Bilateral Conjunctival Rhinosporidiosis in a Paediatric Patient
Charudutt Kalamkar1, Amrita Mukherjee2
1 Consultant, Department of Ophthalmology, Shri Ganesh Vinayak Eye Hospital, Raipur, India.
2 Consultant Department of Ophthalmology, Shri Ganesh Vinayak Eye Hospital, Raipur, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Charudutt Kalamkar, Shri Ganesh Vinayak Eye Hospital, Opposite Colors Mall, Opposite Ganga Diagnostic, Dhamtari Road, Raipur-492001, India.
E-mail: charudutt03@yahoo.co.in
Conjunctival mass, Endospores, Sporangial sac
Rhinosporidiosis occurs predominantly in tropical climate with contaminated pond water being a common source of infection. It can occur in any age group and commonly involves nasal mucosa, conjunctiva and lacrimal sac.
A nine-year-old boy presented in Ophthalmology Out Patient Department (OPD) with bilateral conjunctival mass lesions. Best Corrected Visual Acuity (BCVA) in both eyes (Oculus Uterque:OU) was 6/6, N.6. The masses were painless and were slowly progressing in size for the past one month. He belonged to rural area and gave a history of bathing in pond water daily.
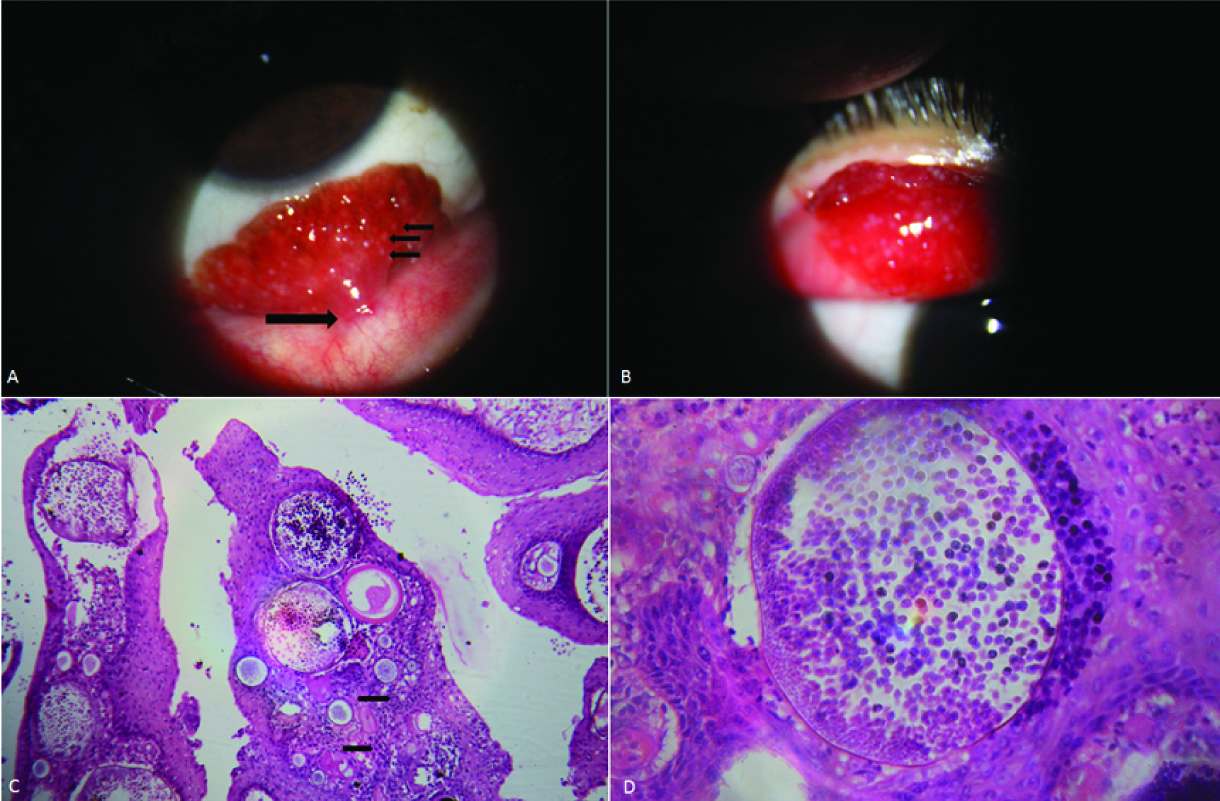
Right eye (OD) examination revealed fleshy polypoidal mass (12 mm x 8 mm) arising from palpebral conjunctiva of the lower lid [Table/Fig-1a]. Left eye had similar pedunculated mass (10 x 6 mm) arising from tarsal conjunctiva of the upper lid [Table/Fig-1b]. Slit lamp examination revealed red coloured mass with irregular surface with multiple yellowish dots on surface [Table/Fig-1a,b]. The fleshy head of the mass was attached to conjunctiva through a stalk. Surrounding conjunctiva appeared healthy in both eyes OU. Rest anterior and posterior segment evaluation was normal. Otolaryngological examination was normal.
Slit lamp biomicroscopy image and Hematoxylin and Eosin (H&E) stained histo-pathological sections:
(a) Slit lamp image of Right eye showing fleshy pedunculated mass with Stalk (Long Black arrow) arising from palpebral conjunctiva of lower lid. Surface of lesion having numerous yellowish dots on surface overlying sporangia (Small Black Arrows).
(b) Slit lamp image of Left eye demonstrating polypoidal mass having numerous yellowish dots on surface arising from upper lid tarsal conjunctiva.
(c) Multiple sporangia in different stages of development filled with endospores. (H&E x10) Inflammatory cell infiltrates in surrounding stroma (Small Black Arrows)
(d) Thick walled sporangial sac filled with numerous endospores surrounded by inflammatory cells. (H&E x40)
In OU, the pathological masses were surgically excised and bases were cauterized. Topical gatifloxacin (0.3%) eye drops were administered for seven days. Patient was advised to stop bathing in pond water.
Histopathological examination showed multiple sporangial sacs, at various stages of development, filled with endospores confirming the diagnosis of rhinosporidiosis [Table/Fig-1c,d]. Sporangial sacs were surrounded by inflammatory cell infiltrates in a fibrovascular stroma [Table/Fig-1c]. No recurrence till last follow up at six months post surgery was observed. Informed consent was obtained and the study was adhered to the tenets of the Declaration of Helsinki.
Rhinosporidiosis is caused by Rhinosporidium seeberi, which was earlier classified as fungus, but is now considered in Mesomycetozoea class [1]. It is most commonly found in tropical climate with majority of cases being reported from the Indian subcontinent. In a retrospective study of histopathalogical analysis of ophthalmic lesions in Central India, Rhinosporidiosis consisted of 23.2 % of eyelid lesions [2]. Contaminated pond water is a common source of this organism, which enters the mucosa after minor trauma or abrasion. Mucosa of nose and nasopharynx are the most common sites of involvement, followed by eye [3]. Apart from pedunculated palpebral conjunctival mass, it also involves lacrimal sac or have atypical presentations such as scleral thinning, staphyloma and conjunctival cyst [4,5]. Rhinosporidiosis has also been reported from non endemic region in a paediatric patient by Arora R et al., [6]. Similar to our case, Nair AG et al., described an eight-year-old child with rhinosporidiosis of tarsal conjunctiva treated successfully by surgical excision with cauterization of the base [7]. Ganekal S et al., have also reported pedunculated upper palpebral conjunctival rhinosporidial lesion in a paediatric patient treated by excision alone [8].
Common differentials include chalazion, conjunctival papilloma and pyogenic granuloma. Presence of bilateral pedunculated conjunctival lesions should alert the ophthalmologist to look closely for typical slit lamp appearance. Specific history of bathing in contaminated water should be asked for in all such cases. Typical appearance of the lesion with histopathological demonstration of sporangial sacs filled with endospores helps in differentiating rhinosporidiosis from other similar appearing lesions. Treatment consists of excision of mass with or without base cauterization. Oral medications like dapsone, ketoconazole, trimethoprime-sulphadiazine have been used to prevent recurrences.
In conclusion, rhinosporidiosis should be considered in the differential diagnosis of bilateral fleshy conjunctival mass lesions in paediatric age group. People in rural areas should be cautioned against bathing in pond water.
[1]. Mendoza L, Taylor JW, Ajello L, The class mesomycetozoea: A heterogenous group of microorganisms at the animal-fungal boundaryAnnu Rev Microbiol 2002 56:315-44. [Google Scholar]
[2]. Gupta Y, Gahine R, Hussain N, Memon MJ, Clinico-pathological spectrum of ophthalmic lesions: an experience in tertiary care hospital of central IndiaJournal of Clinical and Diagnostic Research : JCDR 2017 11(1):EC09-EC13. [Google Scholar]
[3]. Sudarshan v, Goel NK, Gahine R, Krishnani C, Rhinosporidiosis in Raipur, Chhattisgarh: A report of 462 casesIndian J Pathol Microbiol 2007 50(4):718-21. [Google Scholar]
[4]. Jhon SS, Mohandas SG, Conjuntival oculosporidiosis with scleral thinning and staphyloma formationIndian Journal of Ophthalmology 2005 53:272-74. [Google Scholar]
[5]. Lavaju P, Arya SK, Kumar B, Upadhyaya P, Conjunctival rhinosporidiosis presenting as a cystic mass-an usual presentationNepal J Ophthalmol 2010 2(2):157-59. [Google Scholar]
[6]. Arora R, Ramachandran V, Raina U, Mehta DK, Oculosporidiosis in Northern IndiaIndian Pediatr 2001 38(5):540-43. [Google Scholar]
[7]. Nair AG, Ali MJ, Kaliki S, Naik MN, Rhinosporidiosis of the tarsal conjunctivaIndian Journal of Ophthalmology 2015 63(5):462-63. [Google Scholar]
[8]. Ganekal S, Dorairaj S, Hegde S, Jhanji V, Conjunctival rhinosporidiosisJ AAPOS 2013 17(4):432-33. [Google Scholar]