Psoriasis is a chronic non-communicable skin disorder occurring at all ages, although it is most common between the ages of 50 and 69. It is a painful disfiguring disease adversely affecting the quality of life [1]. The prevalence varies from 0.09% to 11.4% depending on the country/region being studied [2,3]. It is characterised by long clinical course punctuated by remissions and relapses. It may be associated with a variety of comorbidities [4]. The cause of this disease is still not fully established. Genetic and immunological mechanisms are presumed to play significant role in its pathogenesis. Although, there are suggestions that it could be an autoimmune disease, no autoantigen has so far been identified [5]. There is strong evidence that T cell mediated immunological reactions occur in psoriasis [6]. Platelet activation also plays an important role in such immunological inflammatory reactions. One of the platelet parameters that act as an indicator of platelet activation is MPV. Relationship between MPV and psoriasis has been the subject of investigation in several recent studies [7-10]. The results so far have been inconclusive and conflicting. Some of these studies have claimed statistically significant increase in mean MPV values in psoriasis patients and a strong correlation between MPV and PASI [7,8]. Investigators of these studies have proposed MPV as a viable marker for the severity of psoriasis. However, a few other investigators were not able to reproduce association between MPV and psoriasis [11,12]. The present study was taken up with an aim to determine the relationship between all the ten haematological parameters and the disease severity index in psoriasis patients.
Materials and Methods
The present case control study was carried out at Chettinad Hospital and Research Institute, a tertiary care hospital located on the suburbs of Chennai, India. The duration of the study was 4 months from May to September 2016. Sample size was calculated using the formula for a quantitative Case-Control study using Odds Ratio value and expected proportion exposed in controls of previous studies [7-10]. The calculated sample size was 150, due to time constraint (4 months) it was reduced to 100. Fifty adult patients of psoriasis including 38 males and 12 females were enrolled as cases and 50 healthy age matched adult subjects (43 males and 7 females) used as controls. Only patients with established diagnosis of psoriasis on the basis of clinical and histopathogical criteria were included in the study. All those with history of metabolic syndromes, cardiovascular disease, inflammatory bowel disease, haematological disorders, kidney or liver disease and any other disease that could alter the haematological parameters were excluded from the study. Physiologically healthy individuals who are willing to participate in the study were included as controls. Relevant clinical information was obtained from all the patients.
PASI [13] was calculated by using the formula:
where
E–Erythema, I–Indurations, D-Desquamation, A-Area of skin affected, H–Head, U- Upper limb, T–Trunk, L–Lower limb.
The severity of erythema, induration and desquamation of the psoriasis is assessed as none (0), mild (1), moderate (2), severe (3) or very severe (4). The area of affected skin is expressed as nil (0), 1-9% (1), 10-29% (2), 30-49% (3), 50-69% (4), 70-89% (5) or 90-100% (6). Once the score is derived the Psoriasis is usually classified as mild when PASI score of ≤10, moderate to severe when PASI score is >10.
Venous blood was collected in K2EDTA vacutainer from all the patients and control subjects to determine the following parameters using Coulter LH780 Haematology analyser: Red Blood Cell Count (RBC), White Blood Cell Count (WBC), Haemoglobin (Hb), haematocrit (HCT), Mean Corpuscular Volume (MCV), Mean Corpuscular Haemoglobin (MCH), Mean Corpuscular Haemoglobin Concentration (MCHC), Red Cell Distribution Width (RDW), Platelet Count (PLT) and Mean Platelet Volume (MPV).
The results were statistically analysed using IBM SPSS software (Version 21) or Graph pad Prism (version 7). Student’s t-test for independent samples was used to compare the data obtained from the patients and the control subjects. Spearman Rank Correlation was used to find the correlation between PASI and haematological parameters. A p-value of 0.05 or less was considered significant and a value of <0.01 was deemed highly significant.
Results
The mean, Standard Deviation (SD) and the p-values of haematological parameters in the control subjects and the patients (PASI measured for patients alone) are given in the [Table/Fig-1].
Mean, SD and p-value of haematological parameters in psoriatic patients and healthy controls (including males and females). Note: NS=not significant; S=significant; SD values are below mean values and are preceded by ±sign; the number of cases in controls and patient group are given in parenthesis in top row in that order.
| MPV | All Cases (50 & 50) | Males (43 & 38) | Females (7 & 12) |
|---|
| Control | Patient | p-value | Control | Patient | p-value | Control | Patient | p-value |
|---|
| Age | 50.62 ±14.78 | 46.10 ±11.99 | 0.096 NS | 50.63 ±14.96 | 46.82 ±12.26 | 0.217 NS | 50.57 ±14.79 | 43.83 ±10.78 | 0.277 NS |
| WBC | 8.11 ±2.40 | 8.35 ±2.30 | 0.611 NS | 7.87 ±2.51 | 8.42 ±2.43 | 0.413 NS | 8.99 ±1.44 | 8.13 ±1.83 | 0.318 NS |
| RBC | 4.78 ±0.50 | 4.86 ±0.96 | 0.604 NS | 4.77 ±0.51 | 4.95 ±0.82 | 0.253 NS | 4.86 ±0.48 | 4.60 ±1.27 | 0.536 NS |
| HGB | 13.11 ±1.74 | 13.34 ±2.27 | 0.585 NS | 13.12 ±1.83 | 13.50 ±2.04 | 0.372 NS | 13.10 ±1.13 | 12.81 ±2.80 | 0.763 NS |
| HCT | 40.73 ±5.06 | 42.18 ±7.75 | 0.271 NS | 40.66 ±5.28 | 42.89 ±7.27 | 0.124 NS | 41.14 ±3.66 | 39.94 ±8.69 | 0.691 NS |
| MCV | 85.20 ±6.14 | 87.68 ±11.37 | 0.178 NS | 85.29 ±6.55 | 86.84 ±9.55 | 0.402 NS | 84.66 ±2.62 | 90.35 ±15.51 | 0.254 NS |
| MCH | 26.96 ±3.83 | 27.85 ±4.50 | 0.288 NS | 27.43 ±2.50 | 27.50 ±4.11 | 0.920 NS | 24.11 ±8.08 | 28.97 ±5.38 | 0.140 NS |
| MCHC | 32.11 ±0.77 | 31.69 ±1.67 | 0.115 NS | 32.16 ±0.81 | 31.58 ±1.78 | 0.073 NS | 31.83 ±0.31 | 32.06 ±1.21 | 0.558 NS |
| RDW | 13.66 ±1.21 | 15.16 ±3.88 | <0.02 S | 13.70 ±1.26 | 14.88 ±3.41 | <0.05 S | 13.39 ±0.31 | 16.02 ±4.98 | 0.112 NS |
| PLT | 256.44 ±81.02 | 220.40 ±61.90 | <0.02 S | 246.65 ±81.53 | 222.03 ±63.95 | 0.138 NS | 316.57 ±46.49 | 215.25 ±54.79 | <0.01 S |
| MPV | 8.51 ±1.64 | 9.65 ±2.07 | <0.01 S | 8.61 ±1.72 | 9.79 ±2.07 | <0.01 S | 7.90 ±0.82 | 9.20 ±2.00 | 0.0731 NS |
| PASI | | 15.88 ±2.51 | | | 15.84 ±2.50 | | 16.03 ±2.22 | | |
Average age of the control subjects was 50.62 years (SD 14.78 years). There was no noticeable difference in average age between male and female control subjects. Average age of the patients was less than that of the controls but was not significant. When all the subjects of study were considered, three parameters, namely, RDW, PLT and MPV showed significant differences in mean values between the control subjects and the patients. The mean values for RDW and MPV were significantly elevated in patients. When adjusted p-value was determined, only MPV remained statistically significant (0.032).
When gender-based analysis for these three parameters was done, the following differences were observed. While mean values for RDW and MPV were higher in patients of both sexes, only in males, the increase was statistically significant (RDW<0.05; MPV <0.01). It was the other way around with PLT. Though, it was lower in patients of both sexes when compared with the control subjects, it was significant only in female patients (p <0.01).
All the patients had a PASI score of > 10 (moderate to severe psoriasis) and the average was 15.88 (SD 2.51). There was no significant difference in the severity of disease between male and female patients (p 0.87). [Table/Fig-2] summarises correlation between PASI and various haematological parameters.
Spearman Rank Correlation between various haematological factors and PASI for all the patients, male patients and female patients. Note: rho= Spearman rank correlation coefficient; p=p-value; ALL= all patients; F=females; M=males. Spearman Rank Correlation test was used
| | WBC | RBC | HGB | HCT | MCV | MCH | MCHC | RDW | PLT | MPV |
|---|
| PASI ALL | rho | -.240 | -.038 | -.078 | -.025 | .040 | .024 | -.030 | .257 | -.509 | .597 |
| p | .093 | .796 | .592 | .864 | .782 | .868 | .838 | .072 | <.001 | <.001 |
| PASI F | rho | -.067 | -.203 | -.280 | -.084 | .266 | .168 | .004 | .502 | -.628* | .621 |
| p | .837 | .527 | .378 | .795 | .404 | .602 | .991 | .096 | .029 | .031 |
| PASI M | rho | -.281 | .066 | -.037 | .004 | -.019 | -.011 | -.057 | .197 | -.467 | .578 |
| p | .088 | .694 | .824 | .981 | .910 | .948 | .734 | .236 | .003 | .000 |
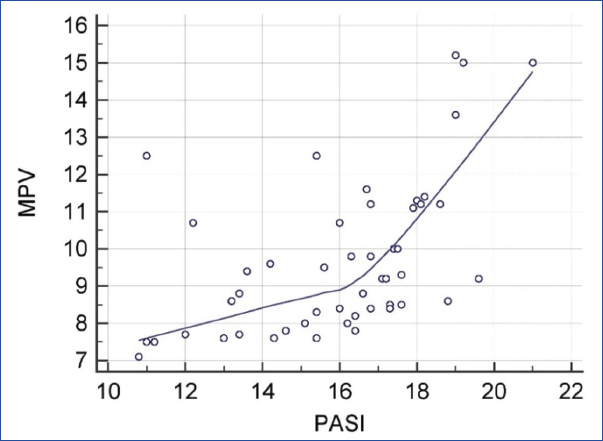
Overall, PASI showed a strong positive correlation with MPV (rho 0.597) which was statistically highly significant (p<0.001) [Table/Fig-3].
Graph showing rank correlation between MPV and PASI (rho 0.597; p <0.01)
By contrast, PASI showed a strong negative correlation with PLT (rho -0.509) which was also statistically highly significant (p<0.01) [Table/Fig-4].
Graph showing inverse rank correlation between PLT and PASI (rho -0.507; p <0.01)
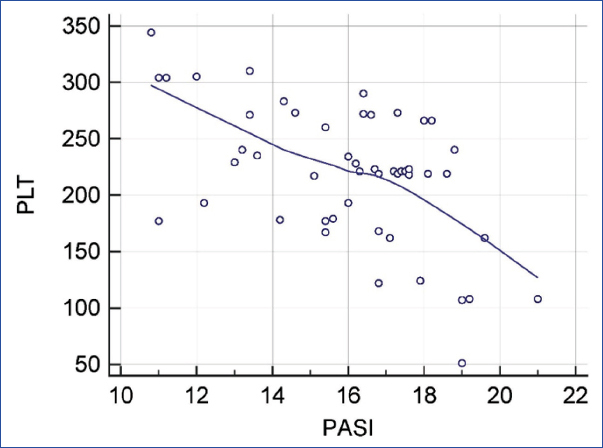
These correlations persisted when gender based analysis was done. In male patients, the correlation coefficients were R=0.578 (p <0.01) for MPV and R=-0.467 (p<0.01) for platelets. In female patients, corresponding values were R=0.621 (p<0.05) for MPV and R=-0.628 (p<0.05) for platelets.
[Table/Fig-5] shows the age and gender wise distribution of Mean PASI score, age of onset and duration of Psoriasis. The commonest age group in which the patients presented with psoriasis was 41 to 50 years. The mean duration of the disease ranged between 3 to 8 years.
Age and Gender wise distribution of Mean PASI score, age of onset and duration of Psoriasis
| Age group | Gender | No of patients | Mean PS Score | Mean Age of Onset (years) | Mean Duration (years) |
|---|
| 21 -30 | Males | 4 | 15.53 | 22.20 | 3.25 |
| Females | 1 | 16.40 | 19.00 | 3.00 |
| 31 -40 | Males | 8 | 15.98 | 30.70 | 5.00 |
| Females | 4 | 17.20 | 34.00 | 4.00 |
| 41-50 | Males | 12 | 15.41 | 40.75 | 5.83 |
| Females | 5 | 15.16 | 39.80 | 5.60 |
| 51-60 | Males | 9 | 15.91 | 49.10 | 6.70 |
| Females | 1 | 15.16 | 39.80 | 5.60 |
| 61-70 | Males | 5 | 15.54 | 58.80 | 7.00 |
| Females | 1 | 15.10 | 50.00 | 8.00 |
Discussion
Psoriasis is a common non-contagious chronic inflammatory disorder characterised by activation of T cells with the release of pro-inflammatory cytokines like tumour necrosis factor alpha (TNFα), interleukin 1, interleukin-6, interleukin-17, interleukin-22 and interleukin-36 [6,14,15]. These mediators are supposed to cause rapid turnover with premature maturation of keratinocytes. However, none of these mediators have proved to be reliable biological markers for the disease or its severity. In an attempt to find a reliable biological marker, some of the recent studies have explored the suitability of platelets and their products for that purpose as platelets are known to play an important role not only in haemostasis but also in inflammation. The platelet related parameters that have been evaluated so far thus, include platelet-lymphocyte ratio (PLR), CD-62, p-selectin, PDW and MPV [10,11,16]. Some of these are indicators of platelet activation. Among these, MPV has attracted the most attention. MPV values seem to be altered in a variety of disorders including systemic lupus erythematosus, cardiovascular disease, systemic sclerosis, rheumatoid arthritis, osteoarthritis etc., [17, 18].
Karabudak O et al., in a study carried out on 20 patients with mild to moderate psoriasis, found significantly higher values for MPV in patients compared to controls [7]. In another study, done on 106 patients of psoriasis and psoriatic arthritis, Canpolat F et al., was able demonstrate a significantly higher MPV in psoriasis as well as psoriatic arthritis [8]. MPV also showed a positive correlation with PASI and duration of the disease. They suggested that MPV could be a useful marker for the severity of the disease. Chandrasekar L et al., in their case control study on 62 psoriasis patients along with age and sex matched controls [10]; found that MPV values were higher in patients as part of overall activation of platelets.
In a retrospective study, Kim DS et al., found that patients with psoriasis had elevated values for MPV that correlated with PASI [9]. In marked contrast to these studies, Saleh HM et al., failed to see any significant association between psoriasis and MPV in their study to find out the role of platelet activation in the causation of psoriasis and atherosclerosis [11]. In their study, CD62 appeared to be more important as a biological marker. The experience of Isik S et al., [12] was similar to Saleh HM et al., [11]. They also failed to find a link between psoriasis and MPV. In another study, Kilic S et al., found significantly elevated MPV in both psoriatic patients and psoriatic arthritis patients. However, the correlation with PASI was only weakly positive [19].
In the present study, haematological parameters of 50 patients with moderate to severe psoriasis were compared with 50 age matched controls. Values for three parameters, namely, RDW, PLT and MPV showed statistically significant differences between the two groups. RDW (p <0.05) and MPV (p<0.01) were significantly increased while PLT was significantly decreased (p<0.05). As far as MPV values are concerned, our findings showed significant higher values which was in agreement with the findings of studies done by Karabudak O et al., p =0.001 [7], Canpolat F et al., p<0.001 [8], Kim DS et al., (r=0.189, p=0.006) [9], Chandrasekar L et al., (p<0.001) [10], Kilic S et al., (p =0.012) [19]. Similarly, elevated RDW levels in psoriasis have been observed in earlier studies [20]. Although, the mean PLT was significantly lower in patients than in controls, only in three patients there was thrombocytopenia; in all others, the values were within normal limits. Lower PLT is probably related to drug therapy [21]. When gender based analysis was done, only in the males, mean RDW and MPV were significantly elevated; although, the mean PLT values were decreased, it was not statistically significant. In women, only mean PLT showed significant reduction. Other two parameters were not significantly altered. This gender based difference on the effect of psoriasis on haematological parameters has not been observed earlier. It may be the result of relatively low number of female patients, which may be one of the limitations of the present study. It can only be clarified by performing the study on a larger number of female patients. However, a recent study claims that psoriasis tends to be more severe in males than in females, thus, giving support to the notion of gender influence on the expression of disease [22].
The positive correlation between PASI and MPV was statistically significant. This is in agreement with the observations of Canpolat F et al., and Kim DS et al., [8,9]. This correlation persisted in both males and females when the gender based analysis was done. There was a strong negative correlation between PLT and PASI, which persisted even when male and female patients were analysed separately. To the best of our knowledge, this inverse correlation between platelet count and severity of the disease has not been documented in literature. Our findings support the contention that increasing MPV and decreasing PLT are indicators of severe disease.
Limitation
The study was conducted for a short period of time and the number of female patients was less. This can be rectified by extending the study duration and sample size. In the future certain other platelet related parameters (PLR, PDW) can be analysed to correlate the platelet activation on PASI score.
Conclusion
From the present case control study involving 50 patients with moderate to severe psoriasis and 50 age matched controls, the mean values for MPV and RDW were higher and mean platelet values were lower in patients than controls. These differences between the patients and controls were statistically significant; but gender based analysis affected results. The changes in MPV and RDW were significant only in males and the changes in Platelet counts were significant only in females. MPV values and Platelet counts showed strong positive and negative correlation respectively, with the PASI score, which was also observed in both male and female patients independently. It can be concluded that increasing MPV and decreasing platelet count can be used as good indicators of the severity of psoriasis. These indicators could also help in assessing the treatment course of the disease.