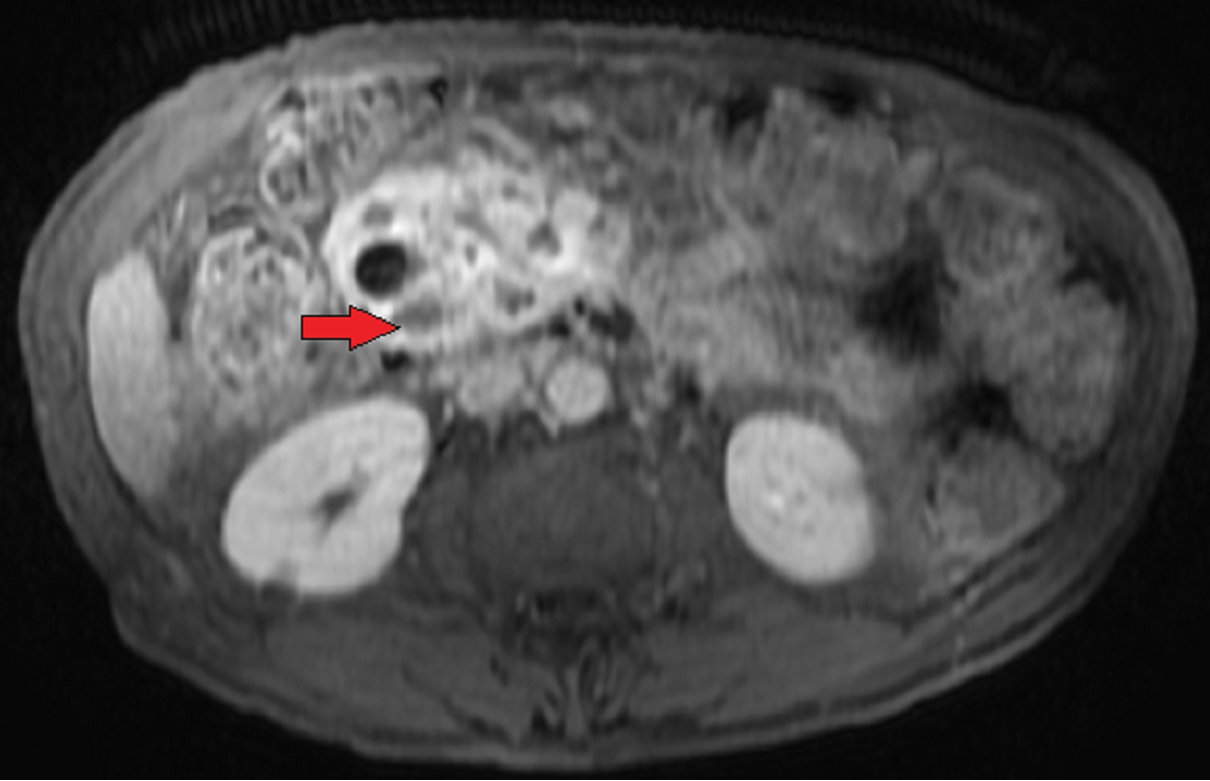
He was readmitted six months later with jaundice. CT scan [Table/Fig-1] was remarkable for a major dilation of the Wirsung duct associated to an enlargement of the main bile duct. MRCP [Table/Fig-2] showed enlargement of the pancreatic gland, multiple cystic lesions of the head of the pancreas with a major dilation of the main pancreatic duct. Intraductal hyperintense lesions were seen in the head, body and tail of the pancreas in the diffusion weighted images. There were no signs of liver or lung metastases. Endoscopic ultrasound with consideration for aspiration of cyst fluid was not done for logistical reasons. Lateral vision duodenoscopy failed to find mucinous output through the papilla. Carcinogenic embryonic antigen level was 5 UI/l. He was subsequently diagnosed with multifocal ITPN and underwent total pancreatectomy and splenectomy [Table/Fig-3].
Abdominal CT revealing enlargement of the pancreatic gland, dilatation of the main pancreatic duct and with multiple cystic lesions of the head (red arrow).
Magnetic Resonance (MR) image showing enlargement of the pancreatic gland with multiple cystic lesions of the head (red arrow).

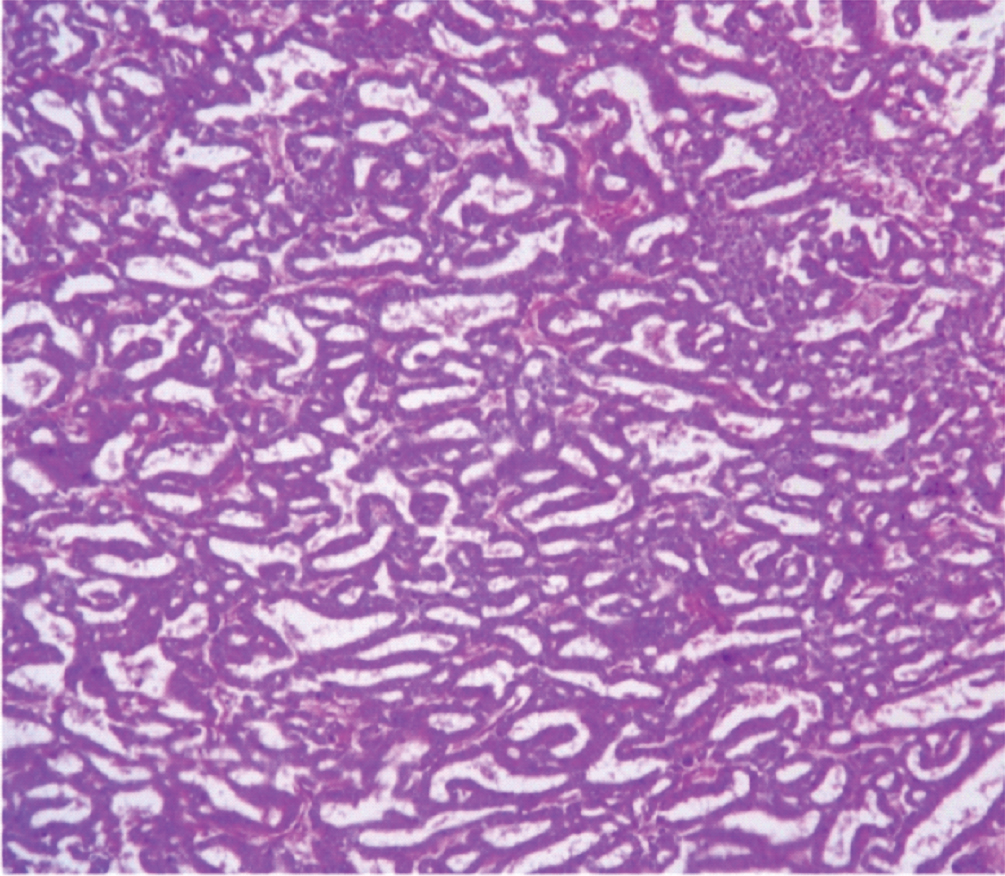
The procedure was undertaken through bilateral subcostal incision. The histology [Table/Fig-4,5] of the tumour revealed an ITPN of the pancreas.
Low power field of the specimen (H&E,4X).
High power field of the specimen (H&E 40X).
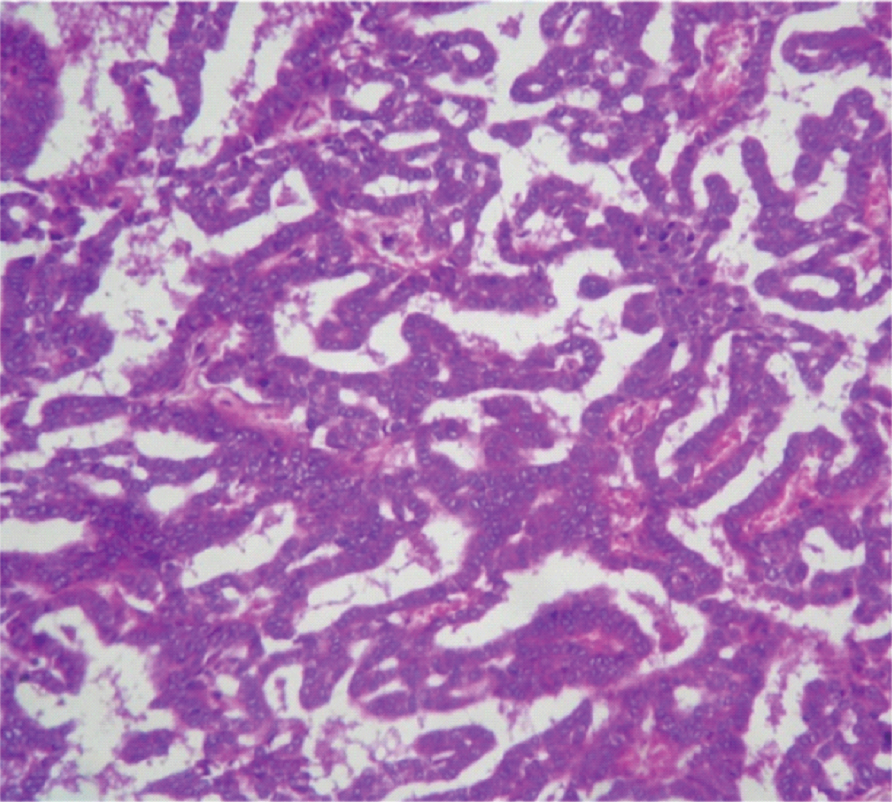
Macroscopically, multiple mixed tumours were seen in the head, body and tail of pancreas. Microscopically, there were solid proliferating tumour cells with tubular and papillary formation with high-grade dysplasia there was no lymph node metastasis. No mucin production was observed. Postoperatively, the patient had an uncomplicated course. He was started on pancreatic enzyme replacement therapy and insulin and then referred to the oncologic department. One year later, the patient remained asymptomatic with no signs of recurrence.
Discussion
ITPN is a rare and newly recognized intraductal pancreatic pathology [1,2]. It was first described by Yamaguchi et al in 2009 [3]. Klöppel G HR et al., in the WHO classification published in 2000, classified the pancreatic intraductal neoplasms into three groups [4]; Intraductal Tubular Neoplasms (ITN), Pancreatic Intraepithelial Neoplasm (PanIN) and Intraductal Papillary Mucinous Neoplasm (IPMN). Then in the most recent 4th edition of WHO classification, intraductal neoplasms of the pancreas were divided into two subtypes: IPMN and ITPN [2].
According to the 2010 WHO [2], ITPN are: ‘intraductal, grossly visible, tubule-forming epithelial neoplasm with high-grade dysplasia and ductal differentiation without overt production of mucin. ITPN constitutes <1% of all pancreatic exocrine neoplasms and only 3% of intraductal neoplasms of the pancreas [1]. Keiichi Date et al., published in 2016 a Literature review that revealed only 58 cases of ITPN in the pancreas [5]. ITPN occurs in an age range of 35–80 years and there is no sex predilection. Nearly half of ITPNs are located in the head of the pancreas, followed by the body and then the tail. Multifocal ITPN has also been reported. Tumours are usually slow growing and are therefore, relatively large at the time of diagnosis.
Its clinical presentation can be quite varied, which makes the diagnosis quite challenging The most common reported symptoms were abdominal pain, jaundice, exacerbation of diabetes mellitus, appetite loss, weight loss [1,6].
Our patient, presented to the emergency department with epigastric pain associated with nausea and vomiting. On imaging studies, it presented as a cystic lesion with a dilated and irregular main pancreatic duct. The difference with IPMN is the absence of low attenuation mucin. The differential diagnoses of ITPN are IPMN, Solid Pseudopapillary Neoplasm (SPN), pancreatic neuroendocrine tumour [7,8]. ITPN is a solid nodular tumour that obstructs dilated ducts on macroscopic examination. There is no visible secreted mucin. Cytology demonstrates closely apposed tubules that form cribriform complex structures in dilated pancreatic ducts with focal areas of papillary architecture. They have uniform high grade dysplasia and frequent mitotic figures [2].
Most ITPNs arise in the main pancreatic duct with ductal dilation while only about 5% of the cases arise in branch ducts [6]. The differential diagnosis for ITPN may also include intraductal acinar cell carcinoma. Immunohistochemistry studies may be helpful to differentiate IPMN from ITPN in rare cases that lack classic morphology or overlap histologically with IPMNs [9]. Typically, ITPNs are positive for cytokeratin (CK) 7, CK19, MUC1, and MUC6, and they are negative for MUC2, MUC5AC, trypsin, and b-catenin. IPMN, in comparison to ITPN, is usually positive for MUC-5AC but often negative for MUC-1. IPMN has a lower Ki-67 labeling index and KRAS-mutations are more common in IPMN compared to ITPN [10].
Compared with IPMNs, molecular genetic studies of ITPN are relatively limited due to the small number of cases available. In this case, although we did not do MUC immunostaining or laboratory studies on KRAS mutations, we reached at the diagnosis of ITPN mainly based on the macroscopic findings and morphological features
Because of the risk of malignancy, surgery and close clinical follow-up is generally recommended in order to improve the prognosis by detecting recurrences at an early stage. Pancreato-duodenectomy and distal pancreatectomy are the most frequent procedures.
Total pancreatectomy like our case is still rarely performed. Limited clinical follow-up data restricted an analysis of survival. However, these tumours generally have a favorable prognosis when completely excised.
Conclusion
ITPN still is a relatively new entity. The diagnosis can be challenging due to morphologic overlap with other intraductal lesions and its rarity. Further case series will allow to clarify its clinicopathological and molecular characteristics for the better understanding of the prognostic factors and treatment options.
[1]. Kasugai H, Tajiri T, Takehara Y, Mukai S, Tanaka J, Kudo S, Intraductal tubulopapillary neoplasms of pancreas: case report and review of literatureJ Nippon Med Sch 2013 80:224-29. [Google Scholar]
[2]. Adsay NV, Fukushima N, Furukawa T, Hruban RH, Intraductal neoplasms of pancreas; in Bosman FT, Carneiro F, Hruban RH, Theise ND (eds)World Health Organization Classification of Tumours of the Digestive System 2010 ed 4LyonIARC:304-13. [Google Scholar]
[3]. Yamaguchi H, Shimizu M, Ban S, Koyama I, Hatori T, Fujita I, Intraductal tubulopapillary neoplasms of the pancreas distinct from pancreatic intraepithelial neoplasia and intraductal papillary mucinous neoplasmsAm J Surg Pathol 2009 33:1164-72. [Google Scholar]
[4]. Klöppel G HR, Longnecker DS, Ductal adenocarcinoma of the pancreas. In: Hamilton SR, Aaltonen LA, editorsWHO classifications of tumours: Pathology and genetics of tumours of the digestive system 2000 IARC [Google Scholar]
[5]. Date K, Okabayashi T, Shima Y, Iwata J, Sumiyoshi T, Kozuki A, Clinicopathological features and surgical outcomes of intraductal tubulopapillary neoplasm of the pancreas: a systematic reviewLangenbecks Arch Surg 2016 401(4):439-47. [Google Scholar]
[6]. Yoshida Y, Matsubayashi H, Sasaki K, Kanemoto H, Uesaka K, Ono H, Intraductal tubulopapillary neoplasm of the pancreatic branch duct showing atypical imagesJ Dig Dis 2015 16(6):357-61. [Google Scholar]
[7]. Guan H, Gurda G, Lennon A, Hruban RH, Erozan YS, Intraductal tubulopapillary neoplasms of the pancreas on fine needle aspiration: case report with differential diagnosisDiagn Cytopathol 2014 42:156-60. [Google Scholar]
[8]. Furuhata A, Minamiguchi S, Mikami Y, Kodama Y, Sumiyoshi S, Adachi S, Intraductal tubulopapillary neoplasm with expansile invasive carcinoma of the pancreas diagnosed by endoscopic ultrasonography guided fine needle aspiration: a case reportDiagn Cytopathol 2013 42:314-20. [Google Scholar]
[9]. Kolby D, Thilen J, Andersson R, Sasor A, Ansari D, Multifocal intraductal tubulopapillary neoplasm of the pancreas with total pancreatectomy: report of a case and review of literatureInt J Clin Exp Pathol 2015 8(8):9672-80. [Google Scholar]
[10]. Chang X, Jiang Y, Li J, Chen J, Intraduc-tal tubular adenomas (pyloric gland-type) of the pancreas: clinicopathologic features are similar to gastric-type intraductal papillary mucinous neoplasms and different from intraductal tubulopapillary neoplasmsDiagn Pa-thol 2014 9:172 [Google Scholar]