Anorectal Melanoma: An Unusual Cause of Rectal Bleeding
Uma Kumar1, Udita Singhal2
1 Specialist Pathology, Department of Pathology, ESI Hospital, Delhi, India.
2 Assistant Professor, Department of Pathology, ESI Hospital and Dental College, Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Uma Kumar, Specialist Pathology, Department of Pathology, ESI Hospital, Sector 15, Rohini, Delhi-110089, India.
E-mail: dr.uma.path@gmail.com
Anorectum is a rare site for primary melanoma. It is an aggressive cancer with poor prognosis. The diagnosis is often delayed due to non-specific signs and symptoms. Clinically, it is often misdiagnosed as hemorrhoids. The cytological diagnosis can be challenging especially when melanin pigment is sparse or absent. Herein, we present a rare case of anorectal melanoma which was initially misdiagnosed as hemorrhoids. A final correct diagnosis was made on cytology when later on the patient developed inguinal metastasis.
Cytology, Lymph node metastasis, Malignant, Rectum
Case Report
A 55-year-old male came to surgical clinic with complaints of bleeding per rectum and a protruding mass during defecation for six months. He was taking treatment in the form of sitz bath and stool softener from a local practitioner for hemorrhoids. There was no significant medical history. On physical examination, patient was conscious, oriented and thin built, pale, pulse-78/min, BP- 126/82 mmHg and was afebrile. There was no icterus, cyanosis or pedal edema. Left inguinal lymph nodes were palpable measuring 1.5 to 0.5 cm. Local examination revealed an irregular, friable mass measuring 2.5 x 2 cm protruding from the anal canal on the left side of anal verge. Per rectal digital examination revealed a firm to hard exophytic growth in continuity with the external mass. Blood investigation revealed microcytic hypochromic anaemia with haemoglobin 9 gm/dl, total leucocyte count 15660/cm3, platelet count 5.6 lakhs/cm3. Blood carcinoembryonic antigen level was 3.7 ng/ml (0-2.5 ng/ml). Liver function tests and renal function tests were within normal limits. Contrast enhanced computed tomography showed long segment circumferential thickening of rectum with loss of fat plane between anterior and posterior bladder wall with perirectal lymphadenopathy. A provisional diagnosis of a malignant lesion with lymph node metastasis was rendered and Fine Needle Aspiration Cytology (FNAC) from anal swelling and inguinal lymph node was advised.
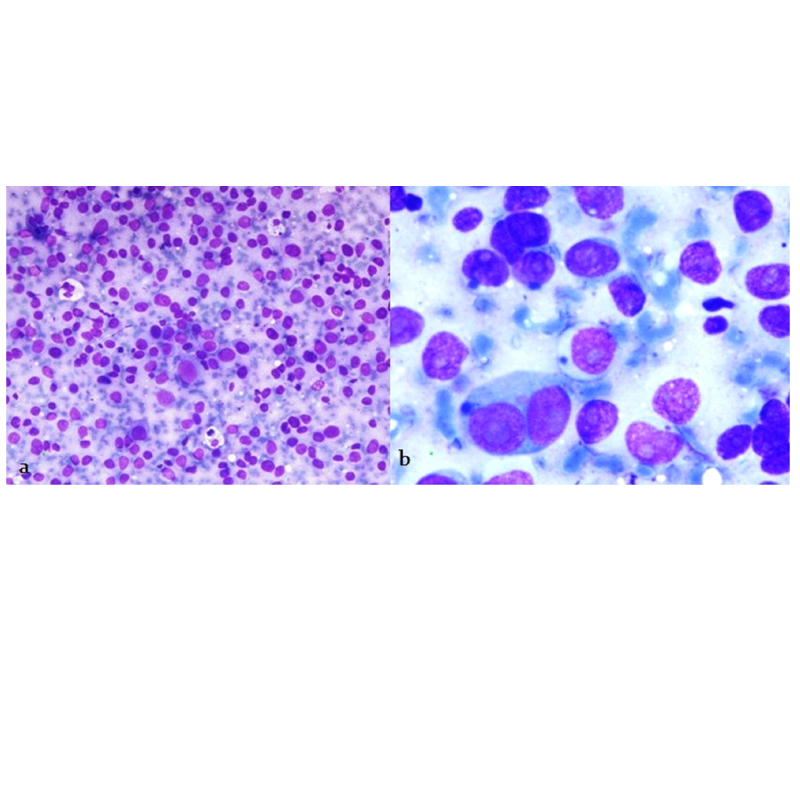
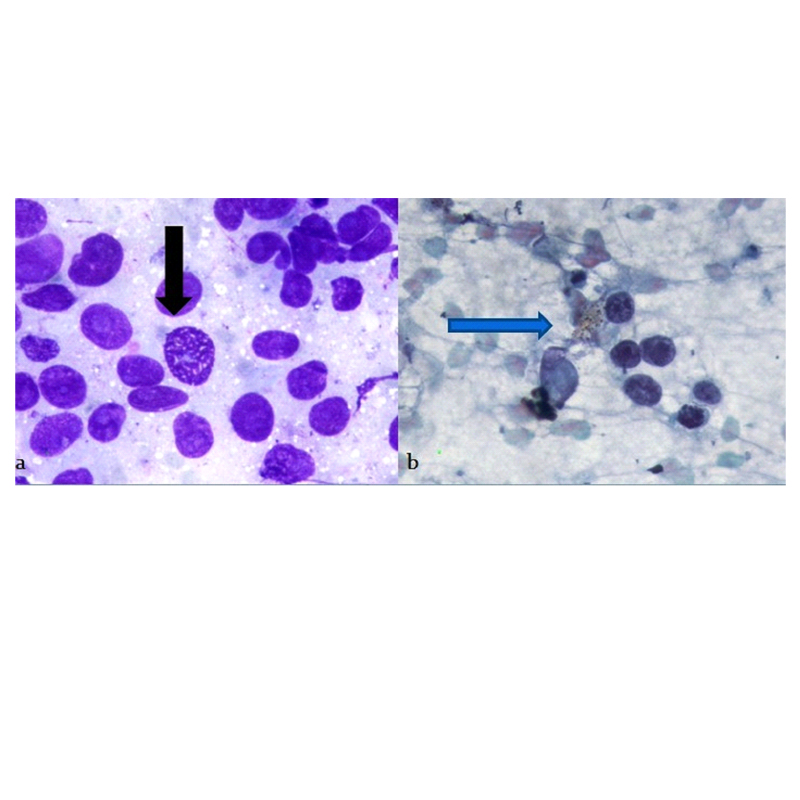
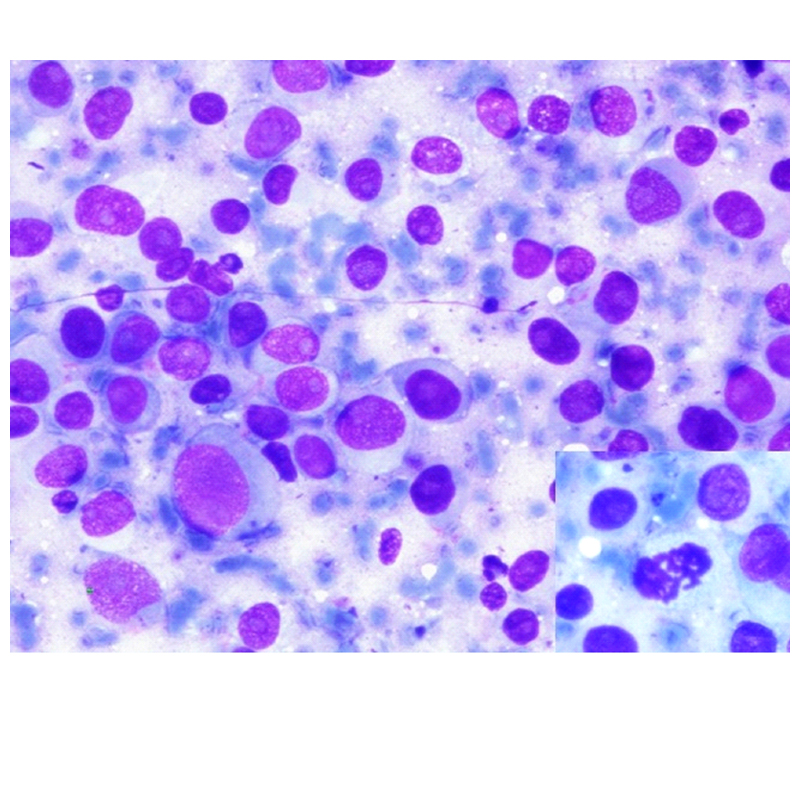
FNAC was done from anal swelling and inguinal lymph node. The smears were stained with Giemsa and Papanicolaou stains. Smears from anal swelling revealed high cellularity with singly dispersed cell population [Table/Fig-1a]. These cells were highly pleomorphic, with increased N:C ratio, had centrally placed nuclei, prominent single nucleoli and moderate amount of cytoplasm [Table/Fig-1b]. Numerous mitotic figures were also seen [Table/Fig-2a]. Many binucleate cells, bizarre cell were also noted [Table/Fig-1b]. Few of the cells showed intracytoplasmic brown to black pigment [Table/Fig-2b]. Smears from inguinal lymph node showed a similar morphology, however, intracellular pigment was not seen in these smears [Table/Fig-3]. So, a diagnosis of malignant melanoma of anal canal with lymph node metastasis was rendered on cytology and biopsy was advised for histopathological confirmation.
Cytological smear showing a) Highly cellular smear with singly dispersed cells (Giemsa stain 100x); b) Cells with centrally placed nuclei with prominent nucleoli. Binucleate cell also seen (Giemsa stain 400x).
a) Cells showing marked pleomorphism and mitosis (black arrow marked) (Giemsa stain 400x); b) Cells showing intracytoplasmic pigment (blue arrow marked).
Cytology smears from lymph node showing singly scattered cells with eccentrically placed nuclei and prominent nucleoli, inset showing mitosis (Giemsa stain 400x).
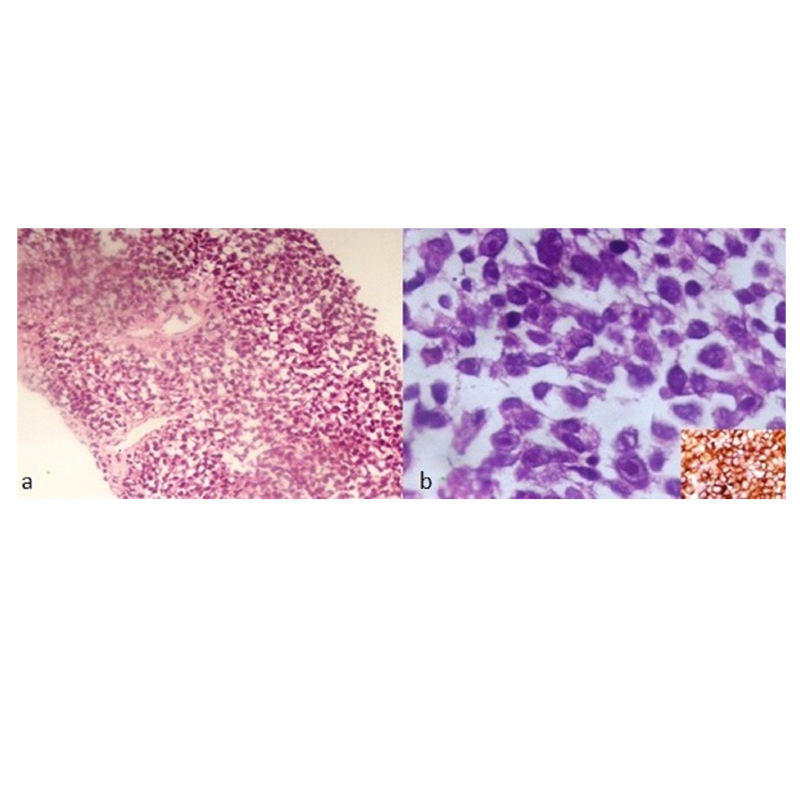
A punch biopsy from rectum was done under local anaesthesia. Hematoxylin and Eosin (H&E) stained sections showed a tumour composed of round to polygonal cells, indistinct cytoplasm and high N:C ratio. Nuclei showed moderate pleomorphism, were hyperchromatic with prominent eosinophilic large nucleoli and anisonucleolosis [Table/Fig-4a]. The tumour cells were positive for HMB-45 [Table/Fig-4b]. So, final diagnosis of anorectal melanoma was given. A staging positron emission tomography was performed which showed multiple metastasis in liver, spleen, inguinal lymph nodes and abdomino-pelvic lymph nodes. Patient was referred to a higher centre for further management. Unfortunately, the patient was lost to follow-up.
a) Section showing tumour cells arranged in sheets (H&E 100x); b) High power showing cells with high nuclear cytoplasmic ratio and prominent nucleoli, inset showing tumour cells positive for HMB-45 (H&E 400x).
Discussion
Anorectal melanoma is an extremely rare and highly aggressive malignancy which has a tendency to early distant spread [1]. It represents less than 1% of all melanomas and accounts for around 0.25%-1.25% of all anorectal malignancies [2]. More than 90% melanomas are cutaneous in origin. Of the remaining forms of melanoma ocular melanoma accounts for approximately 5%, melanoma of unknown origin for 2% and mucosal melanoma for 3%. Within the mucosal subgroup, anorectal melanoma is the third most common site after head/neck and the female genital system [3].
The mean age of disease onset is 60 years. Some studies suggested female predominance [1]. The lesion is usually polypoidal and easy to bleed, with or without pigmentation. The most common presentation is rectal bleeding, pain, tenesmus and changes in bowel habit [1,2]. Because of the nonspecific symptoms it is easily mistaken for hemorrhoids, similar to our case. The tumour is located usually in or close to pectinate line and grow towards rectal ampulla. It extends along the submucosal plane proximally towards rectum, simulating a primary rectal tumour [2,3]. Wienstock MA reported that 41% of anorectal melanoma had regional spread, 22% had distant metastasis and only 37% had confined disease [4]. Sites of distant metastasis are lymph nodes, lungs, liver brain, bone and skin [1,3]. Our patient had liver, spleen, inguinal lymphnodes and abdominopelvic lymph nodes metastasis at the time of presentation. The average survival is of 8-24 months with a five year survival rate of 10%-15% [5]. Prognostic factors include the stage of the disease at the time of diagnosis and the tumor thickness [3,4].
Anorectal melanoma arises from the melanocytes present in the mucosa of anal canal. Studies suggest that there is a role of activating KIT (KIT proto-oncogene receptor tyrosine kinase) mutation in the pathogenesis of anorectal melanoma [6].
Cytological features of the malignat melanoma include: highly cellular smear with epithelioid/plasmacytoid cells with abundant cytoplasm, cytoplasmic melanin pigment, macronucleoli, prominent anisokaryosis, pseudoinclusions and frequent binucleated and multinucleated cells. The presence of intracellular melanin in neoplastic cells is the gold standard for the diagnosis of malignant melanoma [7]. Murali R et al., studied cytomorphological features of metastatic malignant melanoma in 944 cases and found melanin pigment in only 262 (27.6%) cases [8]. In our case, smears from anal swelling showed intracellular melanin in occasional cell. Special stains like masson fontana, melanin bleach can be used to confirm the pigment, but it was not done in our case. Cytological differential diagnosis are poorly differentiated adenocarcinoma and lymphoma [7,8].
On histopathology, the diagnostic clue for malignant melanoma are cytoplasmic brown to black coloured pigment and junctional changes. The junctional changes implies the presence of atypical epidermoid cells adjacent to the focus of malignant tumor. In the absence of these two, diagnosis of melanoma depends on the immunohistochemistry. Melanoma cells are positive for S-100, HMB-45, vimentin, melan A, tyrosinase and MITF [9,10]. Several new diagnostic markers are under investigation like MUM-1, Mel-5, melanocortin-1 and PNL2 [10]. Unfortunately, the treatment of anorectal melanoma is moderately successful. Surgery remains the mainstay of treatment which includes wide local excision and abdomino-perineal resection. Lymph node dissection is advised for clinically palpable lymph nodes. Chemotherapy, radiation therapy and immune therapy have limited role [11].
Conclusion
To conclude, anorectal melanoma is an extremely rare, highly aggressive malignancy. Survival can be improved by early detection and complete surgical removal. A high clinical index of suspicion should be kept for an elderly patient with complaints of rectal bleeding. FNAC is an easy and cost effective tool to aid the diagnosis and for optimal clinical management.
[1]. Podnos YD, Tsai NC, Smith D, Ellenhorn JD, Factors affecting survival in patients with anal melanomaAm Surg 2006 72:917-20. [Google Scholar]
[2]. Khan M, Bucher N, Elhassan A, Barbaryan A, Ali AM, Hussain N, Primary anorectal melanomaCase Rep Oncol 2014 7:164-70. [Google Scholar]
[3]. David Row, Martin R. Weiser, Anorectal MelanomaClinics in Colon and Rectal Surgery 2009 22(2):120-26. [Google Scholar]
[4]. Weinstock MA, Epidemiology and prognosis of anorectal melanomaGastroenterology 1993 104(1):174-78. [Google Scholar]
[5]. Urbani M, Troian M, Bellio G, Bortul M, Primary anorectal melanoma: a case of 5 year disease-free survivalInternational Surgery Journal 2017 4(2):768-71. [Google Scholar]
[6]. Antonesco CR, Busam KJ, Francone TD, Wong GC, Guo T, Agaram NP, L576KIT mutation in anal melanomas in anal melanomas correlates with KIT protein expression and is sensitive to specific kinase inhibitionInt J Cancer 2007 121(2):257-64. [Google Scholar]
[7]. Chakrabarti PR, Varma A, Kiyawat P, Gupta K, Cytological diagnosis of metastatic melanoma: A case report (Metastatic melanoma diagnosed on FNAC)Indian Journal of Pathology and Oncology 2015 2(2):84-86. [Google Scholar]
[8]. Murali R, Watson GF, Lee CS, Uren RF, Saw RPM, Scolyer RA, Diagnosis of metastatic melanoma by fine-needle biopsy: Analysis of 2204 casesAm J Clin Pathol 2007 127:385-97. [Google Scholar]
[9]. Chute DJ, Cousar JB, Mills SE, Anorectal malignant melanoma: morphologic and immunohistochemical featuresAm J Clin Pathol 2006 126(1):93-100. [Google Scholar]
[10]. Weinstein D, Leininger J, Hamby C, Safai Bijan, Dignostic and prognostic biomarkers in melanomaJ Clin Aesthet Dermatol 2014 7(6):13-24. [Google Scholar]
[11]. Marc Singer, Matthew G, Mutch. Anal melanomaClinics in colon and Rectal Surgery 2006 19(2):78-87. [Google Scholar]