T1DM is a chronic inflammatory disease characterized by diminished insulin secretion due to damage to islets of Langerhans in the pancreas [1]. Approximately, 90% of diabetes in children and adolescents is of Type 1 [2]. The prevalence of vitamin D deficiency is as high as 50-90% in the Indian population and is attributed to increased melanin content of skin and increasing urbanization with an indoor lifestyle [3]. Moreover, children with T1DM have a predisposition towards vitamin D deficiency as compared to general population [4]. In addition to immunoregulatory functions, insulin gene expression in pancreatic beta-cells may also be modulated by Vitamin D, thereby regulating insulin secretion [5]. Similar intervention studies by Gabbay et al., Aljabri et al., have demonstrated favourable changes in HbA1c, C-peptide, insulin dose and insulin sensitivity in patients supplemented with Vitamin D [6,7]. However, Pitocco et al., and Bizzari et al., found no beneficial effect of Vitamin D on C-peptide or HbA1c levels [8,9].
This randomized controlled trial was conducted to further evaluate the role of Vitamin D as an adjuvant in improving glycaemic control and residual pancreatic beta-cell function in children with T1DM. Primary outcome was the mean change in HbA1c levels over a period of six months.
Materials and Methods
This randomized controlled trial was conducted at JIPMER, a tertiary care teaching hospital, South India during the period of August 2014-15 for one year. Due approval from Institute Ethics Committee (IEC) was obtained and was registered in Clinical Trials Registry of India (CTRI/2014/07/004739), after informed consent from parents, children (1-18 years of age) with T1DM attending the Paediatric endocrinology clinic were enrolled. Confirmation of Type 1 diabetes was based on: dependence on insulin for diabetes control from time of diagnosis, Diabetic ketoacidosis or marked ketonuria at time of clinical onset, lack of obesity, and Acanthosis Nigricans. However, those with one or more of the following criteria were excluded: children already on Vitamin D supplements for preceding one month, Malabsorption syndrome, primary or secondary immunodeficiency, Renal stones, Chronic kidney disease, Adrenal tumours and children on steroid therapy for more than 2 weeks. The same inclusion and exclusion criteria was followed for selection of both cases and controls. Stratified random sampling was done using age strata as follows: 1-3 years, 4-8 years, 9-18 years. Allocation concealment was done using pre-printed randomization sequences kept in opaque sealed envelopes. The principal investigator and lab personnel were blinded to the group allocation. The intervention and standard of care arm consisted of 26 participants each. Oral Vitamin D therapy was administered in addition to insulin in intervention arm while only insulin was continued for the other arm.
The primary outcome variable taken was the decrease in HbA1c levels at 6 months after the intervention, for sample size calculation. A similar study from Saudi Arabia [7] showed that Vitamin D supplementation for 12 weeks reduced HbA1c by 10% with a standard deviation of 2.4. It was estimated that 24 patients in each group would be required to achieve 80% power; α=0.05 and two sided 95% CI to detect a mean difference of 2 % in HbA1c between the 2 groups. Adjusting for an attrition of 20%, a total of 56 patients were required to be enrolled.
The demographic parameters, body mass index, details regarding insulin therapy including daily requirement and compliance to insulin therapy and Self Monitoring of Blood Glucose (SMBG) were noted for all children. Oral Vitamin D therapy was administered once a month for 6 months in addition to insulin in intervention arm while only insulin was continued for other arm. Vitamin D (cholecalciferol) 60,000 IU tablets (Mfd. by Mankind, India) were used. Vitamin D dosage was calculated using upper limit of Vitamin D intake as per American Association of Paediatrics guidelines, 2011 [10] i.e., 1-3 years-60,000 IU, 4-8 years-90,000 IU, 9-18 years-1,20,000 IU. An adequate dietary calcium intake was ascertained through dietary recall. Plasma HbA1c, serum 25-OHD and C-peptide were measured at baseline and repeated after 6 months. Serum 25-OHD levels were measured by ELISA (Mfd. MicroVue - California, USA) Plasma HbA1c (normal range 4%-6.5%) was measured by High Performance Liquid Chromatography (Bio-Rad D-10™ Haemoglobin A1c analyser, USA). Serum C-Peptide was measured using ELISA kits (Mfd. DRG International, Inc., USA).
Parents and older children were counselled regarding importance of compliance to insulin therapy and SMBG at home. A free glucometer and a blood glucose monitoring notebook were issued to each parent, along with a diabetic diet chart and a diabetes information handout for the parents. Compliance to SMBG was defined as five point monitoring i.e. monitoring blood glucose five times on one specific day of the week i.e., pre breakfast, pre-lunch, pre-dinner, two hours post dinner, and 2 am. Insulin doses were titrated by a team of paediatricians and endocrinologists not involved in the study. All children followed up monthly for a total duration of 6 months. Parents were contacted over phone if the monthly follow up was missed. Pill adherence was assessed by a self-report on the basis of pill counts. All children in intervention arm were monitored for symptoms and signs of Vitamin D toxicity (vomiting, polyuria and gastritis) at each follow up. Serum Calcium and Urinary Calcium/ creatinine ratio was done at 3 and 6 months follow-up. Urinary calcium/ creatinine ratio less than 0.2mg/dl was considered normal.
Per-protocol analysis was done. Quantitative data like 25-OHD levels, HbA1c, C-peptide, Insulin dose/day were represented using mean±SD. Analysis of quantitative data between two groups was done using unpaired t-test if data passed ‘Normality test’ and by Mann-Whitney test if data failed ‘Normality test’. A p-value<0.05 was considered significant. SPSS Version 17 was used for data analysis.
Results
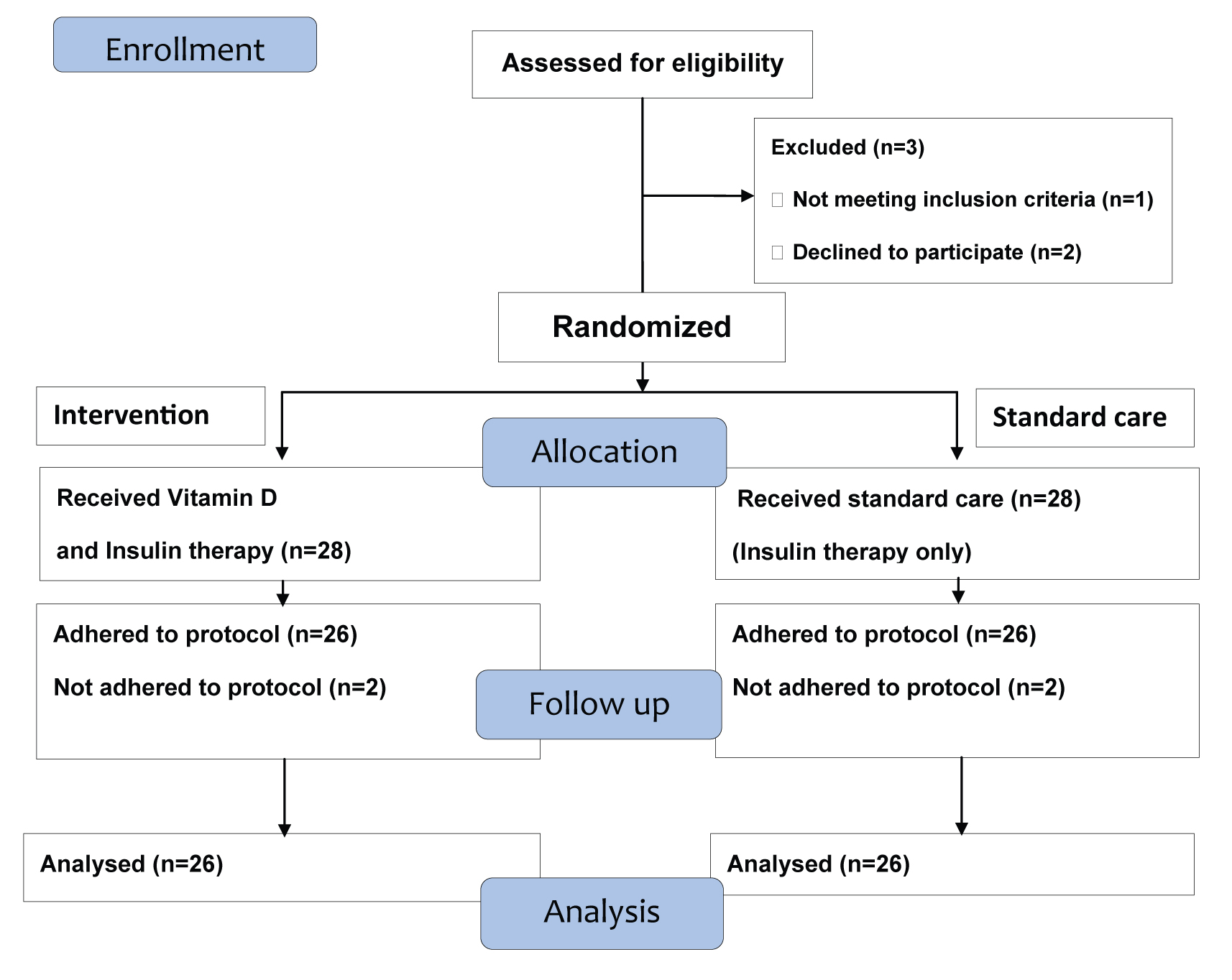
In our study, 56 children were found eligible and were randomized to the two arms (intervention and standard of care). In view of failure to adhere to protocol, two children were removed from each arm and data of 52 children were analysed [Table/Fig-1]. The baseline characteristics of children in both arms are described in [Table/Fig-2]. As high as 63.5% children with T1DM (33 of total 52) were Vitamin D deficient i.e., serum 25 OHD < 20 ng/ml [11]. Six months supplementation of Vitamin D caused significant rise in serum vitamin D levels to sufficient range in intervention arm with mean serum 25-OHD level of 68.64 ng/ml. The outcome variables observed after 6 months are depicted in [Table/Fig-3]. The mean C-peptide levels showed a significant rise in the intervention arm as compared to standard of care arm (p <0.05) at the end of 6 months. No adverse events due to Vitamin D therapy were noted.
Baseline characteristics of children in both arms.
| Characteristics | Intervention arm | Standard of care arm | p-value |
|---|
| Mean Age (years) (SD) | 9.5 (3.9) | 9.0 (4.4) | 0.67 |
| Male: Female | 14:12 | 13:13 | |
| Duration of diabetes (years) (SD) | 4.75 (3.0) | 4.0(2.5) | 0.84 |
| BMI (kg/m2) | 22.6 | 24.2 | 0.57 |
| Compliance to SMBG (%) | 38.5% | 42.5% | 0.92 |
| Type of Insulin | | | |
| Pre-mixed(70:30 NPH :Regular) | 61.5% | 53.8% | 0.62 |
| NPH with Regular(Basal-bolus) | 19.2% | 30.8% | 0.24 |
| Glargine with Regular(Basal-bolus) | 19.2% | 15.4% | 0.48 |
| Mean 25-OHD levels (ng/ml) (SD) | 20.7(10.5) | 19.7(11.8) | 0.75 |
| Mean HbA1c (%) (SD) | 10.2 (2.5) | 10.7 (3.3) | 0.58 |
| Mean Insulin requirement(U/kg/day) (SD) | 1.19 (0.3) | 1.03 (0.3) | 0.15 |
| Mean C-peptide levels (ng/ml) (SD) | 0.3 (0.1) | 0.4 (0.3) | 0.057 |
Outcome variables after 6 months.
| Variables | Intervention arm | Standard of care arm | p-value |
|---|
| Mean 25-OHD levels (ng/ml) (SD) | 68.64 (24.2) | 19.13 (7.9) | <0.01 |
| Mean HbA1c (%) (SD) | 9.82 (1.8) | 10.69 (2.4) | 0.147 |
| Mean Insulin requirement(U/kg/day) (SD) | 1.15 (0.49) | 1.01 (0.36) | 0.19 |
| Mean C-peptide levels (ng/ml) (SD) | 0.51 (0.29) | 0.33 (0.24) | <0.05 |
Discussion
This is one of the few intervention studies using Vitamin D as adjuvant for children with T1DM especially in the Indian context. Children recruited in both arms of this study were similar in terms of the mean age, sex, body mass index, duration of disease, diabetes medication, daily insulin requirement, Vitamin D status, mean HbA1c levels and C-peptide levels at baseline. Vitamin D deficiency was noted in 63.5% of the study population. Higher prevalence of Vitamin D deficiency in T1DM patients has been documented in similar studies [4]. As Vitamin D deficiency is very common among paediatric population, its supplementation may be useful in general for all children including those with T1DM.
The mean change in HbA1c trends towards a greater reduction in the intervention arm than the standard of care arm after 6 months. However, the reduction was not statistically significant. In a similar study in Saudi Arabia, significantly lower HbA1c was achieved in Vitamin D deficient T1DM patients when 25OHD level reached >75 nmol/L at end of 12 weeks [7]. A recent study from Egypt found that better glycaemic control was achieved when Vitamin D was supplemented for 3 months in Vitamin D deficient T1DM patients, albeit no reduction in insulin requirement [12]. Another study from Iran demonstrated a lower mean HbA1c after Vitamin D deficient T1DM patients received a mega dose of Vitamin D (3 Lac IU) intramuscularly [13].
In our study, the mean C-peptide levels showed a significant rise in the intervention arm as compared to standard of care arm (p <0.05) at the end of 6 months, indicating improved beta-cell function. Gabbay et al., have demonstrated a slower rate of decline in C–peptide levels, significant fall of HbA1C levels in 6 months, and a significant decrease in GAD65 antibody titres in T1DM patients after supplementing 2000 IU/ day Vitamin D for18 months [6].
C-peptide acts as a surrogate marker of residual β-cell function as it is coupled with insulin release [14]. A boost to insulin synthesis and secretion by Vitamin D can be explained by the presence of the vitamin D response element in the human insulin gene promoter region and activation of transcription of the human insulin gene by 1,25- dihydroxyvitamin D [15]. Even a slight increase in C-peptide levels has been shown to reduce long-term complications of T1DM [16].
The daily insulin dose requirement did not show a significant difference between the two groups at 6 months follow up.
Limitation
Major limitations of this study were the non-standardized insulin regimen, use of different types of insulin analogs, relatively small sample size, and the short duration of the study.
The role of Vitamin D as an immunomodulator needs to be further researched in T1DM patients, preferably in a larger sample size and for a longer duration.
Conclusion
This study shows that oral Vitamin D may serve as an adjuvant for insulin therapy in children with T1DM by the augmentation of beta cell function and insulin secretion. However, tangible results in the form of better glycaemic control and decreased requirement for exogenous insulin were not achieved.