Primary Adenocarcinoma of the Fallopian Tube: A Rare Entity
Ankita Singh1, Sudha Prasad2, Ashok Kumar3, Renu Tanwar4
1 Senior Resident, Department of Obstetrics and Gynaecology, Lok Nayak Hospital, New Delhi, India.
2 Director Professor, Department of Obstetrics and Gynaecology, Lok Nayak Hospital, New Delhi, India.
3 Director Professor, Department of Obstetrics and Gynaecology, Lok Nayak Hospital, New Delhi, India.
4 Professor, Department of Obstetrics and Gynaecology, Lok Nayak Hospital, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ankita Singh, 150, Kadambari Apartments, Sector 9, Rohini-110085, New Delhi, India.
E-mail: drankitasingh@hotmail.com
Primary fallopian tube carcinoma is an uncommon gynaecologic malignancy usually seen in postmenopausal females. We present a case of a 66-year-old postmenopausal female who presented with complaint of blood mixed vaginal discharge on and off for past one month. Workup of the patient revealed no abnormality other than presence of atypical squamous cells on Papanicolaou (PAP) smear. MRI showed mildly bulky cervix with around 4cc fluid in endometrial cavity. As the patient remained symptomatic and fluid in endometrial cavity persisted, total abdominal hysterectomy with bilateral salpingo-oophorectomy was done. On histopathological examination, fimbrial end of left tube had features of poorly differentiated papillary serous adenocarcinoma. Postoperatively, she was given chemotherapy and is doing well with more than 3 years of follow up.
This case highlights the importance of high suspicion in postmenopausal women with bleeding per vaginum, where there is little to suggest clinically or radiologically.
Chemotherapy, Fallopian tube, Post menopausal
CASE REPORT
A 66-year-old female, P3L3, menopausal for 16 years, presented to Gynaecological Outpatient Department with complaint of blood mixed vaginal discharge on and off for past one month. Her bladder and bowel habits were normal. No significant past medical or surgical history was found. Her general physical and abdominal examination was normal. On per speculum examination, cervix was healthy. On vaginal examination, the uterus was retroverted, menopausal in size, firm, mobile with bilateral fornices free. Routine investigations were within normal limits. PAP smear had shown atypical squamous cells. Pelvic sonography showed minimal collection in endometrial cavity with endometrial thickness of 1.8mm. Scanty endometrial and endocervical tissue were obtained on biopsy which had no evidence of malignancy. Four-quadrant cervical biopsy was done which showed changes of chronic cervicitis without dysplasia. CA125 was normal. Repeat ultrasound showed minimal collection in endometrial cavity.
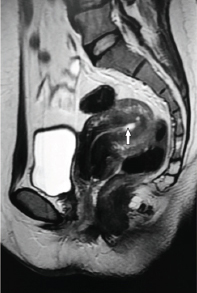
She underwent cervical dilatation and approximately 2cc of serous fluid was drained, which was sent for culture and sensitivity and AFB stain. AFB stain was negative. There was growth of E. coli on culture and Oral Clindamycin was started as per sensitivity report. Patient continued to have vaginal bleeding on and off. MRI of whole abdomen and pelvis showed mildly bulky cervix with around 4cc fluid in endometrial cavity and unremarkable bilateral adnexa [Table/Fig-1]. Patient remained symptomatic as well as fluid in endometrial cavity persisted on repeat ultrasound. Considering history, examination and investigative findings, a provisional diagnosis of dysfunctional uterine bleeding (atrophic endometritis) was made. Patient was counselled that though there is no definite indication for surgery at present, she needs to remain under follow up. As the patient and relatives were very anxious due to on and off bleeding along with presence of atypical cells on PAP smear, they were given option for abdominal hysterectomy with bilateral salpingo-oophorectomy.
Sagittal T2 weighted image: of pelvis shows retroverted normal size uterus with minimal fluid (arrow) in the endometrial cavity in fundal region. The myometrial signal intensity and rest of the endometrium appears normal. Urinary bladder, recto-sigmoid loops and pelvic fat planes are unremarkable.
Patient underwent abdominal hysterectomy with bilateral salpingo-oophorectomy. Intraoperatively, uterus was menopausal (5x3 cm) in size; surface was smooth and normal in appearence. Lateral one third of left fallopian tube was thickened with agglutinated fimbriae. Right fallopian tube was normal looking. Bilateral ovaries were small with normal consistency. The rest of the abdomino-pelvic cavity was normal. Total Abdominal Hysterectomy with bilateral salpingo-oophorectomy was performed. On cut section, endocervical canal, endometrial cavity and myometrium were grossly normal.
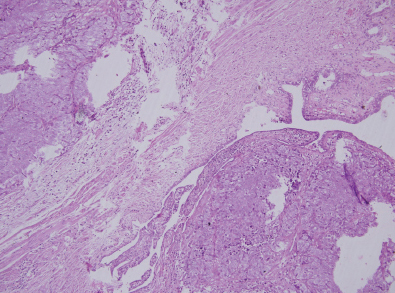
Postoperative period was uneventful. On histopathological examination, fimbrial end of left tube had features of poorly differentiated papillary serous adenocarcinoma. Tumour had transmural infiltration of tubal wall with extension into serosa [Table/Fig-2]. Section from left parametrium and ovary had no deposits (Stage 1c). Postoperatively, her haemogram, liver and kidney function tests were done and she was started on chemotherapy in view of the high grade of the lesion (Grade 3). She received six cycles of cisplatin and paclitaxel. Two unit PCV transfusion was done during chemotherapy due to ensuing anaemia.
Histopathology slide: Wall of fallopian tube with normal mucosa and papillary adenocarcinoma with infiltration in the wall (H & E 20X).
Repeat MRI done after 1 year showed no residual disease. The patient was followed up at regular intervals for three years and was clinically well, with no evidence of disease recurrence or progression.
Discussion
Primary fallopian tube carcinoma is an uncommon gynaecologic malignancy contributing to approximately 0.14% -1.8% of female genital tract malignancies [1]. Literature has reported around 1,500 to 2,000 cases of fallopian tube cancer worldwide [2]. They can at times present in atypical circumstances Which require high suspicion on the part of clinician for diagnosis.
Primary fallopian tube carcinoma is mostly seen in postmenopausal females, with a median age of 52 years [3]. Around 80% of the tubal carcinoma is metastatic, mainly from ovarian, endometrial and gastrointestinal cancers [4]. The aetiolgy of the disease is not known. It may be associated with chronic tubal inflammation, infertility, tuberculous salpingitis and tubal endometriosis [5,6]. BRCA specific genetic mutations such as BRCA 1 & 2 may increase the susceptibility. The histological and clinical features of fallopian tube cancer and ovarian cancer are quite similar therefore advanced cases may be mistakenly identified as primary ovarian cancer [7-9].
The usual presentation is perimenopausal or postmenopausal vaginal bleeding in about 50% of the patients [2]. It may also present with watery or amber coloured vaginal discharge, pelvic pain which may be coliky as a result of forced tubal peristalsis or dull non specific pain due to distention of tube, pelvic mass or gastrointestinal symptoms. Hydrops tubae profluens is characterised by relief of pain with shrinkage of pelvic mass along with vaginal discharge as a result of filling and emptying of partially occluded fallopian tube [10-12].
On physical examination, a pelvic mass may be there that is occasionally of characteristic sausage shape but in our patient pelvic examination was unremarkable. Latzko’s triad of symptoms, which includes profuse sero-sanguinous discharge vaginally, abdominal or pelvic mass and colicky pain which gets relieved by sudden disappearance of the mass has been reported in only 15% of cases but is pathognomic [13]. Mostly diagnosis is made on the operative table or by histopathology [4] as in our patient.
Most common site for primary fallopian tube carcinoma is ampulla of the fallopian tube. In 10% to 20% of cases, bilateral fallopian tubes were found involved [14]. Around 50% of the tubal carcinomas are serous; rest may be endometrioid, transitional, undifferentiated or other rare epithelial cell types [12].
Imaging modalities like Ultrasound and MRI may not be able to differentiate fallopian tube carcinoma from ovarian cancer unless ovaries are separate from the sausage shaped tubal mass. Fallopian tube carcinoma is often diagnosed incidentally during abdominal hysterectomy with bilateral salpingo-oophorectomy for other indications. Fallopian tube carcinoma should be considered in the differential diagnosis of perimenopausal and postmenopausal females presenting with complaint of complex adnexal masses, unexplained uterine bleeding and abnormal glandular cells on cervico-vaginal smear and negative diagnostic curettage [15].
Fallopian tube carcinoma is surgico-pathologically staged according to the staging classification by the International Federation of Gynaecology and Obstetrics (FIGO) Oncology Committee. Primary fallopian tube carcinoma are managed by surgical staging with cytoreductive surgery to remove the primary tumour along with total Abdominal hysterectomy, bilateral salpingo-oophorectomy and pelvic lymph node resection followed by adjuvant chemotherapy. The current chemotherapy of choice consists of 3-6 cycles of platinum-taxane combination [1]. Median progression free survival at 3 years has been reported to be 67% for patients who underwent surgery followed by chemotherapy [16].
Conclusion
Primary fallopian tube carcinoma is an extremely rare gynaecological malignancy and is generally recognized as a disease of post menopausal women. Preoperative diagnosis is difficult due to silent course of this neoplasm and may be diagnosed first intraoperatively or by pathologist. This case highlights the importance of high suspicion in females with postmenopausal bleeding per vaginum, with a clinically and sonographically normal pelvis.
[1]. Pectasides D, Pectasides E, Economopoulos T, Fallopian tube carcinoma:a reviewOncologist 2006 11(8):902-12. [Google Scholar]
[2]. Roychowdhury J, Panpalia M, A rare case of fallopian tube cancerOnline J Health Allied Scs 2007 4:5-7. [Google Scholar]
[3]. Nag D, Bhaumik P, Nandi A, Samaddar A, Bilateral primary fallopian tube papillary serous carcinoma in postmenopausal woman:Report of two casesJournal of Mid-life Health 2016 7:34-37. [Google Scholar]
[4]. Pardeshi SP, Kulkarni MM, Hishikar VA, Primary fallopian tube carcinomaJournal of Postgraduate Medicine 1996 42(2):59-61. [Google Scholar]
[5]. Tahiri Elousrouti L, Erragad FZ, Jayi S, Hammas N, Harmouch T, Primary Adenocarcinoma of the Fallopian Tube:Report of Two CasesJ Clin Case Rep 2016 6:792 [Google Scholar]
[6]. Navin Noushad S, Suresh Kumar D, Primary fallopian tube cancer:a rare gynecological malignancyAmerican Journal of Cancer Case Reports 2016 4:129-33. [Google Scholar]
[7]. Gadducci A, Landoni F, Sartori E, Analysis of treatment failures and survival of patients with fallopian tube carcinoma:a Cooperation Task Force (CTF) studyGynecologic Oncology 2001 81:150-59. [Google Scholar]
[8]. McMurray EH, Jacobs AH, Perez CA, Carcinoma of the fallopian tube. Management and sites of failureCancer 1986 58:2070-75. [Google Scholar]
[9]. Jeung IC, Lee YS, Lee HN, Park EK, Primary carcinoma of the fallopian tube:report of two cases with literature reviewCancer Res Treat 2009 41(2):113-16. [Google Scholar]
[10]. Horng HC, Teng SW, Huang BS, Sun HD, Yen MS, Wang PH, Primary fallopian tube cancer:domestic data and up-to-date reviewTaiwan J Obstet Gynecol 2014 53(3):287-92. [Google Scholar]
[11]. Lau HY, Chen YJ, Yen MS, Chen RF, Yeh SO, Twu NF, Primary fallopian tube carcinoma:a clinicopathologic analysis and literature reviewJ Chin Med Assoc 2013 76(10):583-87. [Google Scholar]
[12]. Gomes FV, Dias JL, Lucas R, Cunha TM, Primary fallopian tube carcinoma:review of MR imaging findingsInsights Imaging 2015 6(4):431-39. [Google Scholar]
[13]. Ajithkumar TV, Minimole AL, John MM, Ashok kumar OS, Primary Fallopian Tube CarcinomaObstet Gynecol Surv 2005 60:247-52. [Google Scholar]
[14]. Hosokawa C, Tsubakimoto M, Inoue Y, Nakamura T, Bilateral primary fallopian tube carcinoma:findings on sequential MRIAm J Roentgenol 2006 186(4):1046-50. [Google Scholar]
[15]. Madan S, Dalal M, Nanda S, Kumar P, Fallopian tube carcinoma presenting as ovarian mass:a case reportInternational Journal of Community Health and Medical Research 2016 2(1):27-30. [Google Scholar]
[16]. Gemignani ML, Hensley ML, Cohen R, Venkatraman E, Saigo PE, Barakat RR, Paclitaxel-based chemotherapy in carcinoma of the fallopian tubeGynecologic Oncology 2001 80(1):16-20. [Google Scholar]