Presently, India is with rising epidemic of diabetes, a lifestyle and stress-related disorder, occupying 19% of world’s diabetic population and second place in reference to prediabetes, an asymptomatic condition occurring even before, the onset of clinically established diabetes and worldwide estimation of diabetes prevalence of 381.8 million adults in 2013 that is projected to 591.9 million adults in 2035 [1–4]. Diabetes mostly affects the elder population in developed countries; but in developing countries like India, young adults are affected causing threat to their quality of living, working lifestyle and health [2]. They often feel challenged by the disease condition, its substantial demands. and day-to-day management. In these modern days, most common causes to develop diabetes and prediabetes are stress, sedentary lifestyle, weight gain and urbanization [5]. Even though recently many new pharmacological treatment regimens are available, attention is drawn on to the effect of non pharmacological lifestyle interventions on diabetes prevention and treatment [6]. In Asian population, factors like psychological stress, anxiety, depression and decreased sleep hours have become common [7]. Moreover, India has been presently termed as hyperdopaminergic and hyperadrenergic [8]. Diabetes treatment majorly needs behavioural and lifestyle alteration along with standard medical therapy [9], as these changes are known to offset diabetes complications in diabetics and reduce 63%-65% of diabetes risk in prediabetics [10].
Yoga, a traditional mind-body medicine originated 4000 years ago in India, has known history to manage diabetes condition [6]. Yoga therapy includes physical postures (asanas), breathing exercises (pranayama), relaxation and meditation [11]. It is an ingenious technique to attain equilibrium and well-being of mental, physical, emotional and spiritual aspects, thereby improving QoL of the individual [12]. According to Burckhardt CS et al., the QoL is the “ultimate goal of all health interventions” and he has stated QoL as the complete influence of the disease condition not only on the physical or social domains but also on mental well-being [13]. Flanagan QoL scale is a simple questionnaire compared to other health related QoL questionnaires, that has been tested for reliability and validity in diabetes and applicable to wide range across gender, cultural and language groups [14]. A recent report from India in diabetics showed significant improvement in QoL but non significant glycaemic improvement with yogic breathing [9]. Yoga intervention for eight weeks when compared to walking control group reported decreased body weight, reduced Waist Circumference (WC) and mental well-being [15]. IDRS is based on individual’s age, gender, family history of diabetes, WC and physical activity is feasible and helpful than performing Oral Glucose Tolerance Test (OGTT) to screen undiagnosed diabetics in India [16]. When compared to other diabetes risk scores, IDRS is simplified as it uses four easily obtainable risk factors from American Diabetes Association (ADA) recommendation and validated for South Indian population by CURES 10 year follow up study by the Madras diabetes research foundation [16].
Though many reports are available on the management of diabetes with yoga, most of the studies are done, in the elderly diabetic population with more disease duration and/or with other comorbidities, lesser duration of therapy and minimal sample size [12,15,17–19]. It has not been established in prediabetes yet. As hypertension also affects QoL [20], we have included normotensive population to see the effect of glycaemic status on QoL. Till date, to the best of our knowledge, no Randomized Control Trial (RCT) reports are available to show the effect of yoga therapy on QoL and IDRS in the normotensive young adult population with prediabetes and diabetes. Therefore, we have conducted a RCT to see the effect of 12 weeks of yoga therapy along with standard treatment on QoL and IDRS in normotensive Indian adult prediabetics and diabetics.
Materials and Methods
Design: This study used pre and post test randomized control parallel-group trial. It was approved by scientific advisory and Ethical Committee of Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Puducherry, India. This trial has been registered in clinical trial registry of India, with registration number: CTRI/2014/07/004754. The study was conducted from September 2013 to April 2016. The pre and post test assessment was done at 0 and 12 weeks respectively.
Sample: Sample size was calculated to be 62 in each group in order to detect a difference of 6 mg/dl of FPG in prediabetes with yoga and prediabetes without yoga. Standard deviation for prediabetes with yoga and prediabetes without yoga is 11.7 and 10.8 respectively [12]. Calculations were based on two sided CI of 95%, power of 80% and dropout rate 10% by using Open-Epi software.
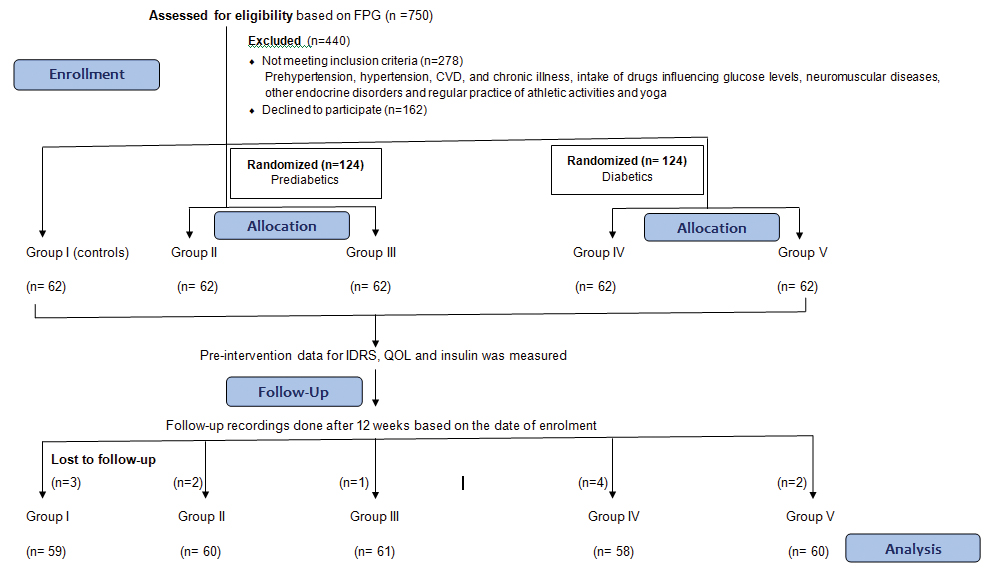
Volunteers in the age group of 18-45 years were screened for prediabetes and newly diagnosed diabetic cases were enrolled from Endocrinology OPD of JIPMER. Among 750 screened individuals, 278 subjects with prehypertension, hypertension, cardiovascular disease and chronic illness, intake of drugs influencing glucose levels, neuromuscular diseases, other endocrine disorders and regular practice of athletic activities and yoga were excluded. Among 440 excluded individuals, 162 subjects declined to participate in the study. Normotensive participants (n=310, systolic and diastolic blood pressure: 100-119 mm Hg and 60-79 mm Hg) were divided into healthy controls (Group I) (n=62, FPG: 60-99 mg/dl), prediabetics (n=124, FPG: 100-125 mg/dl) and diabetics (n=124; FPG ≥126 mg/dl) based on ADA 2013 criteria [21]. Computer generated random numbers and sealed opaque envelope technique was used to allocate study subjects into following sub groups Group II (n=62, prediabetes- standard treatment), Group III (n=62, prediabetes- standard treatment + yoga therapy), Group IV (n=62, diabetes- standard treatment) and Group V (n=62, diabetes- standard treatment + yoga therapy) [Table/Fig-1].
Consort flow chart; Group II and IV: Standard treatment; Group III and V: Standard treatment + yoga.
Written informed consent was obtained from all the subjects before the initiation of the study. Their personal history like dietary habits, smoking, alcoholism, physical activity, occupational status, family history of hypertension/diabetes/cardiovascular disease and medical history were obtained. The person who assessed the outcomes was blinded.
Biochemical measures: After overnight fasting, subjects were asked to report at 8 am to the cardiovascular research laboratory of Physiology and five ml of blood sample was drawn with venipuncture under aseptic precautions. The FPG was estimated by glucose-oxidase peroxidase method (Genuine Biosystem, Chennai, India) and fasting Insulin by ELISA kit (BIORAD Evolis system, Marnes-La-Coquette, France). Homeostatic model assessment of insulin resistance (HOMA-IR) was calculated using the formula: fasting insulin (μIU/ml) × fasting glucose (mg/dl)/405 [22].
Anthropometric measures: Subject’s height (cm), weight (Kg), waist circumference (cm) and hip circumference (cm) were measured to calculate Body Mass Index (BMI) and Waist-Hip Ratio (WHR).
Blood Pressure (BP): Systolic and diastolic blood pressure was recorded by using automatic BP monitor (Omron, SEM-1, Kyoto, Japan) to exclude the subjects with prehypertension and hypertension.
Indian diabetes risk score (IDRS) [16]: To calculate diabetes risk score, IDRS questionnaire that was based on age, gender, family history of diabetes, WC and physical activity was used. An IDRS value ≥60 has the optimum sensitivity (72.5%) and specificity (60.1%) for determining diabetes. It has the accuracy of 61.3%, positive predictive value of 17.0% and negative predictive value of 95.1%.
Quality of life scale (QoL) [14]: Subject’s QoL was assessed using Flanagan QoL scale. It is a questionnaire consisting of 16 items, which includes social well-being, material and physical well-being, relationship with peers, personal development and fulfilment, recreation and independence. Subjects were encouraged to attend each question even if they are not presently involved in it. Scoring was done by summing up of items, to make a total score ranging from 16 to 112. Average total score of healthy individuals is about 90.
Intervention: During the 12 weeks study period, Group I was asked not to change their lifestyle. Group II and Group IV subjects received standard treatment as advised by the clinician and followed the treatment during the study period. They were advised to take up walking for 45 minutes duration three times/week for 12 weeks. Their adherence to treatment was followed up by regular phone contact and with their follow up visits to OPD. Diet pattern was not included in the study. During the 12 weeks of the study period, no major change in physical activity or medication took place which was confirmed by the regular contact with the subjects. Group III and Group V subjects received yoga therapy along with the standard treatment. Under our direct supervision, they underwent yoga therapy as per the module formulated in accordance with guidelines of Morarji Desai National Institute of Yoga (MDNIY) [Table/Fig-2] for three days per week for 12 weeks in Advanced centre for yoga, JIPMER. Each session lasted for 45 minutes. These practices were instructed by qualified and experienced yoga expert. Apart from the therapy sessions under direct supervision, the patients were instructed to do these practices at home. The log book was maintained for yoga therapy sessions, regularity of home practice was monitored by regular phone contact. The yoga therapy module and handouts which contain the instructions of procedures were given to the subjects. There were some patients which lost to follow up at final assessment [Table/Fig-1].
| Sl.No | Yoga therapy module | Duration of practice(in minutes) |
|---|
| 1. | Sukshma vyayama/ loosening exercises | 5 |
| Neck movementsHands stretch breathingElbow flexion and extensionWrist movementsWaist rotationKnee movementsLeg stretch and movementsTadasana breathingKati chakrasana breathing | |
| 2. | Suryanamaskara3 rounds with breathing | 3 |
| 3. | Asana | 15 |
| PadahastasanaKonasanaVakrasanaArdhamatsyendrasanaPaschimottanasanaShalabhasanaDhanurasanaPavanamuktasanaArdha HalasanaSarala Matsyasana | |
| 4. | Pranayama | 10 |
| Nadi Shodhana Pranayama (9 rounds)Bhramari Pranayama (9 rounds)Chandra Nadi Pranayama (9 rounds) | |
| 5. | Meditation | 2 |
| A kara (3 rounds)U kara (3 rounds)M kara (3 rounds)A-U-M kara (3 rounds) | |
| 6. | Relaxation | 10 |
| ShavasanaYoga Nidra & A-U-M Chanting | |
| Total Duration of Practice | 45 |
Statistical Analysis
SPSS version 16.0 for Windows (SPSS Software Inc., Chicago, IL, USA) was used for statistical analysis. Data were expressed as Mean±SD. A Kolmogorov-Smirnov z-test was done for the assumption of Gaussian distribution. The Student’s paired t-test was applied to compare parameters pre and post intervention. The intergroup comparison of parameters was done by One-way ANOVA and post-hoc analysis by Tukey. Statistical significance was considered at p<0.05 and null hypothesis was rejected at p<0.05.
Results
Baseline data of general characteristics and anthropometric measurements is given in [Table/Fig-3]. There was no significant difference in age among three groups. Weight, BMI and WHR showed significant difference in prediabetes and diabetes subjects compared to control subjects, but no difference was found between prediabetes and diabetes group.
Comparison of parameters between controls, prediabetes and diabetes.
| Sl.No | Parameters | Controls(n=62) | Prediabetes(n=124) | Diabetes(n=124) |
|---|
| General characteristics and anthropometric parameters |
| 1 | Age (Yrs) | 36.72±6.12 | 35.81±6.32 | 37.28±6.21 |
| 2 | M/F | 34/28 | 69/55 | 64/60 |
| 3 | Weight (Kg) | 63.12±11.18 | 70.54±7.34* | 73.2±12.26** |
| 4 | BMI (Kg/m2) | 24.55±3.45 | 27.15±3.90*** | 27.65±5.71** |
| 5 | WHR | 0.91±0.05 | 0.94±0.05* | 0.96±0.07*** |
Data are expressed as mean±SD. Comparison of Controls vs Prediabetes and Diabetes is done by Student unpaired t test and denoted by *, Prediabetes vs Diabetes is denoted by #. *p<0.05, **p<0.01, ***p<0.001; †p<0.05, ††p<0.01, †††p<0.001.
BMI: Body mass index; WHR: Waist-hip ratio
Pre and post intervention data of IDRS, QoL and glucose related parameters are given in [Table/Fig-4]. There was no significant difference in group I for all parameters. IDRS, QoL, FPG, fasting insulin and Homeostatic Model Assessment of Insulin Resistance (HOMA-IR) showed significant pre-post difference in all groups but level of significance was more (p<0.001) in Group III and Group V compared to standard treatment groups. Between-group comparison of mean percentage change from baseline of all these parameters showed significant difference (p<0.001) in yoga + standard treatment groups (Group III and Group V) when compared to standard treatment alone and also with healthy controls [Table/Fig-5].
Within group comparison of IDRS, QOL scale and glucose related parameters between controls, prediabetes and diabetes.
| S. No | Parameters | Intervention | Controls | Prediabetes | Diabetes |
|---|
| Group I(n=59) | Group II(n=60) | Group III(n=61) | Group IV(n=58) | Group V(n=60) |
|---|
| 1 | IDRS | Pre | 44.93±9.53 | 73.00±7.88 | 74.59±6.21 | 74.91±7.35 | 75.33±6.50 |
| Post | 44.03±8.75 | 70.00±11.50* | 57.21±10.19*** | 67.02±8.86*** | 58.67±10.16*** |
| 2 | QoL scale | Pre | 90.29±5.60 | 74.17±6.49 | 73.79±6.35 | 66.56±7.08 | 66.78±7.30 |
| Post | 91.63±7.27 | 77.47±7.15** | 85.62±5.77*** | 70.81±7.13** | 82.02±7.74*** |
| 3 | Fasting Plasma Glucose (mg/dl) | Pre | 82.68±9.97 | 113.90±5.04 | 112.18±7.61 | 181.86±27.75 | 195.42±49.93 |
| Post | 83.90±9.49 | 111.43±6.73** | 83.43±12.91*** | 162.33±27.67** | 152.33±31.26*** |
| 4 | Fasting insulin (μIU/ml) | Pre | 5.74±2.20 | 20.87±7.06 | 21.27±6.70 | 32.48±9.53 | 32.02±9.06 |
| Post | 5.98±1.99 | 18.44±7.59** | 12.01±5.94*** | 27.07±8.14** | 20.35±8.61*** |
| 5 | HOMA-IR | Pre | 1.18±0.48 | 5.87±2.00 | 5.89±1.90 | 14.69±5.41 | 15.40±5.69 |
| Post | 1.25±0.46 | 5.10±2.16** | 2.48±1.33*** | 10.97±4.43** | 7.54±3.21*** |
Data are expressed as mean±SD . Comparison of pre vs post is done by Student’s paired t test and p value is denoted by *. *p<0.05, **p<0.01, ***p<0.001. Group II and Group IV: Standard treatment; Group III and Group V: Yoga + Standard treatment.
IDRS: Indian diabetes risk score; QoL: Quality of life; HOMA-IR: Homeostatic model assessment of insulin resistance.
Between group comparison of IDRS and QOL scale and glucose related parameters between controls, prediabetes and diabetes.
| S. No | Parameters | Controls | Prediabetes | Diabetes | ANOVA p-value |
|---|
| Group I(n=59) | Group II(n=60) | Group III(n=61) | Group IV(n=58) | Group V(n=60) |
|---|
| 1 | IDRS | 2.01 | - 4.11 | -23.31 †††,§§§ | -10.49 §§ | -22.12 ‡‡‡, §§§ | <0.001 |
| 2 | QOL scale | 1.54 | +4.45 | +16.03 †††,§§§ | +6.39 § | +22.80 ‡‡‡, §§§ | <0.001 |
| 3 | Fasting Plasma Glucose (mg/dl) | 1.48 | -2.10 §§ | -25.41 †††, §§§ | -10.34 §§§ | -22.05 ‡‡‡, §§§ | <0.001 |
| 4 | Fasting insulin (μIU/ml) | 4.17 | - 11.59 §§ | -43.96 †††, §§§ | -16.64 §§§ | -36.83 ‡‡‡, §§§ | <0.001 |
| 5 | HOMA-IR | 5.90 | -13.10 §§ | -58.75 †††, §§§ | -24.51 §§ | -50.96 ‡‡‡, §§§ | <0.001 |
Data are expressed as mean %ge change from baseline. Group II and Group IV: Standard treatment; Group III and Group V: Yoga + Standard treatment
‘-’ sign indicates decrease and ‘+’ sign indicates increase from baseline.
The intergroup comparison of parameters is done by One-way ANOVA and post hoc analysis by Tukey.
† comparison between group differences in prediabetes. ‡ comparison between group differences in diabetes.
§ represents comparison of prediabetes and diabetes groups with Group I.
†, ‡, § p<0.05; ††, ‡‡, §§ p<0.01; †††, ‡‡‡, §§§ p<0.001.
IDRS: Indian diabetes risk score; QOL: Quality of life; HOMA-IR: Homeostatic model assessment of insulin resistance.
Discussion
QoL is reported to be affected in individuals suffering from diabetes and it influences compliance to treatment [23]. IDRS is a standardized score to assess diabetes risk in the individuals with undiagnosed disease condition [24]. As, there are no reports available, our objective was to assess the effect of yoga therapy on QoL and IDRS in young adult prediabetic and diabetic population.
The findings of this study showed mean percentage reduction in IDRS among participants who underwent yoga along with standard treatment (Group III: 23.31% and Group V: 22.12%) when compared to standard treatment alone (Group II: 4.11% and Group IV: 10.49%) [Table/Fig-5]. This is the first study reporting the effect of yoga therapy on IDRS in prediabetic and diabetic population. IDRS ≥60 has been proved to be useful in determining the prevalence of hypertension, hypercholesterolemia, hypertriglyceridemia, metabolic syndrome and neuropathy [4,24]. Earlier, we have published part of the study reporting decreased QoL and increased IDRS associated with reduced heart rate variability in normotensive young adult prediabetics and diabetics [25]. IDRS was associated with autonomic dysfunction [25], which plays an important role in the pathogenesis of several disease conditions including hypertension [26]. Also, IDRS showed significant association with neuropathy even after adjustment was done for duration of diabetes [24]. Thus, significant decrease in IDRS following 12 weeks yoga treatment indicates the usefulness of yoga therapy in improvement of the metabolic and cardiovascular dysfunctions. There was significant mean percentage increase in QoL scale among study group participants (Group III: 16.03% and Group V: 22.80%) compared to standard treatment alone (Group II: 4.45% and Group IV: 6.39%) [Table/Fig-5]. After 12 weeks, there was significant improvement in QoL and IDRS in Group II and Group IV compared to Group I (control group). Also, these parameters improved in Group II and Group IV post 12 weeks period compared to pre values, which could be due to the effect of 12 weeks of standard treatment alone [Table/Fig-4]. As the standard treatment was common in each group, the significant change in QoL and IDRS score in Group III versus Group II and in Group V versus Group IV could be due to the effect of yoga practice alone. Though the level of significance between groups was almost similar, the mean percentage change was more in yoga groups compared to standard treatment groups. Especially in prediabetics, yoga as add-on therapy along with standard treatment reduces diabetes risk thereby delays the progression into diabetic state. This can be substantiated by significant reduction in FPG, fasting insulin and insulin resistance values in Group III and Group V subjects compared to Group II and Group IV.
This study finding showed significant mean percentage reduction of 10.34 mg/dl in FPG compared to 3.5 mg/dl and 8.24 mg/dl reduction in Chimkode SM et al., and Jyotsna VP et al., studies respectively [19,27]. Chimkode et al., studied effect of yoga on FPG in individuals with 36-55 years of age with atleast one year of disease duration but not on IDRS and QoL in newly diagnosed diabetics and prediabetics. QoL findings in diabetes group were in similarity with a randomized trial conducted by Jyotsna VP et al., [27]. In diabetes patients with more disease duration and age (40-60 years), Jyotsna VP et al., reported significant improvement in QoL in yoga group (n=27) compared to their standard treatment group (n=22) but glycaemic control was non significant [27]. The lack of glycaemic control could be due to less sample size and decreased compliance to yoga with increased age. A pilot study by McDermott KA et al., reported improvement in psychological well-being with yoga similar to present study in individuals of age 37-57 years with high risk for diabetes but in subjects with pre hypertension, there was no significant reduction in fasting plasma glucose [15]. As QoL can be affected by disease duration, aging and other co morbid conditions, we have assessed the effect of yoga in normotensive young individuals (around 18 to 45 years) with newly diagnosed diabetes and prediabetes, which is the novelty of our study.
Improved QoL score among yoga participants implicates the benefit of practicing yoga in alleviating QoL of individuals that helps them to cope-up with day-to-day challenges in life by changing behaviour, relieving stress and anxiety.
Mc Ewen’s theory of allostatic load states that chronic stress changes autonomic nervous system activity and hypothalamic-pituitary-adrenal axis disrupting metabolic, cardiovascular and immune functions of the body [28]. The possible mechanisms of beneficial effects of yoga might be via triggering neurohormonal mechanisms thereby reducing stress and anxiety improving autonomic balance towards parasympathetic activity. Moreover, hypothalamus and striatum, amygdala, hippocampus and prefrontal cortex areas that are expressed with insulin receptors are involved in the pathogenesis of disease conditions with mood and behaviour due to disruption in insulin signalling [29]. Yoga might be improving QoL and well-being by establishing proper insulin signalling in these areas thereby regulating dopaminergic and serotonin neuronal pathways that elevate mood and behaviour [30]. Also, yoga along with standard treatment might be decreasing direct effect of hyperinsulinemia on hypothalamus thereby reducing sympathetic activity and improving parasympathetic activity, improves insulin sensitivity at target tissues and increases peripheral utilization of glucose finally reducing the glucose levels [12]. Therefore, yoga by reducing the diabetes risk score and alleviating QoL is thought to be helpful to delay progression of disease condition from prediabetes to irreversible stages of disease and complications associated with it and also improve glycaemic management, psychological and physical functioning.
Limitation
The screening and diagnosis of the subjects was based on the use of FPG alone on two consecutive values but not on glucose tolerance test. The group activity and the social cohesion also might have improved the scoring of QoL. Yoga therapy for longer duration like one year, having an active control group to counterbalance the effect of social cohesion on QoL of the individuals and addition of diabetes specific QoL questionnaire can be done to have a better understanding of the findings.
Conclusion
Better improvement in QoL was seen in diabetics than prediabetics and reduction in IDRS was comparatively more in prediabetics who were under yoga therapy. Therefore, 12 weeks of yoga when given along with standard treatment improved quality of life and reduced diabetes risk score in prediabetics and diabetics.
Data are expressed as mean±SD. Comparison of Controls vs Prediabetes and Diabetes is done by Student unpaired t test and denoted by *, Prediabetes vs Diabetes is denoted by #. *p<0.05, **p<0.01, ***p<0.001; †p<0.05, ††p<0.01, †††p<0.001.
BMI: Body mass index; WHR: Waist-hip ratio
Data are expressed as mean±SD . Comparison of pre vs post is done by Student’s paired t test and p value is denoted by *. *p<0.05, **p<0.01, ***p<0.001. Group II and Group IV: Standard treatment; Group III and Group V: Yoga + Standard treatment.
IDRS: Indian diabetes risk score; QoL: Quality of life; HOMA-IR: Homeostatic model assessment of insulin resistance.
Data are expressed as mean %ge change from baseline. Group II and Group IV: Standard treatment; Group III and Group V: Yoga + Standard treatment
‘-’ sign indicates decrease and ‘+’ sign indicates increase from baseline.
The intergroup comparison of parameters is done by One-way ANOVA and post hoc analysis by Tukey.
† comparison between group differences in prediabetes. ‡ comparison between group differences in diabetes.
§ represents comparison of prediabetes and diabetes groups with Group I.
†, ‡, § p<0.05; ††, ‡‡, §§ p<0.01; †††, ‡‡‡, §§§ p<0.001.
IDRS: Indian diabetes risk score; QOL: Quality of life; HOMA-IR: Homeostatic model assessment of insulin resistance.