Foreign Body Aspiration: An Unusual Presentation and Outcome
Surabhi Jaggi1, Anuj Kumar2, Kranti Garg3, Deepak Aggarwal4, Reetu Kundu5
1 Junior Resident, Department of Pulmonary Medicine, Government Medical College and Hospital, Sector 32 A, Chandigarh, Union Territory, India.
2 Junior Resident, Department of Pulmonary Medicine, Government Medical College and Hospital, Sector 32 A, Chandigarh, Union Territory, India.
3 Assistant Professor, Department of Pulmonary Medicine, Government Medical College and Hospital, Sector 32 A, Chandigarh, Union Territory, India.
4 Associate Professor, Department of Pulmonary Medicine, Government Medical College and Hospital, Sector 32 A, Chandigarh, Union Territory, India.
5 Assistant Professor, Department of Pathology, Government Medical College and Hospital, Sector 32 A, Chandigarh, Union Territory, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Anuj Kumar, House No. 2183, Sec 44C Chandigarh-160047, Union Territory, India.
E-mail: dranujsoni87@yahoo.com
Foreign body aspiration mostly presents as acute emergency with cough, choking and dyspnoea. Rarely aspiration of foreign body may be the underlying cause in patients presenting with long term symptomatologies. Here is a case of 60-year-old male who came for surgical management of cholelithiasis. During his workup, X-ray chest revealed right paracardiac opacity. Fibre-optic bronchoscopy showed a mass lesion in right main bronchus. It was taken out of the airways by flexible bronchoscope but could not be retrieved. Subsequent chest radiographs showed marked improvement.
Flexible bronchoscopy, Paracardiac opacity, Right main bronchus
CASE REPORT
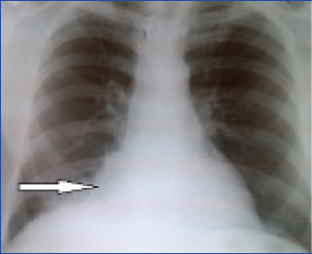
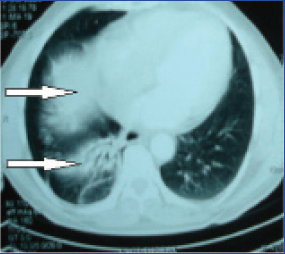
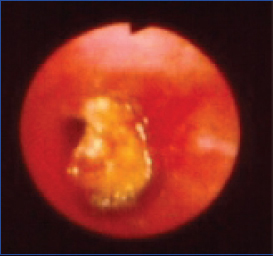
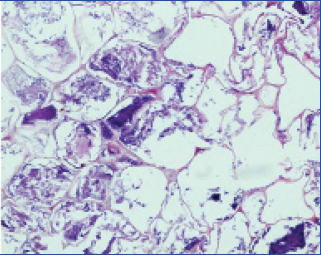
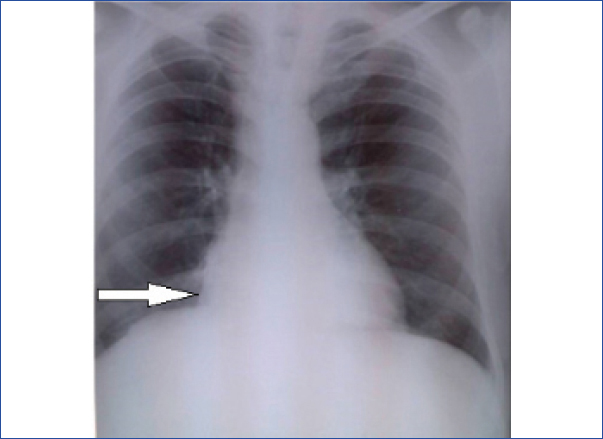
A 60-year-old male who was being worked up for surgical management of cholelithiasis was advised medical consultation for his respiratory complaints. He was a chronic smoker and had a history of long standing cough with dyspnoea on exertion with periodic exacerbations. There was a definitive change in pattern of cough for the last 3 months and he was expectorating mucopurulent sputum. He however ignored it as a seasonal event, that was not very unusual for him. There was no history of fever, haemoptysis, chest pain or increased shortness of breath from baseline. Routine investigations including haemogram, electrocardiogram, liver function test, renal function test, serum electrolytes, fasting blood sugar, coagulogram and urine complete examination were normal. Sputum was negative for acid fast bacillus. Chest radiograph showed paracardiac opacity in right lower zone [Table/Fig-1]. Computed Tomography (CT) of chest showed collapse consolidation of right lower lobe of lung [Table/Fig-2]. Keeping in view prolonged smoking history, age, change in character of cough as reported by the patient, paracardiac opacity and CT findings, malignancy was suspected and patient was taken up for bronchoscopy and during the procedure a suspected mass was seen in the right main bronchus [Table/Fig-3], it was cauliflower like, whitish yellow in colour causing almost complete occlusion of the right main bronchus. Multiple endobronchial biopsies were taken using an alligator jaws type biopsy forceps. As the third biopsy was being taken the mass came up along with the biopsy forceps. At this point it was realised that probably it was a foreign body. An attempt was made to take it out by pulling out the bronchoscope along with the foreign body attached to the biopsy forceps. But during the process, the patient coughed violently and got very restless. As the bronchoscope was taken out, it was observed that the foreign body had got dislodged. The patient suddenly became dyspnoeic and his oxygen saturation began to fall to around 70%. He was given high flow oxygen by a mask and bronchoscope was reintroduced once saturation improved to around 90%. Now the foreign body was seen lying in the left main bronchus. Patient’s head end was lowered and attempt was made to take out the foreign body with a grasping forceps. After a few failed attempts, it was possible to hold it with the grasping forceps. However, again as bronchoscope was negotiating the vocal cords, the patient coughed violently and got up pulling out the bronchoscope. It was noticed that the foreign body had got dislodged from the grasping forceps. However this time, the patient stabilised after a few minutes. On repeat bronchoscopy, the foreign body was nowhere to be seen. It was most likely swallowed by the patient. He was advised for endoscopy which he refused as he was not ready for another procedure after such a traumatic experience for what he considered was a minor routine complaint and now that he was feeling a bit comfortable. X-ray and USG abdomen done subsequently were normal and the post procedure period was uneventful. The biopsy report showed that the foreign body was organic matter [Table/Fig-4]. When specifically asked, the patient gave history of periodic excessive consumption of alcohol with episodes of loss of consciousness. May be during one such event he had unknowingly aspirated the foreign body and was therefore not aware of it. On follow up, his symptoms improved and serial chest radiographs revealed clearance of the right paracardiac opacity [Table/Fig-5].
Right paracardiac opacity in lower zone with slight elevation of diaphragm.
Contrast enhanced CT-scan of chest showed collapse with consolidation in right lower lobe.
Growth seen in right main bronchus during bronchoscopy.
Histopathological section shows vegetable matter admixed with bacterial colonies (H&E 100).
Serial chest radiograph showing clearance of right paracardiac opacity after 4 weeks.
Discussion
Foreign body aspiration is a serious medical condition which demands timely recognition and prompt action [1]. In rare cases it can be present with chronic symptoms like cough, repeated infection or non resolving pneumonia without any obvious history suggestive of an acute event. Foreign body aspiration is common in children and it is not frequently seen in adults [2]. About 75-85% cases occur in children younger than 15 years, more commonly seen in less than three years age group [3].
Rigid bronchoscopy is the preferred mode of its removal in children, but in adults both rigid and flexible bronchoscopies are frequently used [4,5]. Size and shape of foreign body as well as the age of patient determine the site of obstruction. Foreign bodies can either be organic (peanuts, peas) or inorganic (plastic caps, pins, nails, teeth). Risk factors of foreign body aspiration in adults include advanced age, altered state of consciousness due to alcohol or drugs, poor dentition and neurological disorders [6] and it can occur without any underlying risk factors [7]. In adults, they tend to lodge more on right side [8]. Foreign bodies which are proximally lodged mainly have acute presentation like sudden onset cough, choking, hoarseness and aphonia. Bronchial foreign bodies may rarely present with chronic symptoms like cough, repeated infection, non-resolving pneumonia, bronchiectasis, haemoptysis, lung abscess, fibrosis, obstructive emphysema and middle lobe syndrome [9,10]. Organic foreign bodies cause more severe mucosal inflammation, granulation tissue formation leading to complete obstruction and complexity in removal [11]. Identification of foreign body aspiration requires a high index of clinical suspicion, especially in those presenting without a history of aspiration. Chest radiograph has poor sensitivity in diagnosis as most foreign bodies in adults are not radio-opaque however, it can show secondary findings like repeated pneumonia, compensatory emphysema, atelectasis, and bronchiectasis [12]. On CT, manifestations of foreign body aspiration include either direct visualization of radio-opaque foreign bodies or indirect signs like non-resolving pneumonia, atelectasis, unilateral hyperinflation or localized bronchiectasis [13].
Bronchoscopy is frequently both diagnostic and therapeutic in such cases [14].
In our case, first attempt to take out the foreign body failed as biopsy forceps (and not grasping forceps) was tried to pull it out and also the position of the patient was such that the neck was extended. So when the foreign body got dislodged, it gravitated towards the carina. Also, because it was the left lung that was mainly being aerated ever since the foreign body was causing obstruction on right side, it entered the left main bronchus almost asphyxiating the patient. During the second attempt probably a more vigorous anaesthesia of the vocal cords or keeping the patient sedated might have allowed an easier and uneventful exit.
Conclusion
Foreign body aspiration can occur in adults with no underlying risk factors. Patient may be asymptomatic, or have non-specific and long duration of symptoms. Because of the predisposition in elderly age groups, sometimes they may mimic malignancy. So, foreign body aspiration should always be suspected as the aetiology if a patient is having chronic respiratory symptoms not explained by other possible causes.
[1]. Tokar B, Ozkan R, Ilhan H, Tracheobronchial foreign bodies in children:Importance of accurate history and plain chest radiography in delayed presentationClin Radiol 2004 59:609-15. [Google Scholar]
[2]. Rafanan AL, Mehta AC, Adult airway foreign body removal. What's new?Clin Chest Med 2001 22:319-30. [Google Scholar]
[3]. Baharloo F, Veyckemans F, Francis C, Tracheobronchial foreign bodies:Presentation and management in children and adultsChest 1999 115:1357-62. [Google Scholar]
[4]. Ayed AK, Jafar AM, Owayed A, Foreign body aspiration in children:diagnosis and treatmentPediatr Surg Int 2003 19:485-88. [Google Scholar]
[5]. Yadav SP, Singh J, Aggarwal N, Goel A, Airway foreign bodies in children:experience of 132 casesSingapore Med J 2007 48:850-53. [Google Scholar]
[6]. Singh A, Kaur M, Recurrent pneumonitis due to tracheobronchial foreign body in an adultJIACM 2007 8:242-44. [Google Scholar]
[7]. Zubairi AB, Haque AS, Husain SJ, Khan JA, Foreign body aspiration in adultsSingapore Med J 2006 47:415-18. [Google Scholar]
[8]. Asif M, Shah SA, Khan F, Ghani R, Foreign body inhalation-site of impaction and efficacy of rigid bronchoscopyJ Ayub Med Coll Abbottabad 2007 19:46-48. [Google Scholar]
[9]. Franquet T, Gimenez A, Roson N, Torrubia S, Sabate JM, Perez C, Aspiration diseases:fiindings, pitfalls and differential diagnosisRadiographics 2000 20:673-85. [Google Scholar]
[10]. Yilmaz A, Akkaya E, Damadoglu E, Gungor S, Occult bronchial foreign body aspiration in adults:analysis of four casesRespirology 2004 9:561-63. [Google Scholar]
[11]. Oke V, Vadde R, Munigikar P, Bhattarai B, Agu C, Basunia R, Use of flexible bronchoscopy in an adult for removal of an aspirated foreign body at a community hospitalJ Community Hosp Intern Med Perspect 2015 5:28589 [Google Scholar]
[12]. Tseng HJ, Hanna TN, Shuaib W, Aized M, Khosa F, Linnau KF, Imaging foreign bodies:ingested, aspirated, and insertedAnn Emerg Med 2015 66:570-82. [Google Scholar]
[13]. Zissin R, Shapiro-Feinberg M, Rozenman J, Apter S, Smorjik J, Hertz M, CT findings of the chest in adults with aspirated foreign bodiesEur Radiol 2001 11:606-11. [Google Scholar]
[14]. Moura Sa J, Oliveira A, Caiado A, Tracheobronchial foreign bodies in adults - experience of the Bronchology Unit of Centro Hospitalar de Vila Nova de GaiaRev Port Pneumol 2006 12:31-43. [Google Scholar]