The Indian Menopausal Society has projected that by the year 2025, there will be 103 million menopausal women in India. Lower age of menopause in India (47.5 years) combined with increasing life expectancy (71 years) forces the Indian women to spend approximately one-third of her life in menopause [1]. Hormonal fluctuations culminating in the Final Menstrual Period (FMP) begin at least a decade earlier and continue for much longer and are characterized by vasomotor symptoms, sleep disturbances, reduced fertility, irregular menstrual cycles, vaginal dryness and changes in skeletal and cardiovascular system [2]. These symptoms are no longer accepted as part of routine life [3].
HRT is the most effective therapy for the management of menopausal symptoms but they have fallen into disrepute post Women’s Health Initiative (WHI) findings of 2002 [4,5]. Women now do not want to take hormonal treatment out of fear of side effects and even the gynaecologists are reluctant in prescribing HRT post WHI. In view of this, large numbers of Complementary and Alternative Medicine (CAM) therapies have flooded the market and are being extensively used for the management of menopause related problems [6-8]. Majority of these therapies are based on soy isoflavones [9]. Soy isoflavones are phytoestrogens which have higher affinity for oestrogen β receptors. They bind strongly to oestrogen β receptors and weakly to oestrogen α receptors, thus exerting organ-specific oestrogenic or anti-oestrogenic activity by blocking the oestrogen receptor and possessing weak oestrogenic activity [10]. Their high consumption in the Japanese population was credited for lower rates of cardiovascular diseases, breast and endometrial cancer mortality and reduced vasomotor symptoms [11]. This led to the widespread use of non-hormonal therapies based on soy isoflavones for the management of menopausal symptoms though scientific evidence for their efficacy is mixed [12]. Studies have shown that menopausal symptoms vary with the menopausal stage, ethnicity, region and also show great inter-individual variation [13-15]. Moreover, the ability of women to metabolize the soy isoflavone, daidzein into the active equol is also not uniform among different ethnicities [12].
Though the Indian markets are flooded with soy isoflavone supplements, their efficacy in the management of menopausal symptoms among Indian women has not been tested. We planned this pilot study, to evaluate the impact of soy isoflavone supplementation on the Menopause Rating scale (MRS) scores among the heterogenous population of perimenopausal and postmenopausal Indian women.
Materials and Methods
Study Design
The pilot study was conducted as a questionnaire-based, observational, non-randomized, prospective open-labeled study over a period of one year (October 2012 to October 2013) at the Gynaecology OPD of a teaching hospital in Northern India. Institutional Ethical Committee clearance was sought before commencing the study and informed consent was taken from the patients participating in the study.
Sample
Keeping α error as 0.05 and power of the study at 95%, 50 patients were enrolled for the study. They were prescribed 100 mg soy isoflavone supplements per day for 12 weeks by the treating gynaecologist for menopausal symptoms. These patients were prescribed soy isoflavones solely based on the gynaecologists decision or because the patient refused HRT. In order to ensure that the diet did not contain any other soy based foods, they were given a list of foods to avoid during the three months of therapy. Newly diagnosed patients willing to come for follow up were included in the study. Patients who had previous treatment with hormonal treatment or soybean derived products in the previous 12 months were excluded from the study. We did not have any other exclusion criteria as the decision to prescribe soy isoflavones was solely the gynaecologists decision.
Study Tool
A pre-tested questionnaire consisting of three sections A, B and C was used. Section A investigated the description of sociodemographic data such as age, marital status, religion, education and occupational background. Section B dealt with the menstrual history in detail and evaluated the menstrual status of the patient according to the Stages of Reproduction Aging Workshop (STRAW) +10 criteria [16]. On the basis of these details, patients with no menstrual bleeding for the last 12 months were classified as postmenopausal. Similarly, patients with amenorrhoea for ≥60 days were late perimenopausal while those with irregular periods without skipping cycles and more than seven day difference in length of consecutive cycles were classified as early perimenopause state. Perimenopausal group in our study included both early and late perimenopause stages.
Section C of the questionnaire was the English version of the MRS questionnaire [17,18]. It is an internationally accepted tool for the evaluation of menopausal symptoms. It has also been validated as a tool to evaluate the response to therapy. The MRS questionnaire consisted of 11 common menopausal symptoms which are further grouped into three subscales: somatic, psychological and urogenital. Each of the 11 symptoms are scored from 0 (none) to 4 (very severe).
Though the questionnaire is a self-administered tool, it was administered by face-to-face interview in the local language by a postgraduate student to obtain data regarding the severity of menopausal symptoms. MRS questionnaire was used before starting therapy to record baseline symptoms and also after completing 12 weeks of therapy with 100 mg soy isoflavones.
Statistical Analysis
Independent t-test and paired t-test were applied to analyse the data using Statistical Package for Social Sciences (SPSS) software version 23.0 (SPSS Inc, Chicago, IL, USA). P<0.05 was considered as cut-off value for significance.
Results
According to the STRAW+10 criteria, of the 50 women enrolled, 29 were perimenopausal and 21 were postmenopausal. The mean age of the perimenopausal group was 42.28 (1.53) years and that of postmenopausal group was 49.62 (2.99) years. The mean age of attaining menopause in the postmenopausal group observed in our study was 45.48 (1.97) years. The average time since menopause was 4.14 (1.65) years. Most of the women belonged to middle socioeconomic group. The respondents in our study also had similar educational background.
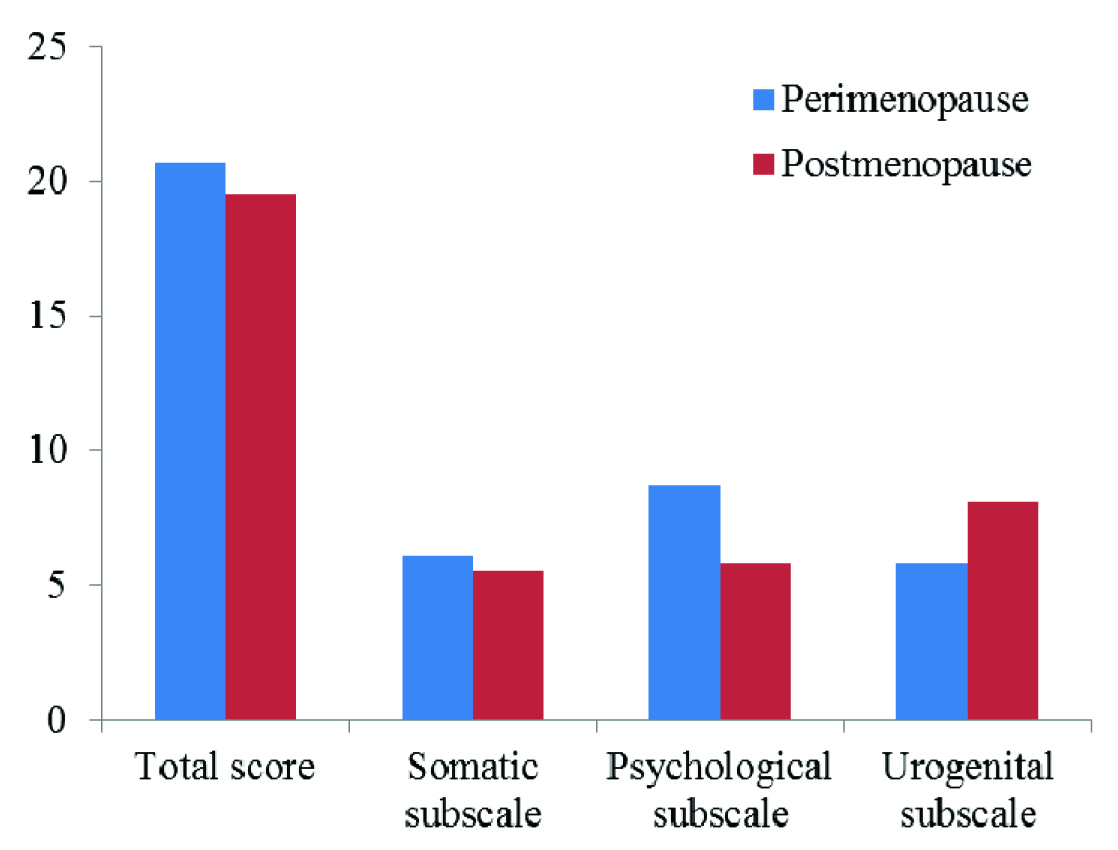
Reliability test of the MRS questionnaire was done using Cronbach’s alpha. The Cronbach’s alpha for somatic, psychological and urogenital subscales were 0.780, 0.724 and 0.627 respectively. At baseline, the mean total score of the perimenopausal and postmenopausal groups were comparable at 20.66 (4.36) and 19.57 (3.38) respectively. However, there was a significant difference between the psychological and urogenital scores (p<0.001) of both the groups [Table/Fig-1].
MRS score at baseline of perimenopausal and postmenopausal women.
Women of both the groups were started treatment with 100 mg soy isoflavone per day for 12 weeks. The MRS response of perimenopausal women showed a significant reduction in the mean total score by 19.55% and the somatic subscale score by 27.7% [Table/Fig-2]. Although the reduction in the urogenital subscale score by 1.19% was statistically significant (p<0.001), this decrease was clinically not significant. Among postmenopausal women, 12.62% improvement in mean total scores, 14.54% in somatic subscale and 26.79% in psychological subscale scores were significant [Table/Fig-3].
Mean MRS scores in perimenopausal group at baseline and after 12 weeks of therapy. Improvement of scores after therapy by absolute difference in scoring points.
| MRS domain | N | Scores before | Scores after | Absolute change | Percentage change |
|---|
| Total score | 29 | 20.66 | 16.62 | 4.04 | 19.55*** |
| Somatic subscale | 29 | 6.1 | 4.41 | 1.69 | 27.7*** |
| Psychological subscale | 29 | 8.7 | 6.41 | 2.29 | 26.32** |
| Urogenital subscale | 29 | 5.86 | 5.79 | 0.07 | 1.19*** |
**p<0.01, ***p<0.001
Mean MRS scores in postmenopausal group at baseline and after 12 weeks of therapy. Improvement of scores after therapy by absolute difference in scoring points.
| MRS domain | N | Scores before | Scores after | Absolute change | Percentage change |
|---|
| Total score | 21 | 19.57 | 17.1 | 2.47 | 12.62*** |
| Somatic subscale | 21 | 5.57 | 4.76 | 0.81 | 14.54*** |
| Psychological subscale | 21 | 5.86 | 4.29 | 1.57 | 26.79*** |
| Urogenital subscale | 21 | 8.14 | 8.05 | 0.09 | 1.11 |
***=p<0.001
On analysing individual symptoms, it was observed that the maximum improvement (40%) was seen in symptoms of hot flashes of mild to moderate degree in both perimenopausal and postmenopausal women. Severe to very severe hot flashes were seen only among perimenopausal women which improved by 36.11% after treatment. Severe fatigue which was the most common complaint of perimenopausal women showed a statistically significant improvement by 29.81% (p<0.001). Improvement in other symptoms of perimenopausal and postmenopausal women such as cardiac symptoms, rheumatoid complaints, depression, irritability and anxiety is summarized in [Table/Fig-4,5].
Mean improvement (in percentage) in the severity at baseline among perimenopausal women. ‘n’ denotes the number of patients.
| MRS scale symptoms | % Improvement in mild to moderate symptoms | % Improvement in severe to very severe symptoms |
|---|
| Hot flushes | 40 (n=10)** | 36.11 (n=9)*** |
| Cardiac symptoms | 31.3 (n=23)** | None had severe symptoms |
| Sleep disturbances | 15 (n=10) | 25 (n=4) |
| Depression | 32 (n=25)*** | None had severe symptoms |
| Irritability | 20.45 (n=22)** | 15.48 (n=7)* |
| Anxiety | 22.5 (n=20)** | 25.93 (n=9)** |
| Fatigue | 16.67 (n=3) | 29.81 (n=26)*** |
| Sexual dysfunction | No change (n=12) | 7.35 (n=17)* |
| Bladder disturbance | 2.63 (n=19) | No change(n=3) |
| Vaginal dryness | -5.77 (n=26) | No change (n=3) |
| Rheumatic complaints | 28.13 (n=16)** | 19.87 (n=13)** |
*p<0.05, **p<0.01, ***p<0.001
Mean improvement (in percentage) in the severity at baseline among postmenopausal women. ‘n’ denotes the number of patients.
| MRS scale symptoms | % Improvement in mild to moderate symptoms | % Improvement in severe to very severe symptoms |
|---|
| Hot flashes | 40.91 (n=11)* | None had severe symptoms |
| Cardiac symptoms | 18.81 (n=11)* | 33.33 (n=2) |
| Sleep disturbances | 26.92 (n=13) | None had severe symptoms |
| Depression | 25 (n=8)* | 16.67 (n=2) |
| Irritability | 21.43 (n=14)* | 33.33 (n=2) |
| Anxiety | 18.75 (n=16)** | None had severe symptoms |
| Fatigue | 12.5 (n=4)** | 31.37 (n=17)*** |
| Sexual dysfunction | No change (n=2) | 6.14 (n=19)* |
| Bladder disturbance | -11.54 (n=13) | No change (n=4) |
| Vaginal dryness | No change (n=2) | 3.51 (n=19) |
| Rheumatic complaints | 16.67 (n=3) | 7.41 (n=18)* |
*p≤0.05, **p≤0.01, ***p≤0.001.
Though the complaints of severe sexual dysfunction improved significantly among both perimenopausal (7.35%) and postmenopausal women (6.14%), other components of the urogenital subscale did not show any improvement [Table/Fig-4,5].
Discussion
Soy isoflavones are being extensively used for the management of menopausal symptoms. This study was undertaken to explore the extent to which the soy isoflavones improved the menopausal symptoms in the Indian women. The MRS scale was used for the evaluation of menopausal symptoms at baseline and after 12 weeks of treatment with 100 mg soy isoflavones per day. This study showed that there was no significant difference in the mean total scores of the perimenopausal and postmenopausal women at baseline. Though the somatic subscale scores were comparable between both the groups, the psychological subscale scores were significantly higher during perimenopause while the urogenital symptoms were significantly more severe in the postmenopausal period. Similar findings were reported from numerous other studies [13,19,20].
Perimenopausal Women
In this study, among perimenopausal women, the baseline scores were highest for the psychological domain which improved by 26.32% after treatment (p<0.01). Almost 90% of the perimenopausal women complained of severe to very severe symptoms of fatigue which reduced by 30% at the end of 12 weeks of therapy with p<0.001. Animal studies have also demonstrated the anti-fatigue action of soy isoflavones in mice but the underlying mechanism at the cellular level for the anti-fatigue benefit of soy isoflavones is still not clear [21]. In this study group, 86% had mild to moderate depressive symptoms, which improved by 32%. Other large scale studies evaluating mood changes during menopause have shown that the risk of depression is high during the perimenopause [22]. Moreover, depression during menopausal transition is influenced by previous episodes of premenstrual syndrome or postpartum depression, hot flashes, nocturnal sweating, insomnia, socioeconomic strata and ethnicity. The depression during the climacteric was more resistant to treatment with conventional antidepressants [23]. Studies evaluating the antidepressant effect of 100 mg soy isoflavone given for three months had found it to enhance the response to sertraline (50 mg) in the treatment of mood disorders in menopausal women [24]. Another two year long study conducted in Italy among 200 menopausal women found that improvement in mood disorders with soy isoflavone genistein (54 mg/day) to be significantly greater than placebo [25]. This study provides further evidence that soy isoflavones can be used as add-on therapy to help alleviate menopause associated depressive symptoms.
The somatic scores improved by 27.7% after treatment with soy isoflavones. All the components of the somatic subscale showed improvement. Of the 29 perimenopausal women, 19 patients complained of hot flashes. The aetiology of hot flashes during menopause was unclear. It has been hypothesized that a relative decrease in circulating oestrogen levels alters the norepinephrine and serotonin levels, thus causing dysfunction of the thermoregulatory nucleus [26]. Results of randomized controlled trials exploring the beneficial effects of soy isoflavones have been mixed [27-29]. A randomized placebo controlled double-blinded trial conducted over 12 weeks with 90 mg of soy isoflavone did not demonstrate any difference in soy based treatment and placebo, both in the frequency and severity of hot flushes. Though, there was significant improvement in both the groups from the baseline, it was attributed to strong placebo effect [28]. However, a meta-analysis of 17 trials revealed that soy isoflavones (54 mg) given for six weeks to 12 months significantly reduced the frequency of hot flashes by 20.6% and the severity improved by 26.2% compared to placebo [29].
Joint pains and other rheumatic complaints also showed a significant improvement in this study. Though effect of soy isoflavone on calcium metbolism was uncertain, there was some evidence of efficacy of soy isoflavone in improving postmenopausal bone health and markers of osteoporosis [30,31]. Studies have also demonstrated that soy intake improved symptoms and biochemical markers of osteoarthritis [32].
Though the improvement in urogenital score was statistically significant, it was not clinically significant. There was no change in symptoms of bladder dysfunction and vaginal dryness. In some cases, these symptoms even progressed during the treatment duration. Similar results were demonstrated by other studies also [12]. Studies have shown that soy isoflavones do not have any effect on the urogenital symptoms and vaginal maturity index [33]. The small improvement seen in this study could be attributed to the improvement in the sexual dysfunction. One reason for this could be that as the symptoms of hot flashes and depression improves, there could be a small improvement in libido.
Postmenopausal Women
With change in menopausal status, the symptoms changed with respect to frequency and severity in this study. The most important complains of the postmenopausal women belonged to the urogenital domain. These findings were similar to other studies [13]. Even after 12 weeks of treatment with soy isoflavones, there was no improvement in symptoms of vaginal dryness or bladder dysfunction. Falling oestrogen levels caused changes in the vaginal environment which predisposes to recurrent urinary tract problems and consequent bladder disturbances. Soy isoflavones as also shown by other studies did not had any effect on the vaginal health [33]. The small but significant improvement in sexual dysfunction in our study can be due to improvement in hot flashes as discussed earlier.
The improvement in psychological subscale score by 26.79% was highly significant (p<0.001). However, the baseline symptoms of depression, irritability and anxiety were mostly of mild to moderate degree and improved by 25%, 21% and 19% respectively. Maximum improvement was seen for severe symptoms of fatigue (31%). Similar extent of improvement was seen among the perimenopausal women also. Studies have demonstrated the beneficial effect of soy isoflavones on menopausal mood symptoms and fatigue [21,24,25].
With increasing age and menopausal status, the frequency and severity of hot flashes decreased. After three months of therapy, mild symptoms showed an improvement of 40% (p<0.05). The most important complain belonging to the somatic subscale among the postmenopausal women in this study were the rheumatic complains. Studies have shown that bone loss is rapid during early years following menopause. Soy isoflavones are thought to act as Selective Estrogen Receptor Modulators (SERM) in the management of osteoporosis [34]. In the present study, rheumatic complains showed a marginal improvement of 7.4% after three months of therapy with soy isoflavones (p<0.05). This small improvement could be due to other confounding dietary factors like calcium, vitamin D and protein which are known to directly affect bone health. Though, some studies have demonstrated no effect of soy isoflavones on calcium metabolism, others have shown an improvement in lumbar BMD and a decrease in fracture risk [30,31].
Limitation
However, the present study had some limitations. Firstly, it was designed as a non-randomized observational study. The results in this study need to be confirmed by a randomized controlled trial. Secondly, MRS questionnaire was administered by a postgraduate student in the local language. Some bias is to be expected because of this.
Conclusion
This study provides evidence of potential benefits of soy isoflavones on improving the MRS score both among the perimenopausal and postmenopausal women. As they are most effective on the somatic and psychological symptoms, their use is more beneficial during perimenopause. Postmenopausal women mostly complain of urogenital symptoms which are unaffected by soy isoflavone use.
**p<0.01, ***p<0.001
***=p<0.001
*p<0.05, **p<0.01, ***p<0.001
*p≤0.05, **p≤0.01, ***p≤0.001.