Delayed Tension Pneumothorax – Identification and Treatment in Traumatic Bronchial Injury: An Interesting Presentation
Amit Gupta1, Amulya Rattan2, Sunil Kumar3, Vinita Rathi4
1 Additional Professor, Department of General Surgery, All India Institute of Medical Sciences, Rishikesh, Uttarakhand, India.
2 2nd Year MCh Resident, Trauma Centre, All India Institute of Medical Sciences, Delhi, India.
3 Director Professor, Department of General Surgery, University College of Medical Sciences and Guru Teg Bahadur Hospital, Delhi, India.
4 Professor, Department of Radiology, University College of Medical Sciences and Guru Teg Bahadur Hospital, Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Amit Gupta, Additional Professor, Department of General Surgery, All India Institute of Medical Sciences, Rishikesh-249203, Uttarakhand, India.
E-mail: dramit2411@yahoo.co.in
A 13-year-old girl, who did not receive any treatment for few hours following Road Traffic Injury (RTI), reported to the Casualty Department and found to have patent airway with clinically normal C spine, air-hunger (RR 42/minute), trachea deviated to left, distended neck veins and absent breath sounds on the right side. The chest X-ray she carried, done immediately after the injury, showed right sided tension pneumothorax. She was put on oxygen at 11 L/minute and an Intercostal chest tube drainage (ICD) was inserted on right side. Her oxygen saturation (40%) failed to improve. ICD bag showed continuous bubbling and air entry remained absent on the right side. An urgent right thoracotomy was done which revealed right main bronchus tear; the tear was repaired using interrupted Prolene® sutures. Patient recovered well and was discharged 10 days later in a stable condition.
Dyspnoea, Road traffic injury, Thoracotomy
Case Report
A 13-year-old girl met with road traffic injury. Immediately following injury, she was taken to a private hospital, where chest X-ray was done following which the patient was referred to our hospital. In our hospital too, she was first seen by casualty medical officer and referred for Neurosurgery consultation without rendering any treatment in view of the brief history of loss of consciousness. The neurosurgeon found Glasgow Coma Scale (GCS) to be 15/15 and obtained a Non-Contrast Computed Tomography (NCCT) of head, which was normal except for scalp haematoma. Thereafter, she was referred to orthopaedic department in view of pain in left knee. The orthopaedician examined her and found musculoskeletal system to be normal and referred her to the general surgeon in view of dyspnoea. By that time, few hours had elapsed without proper primary survey and treatment. At presentation to surgery emergency, she was evaluated by Advanced Trauma Life Support (ATLS) protocol. Airway with cervical spine was normal. Evaluation of ‘Breathing’ revealed respiratory rate of 42/minute, distended neck veins, trachea deviated to left, absent air entry with hyper-resonance on the right side. Oxygen saturation was 40%. Chest X-ray, done immediately after the trauma in a private hospital, showed right sided pneumothorax [Table/Fig-1]. Her pulse rate was 90/minute, blood pressure was 104/66 mmHg and GCS was 15. Both pupils were normally reacting to light. A diagnosis of right sided tension pneumothorax was made and immediate tube thoracostomy was done on right side following which air came out freely and collected in bag with lot of bubbling. Left sided ICD was also done as air entry was felt to be decreased on that side too; this revealed only minimal haemothorax. However, the SpO2 did not significantly improve. In view of above findings, she was suspected to have right bronchial injury and urgent right thoracotomy was planned.
Chest X-ray showing right sided pneumothorax.

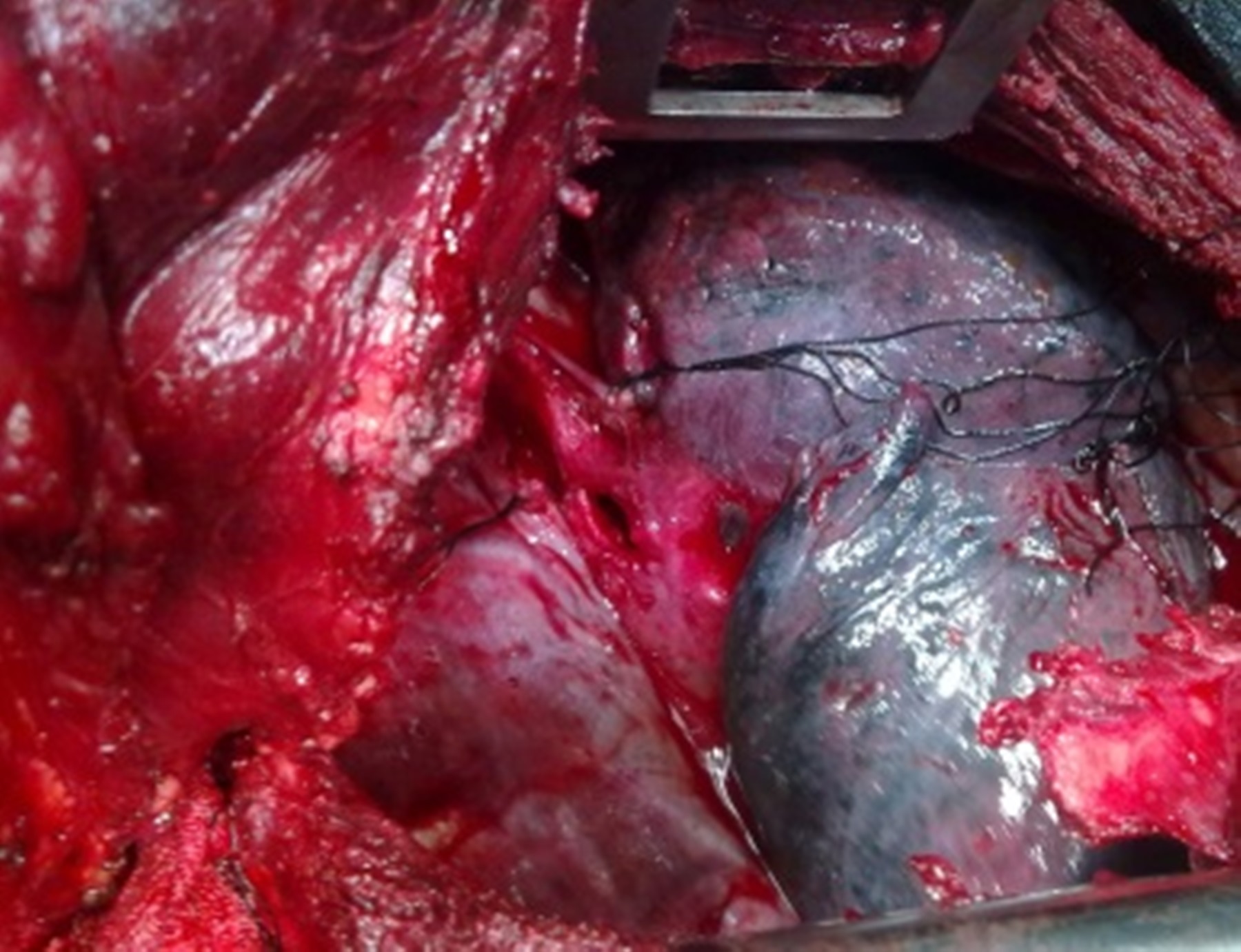
Right thoracotomy was done under general anaesthesia using standard endotracheal tube. Patient was found to have right main bronchus injury [Table/Fig-2] and no associated lung laceration or rib fractures. The right main stem bronchus was primarily repaired using polypropylene 2/0 interrupted sutures. Her oxygen saturation markedly improved. After surgery, patient was kept on ventilator support for one day, and on second postoperative day ventilator support was removed. Patient was shifted to ward on third postoperative day, both chest tubes were removed on fourth postoperative day and made an uneventful recovery. She was discharged on eighth postoperative day and is doing well in follow up period.
Intraoperative photograph showing right main stem bronchial injury.
Discussion
Bronchial injury is a life-threatening condition with non-specific presentation; hence, it goes unnoticed frequently during the initial assessment of traumas patients. The incidence of airway injury is about 1%–3% of all blunt chest injuries. Bronchial injury occurs in 1.5% of major chest trauma of which 30% are missed. Left sided bronchial injuries are more common and most of the injuries occur within 2.5 cm of carina [1].
The possible mechanisms for bronchial injury include: (a) rapid deceleration with resultant shearing of mobile lung and bronchi relative to fixed proximal structures; (b) forced expiration against a closed glottis, causing a sudden rise in airway pressure and resultant longitudinal tear in the bronchi; and (c) compression between the sternum and vertebral column, leading to bursting injury [2]. The signs and symptoms are non-specific which include subcutaneous emphysema, dyspnoea, desaturation, pneumothorax and tension pneumothorax.
About 10% of the patients with bronchial injury are asymptomatic.
The radiographic manifestations too are usually non-specific and include pneumomediastinum, pneumothorax, pneumoretroperitoneum, deep cervical emphysema and subcutaneous emphysema. However, the “fallen lung sign” is specific for complete bronchial transaction [3].
Computed Tomography (CT) of the chest is the imaging modality of choice; it not only confirms the diagnosis but also aids in understanding the extent of damage to other structures. However, fibreoptic bronchoscopy is the best diagnostic tool for determining the location and extent of airway injuries. Because of the nature of multiple injuries, a flexible bronchoscope through an endotracheal tube is usually used. Pate JW recommended rigid bronchoscopy [4]. If these studies are negative and strong suspicious still exists, bronchography may be done. The usage of ventilator, primarily positive end expiratory pressure or continuous positive airway pressure may be disastrous in a patient with suspected bronchial injury [5]. Well functioning thoracostomy tubes should be placed before the patient is positioned on the ventilator. The management of these patients is challenging and depends upon location of the injury, degree of major airway destruction as well as the degree of distal pulmonary parenchymal destruction. It is a challenging diagnosis for the emergency physician and needs a high index of suspicion.
In case of bronchial tear of more than one third circumference, surgical exploration and repair is required or it would lead to stenosis, repeated chest infection and collapse of the lung. Indications of surgery include tension pneumothorax, tracheobronchopleural fistula after drainage, increasing pneumomediastinum or surgical emphysema (despite conservative measures), transmural tear >2 cm and prolapse of oesophageal wall into trachea or mediastinitis. Triple assessment by clinical, radiological and bronchoscopic findings should be done before surgical consideration. Severe cases require pneumonectomy [6,7]. The prognosis after surgery depends on other associated injuries and previous condition of the patient.
Conclusion
This case is unusual in terms of isolated right bronchial injury, without associated injuries and delayed recognition despite clinically and radiologically evident tension pneumothorax. The patient was lucky to have survived despite all odds.
[1]. Hippargi SH, Traumatic bronchial rupture: an unusual cause of tension pneumothoraxInt J Emerg Med 2010 3:193-95. [Google Scholar]
[2]. Bowling WM, Wilson RF, Kelen GD, Buchman TG, Thoracic trauma. In: Tintinalli JE, Kelen GD, Stapczynski S, Ma OJ, Cline DM (eds)Tintinalli’s emergency medicine: a comprehensive study guide 2003 6th ednNew YorkMcGraw-Hill Companies, Inc.:1675 [Google Scholar]
[3]. Grover FL, Ellestad C, Arom KV, Root HD, Cruz AB, Trinkle JK, Diagnosis and management of major tracheobronchial injuriesAnn Thorac Surg 1979 28(4):384-91. [Google Scholar]
[4]. Pate JW, Tracheobronchial and oesophageal injuriesSurg Clin North Am 1989 69(1):111-23. [Google Scholar]
[5]. Davari HR, Malekhossini SA, Management of tracheobronchial injury: Case presentation and review of the literatureActa Medica Iranica 2005 43(4):291-98. [Google Scholar]
[6]. Menon RG, Maddali MM, Valliathu J, Bulushi AAW, Delayed diagnosis of bronchial transaction following blunt chest traumaInd J Thorac Cardiovasc Surg 2008 24(1):15-17. [Google Scholar]
[7]. Dewan RK, Ramchandani R, Sisodia A, Verma PK, Delayed presentation of traumatic bronchial tear and successful repairIndian J Thorac Cardiovasc Surg 2012 28(2):143-45. [Google Scholar]