Ranula is derived from the latin word ‘Rana’ meaning frog, as it resembles the underbelly of a frog. It develops due to trauma or obstruction of the excretory duct of the salivary gland situated in the submandibular or sublingual space [1,2]. In general they are asymptomatic, well circumscribed, fluctuant, bluish coloured swelling present in the floor of the mouth [3].
Sublingual group of ranula or simple ranula are pseudocyst that occurs due to extravasation or retention of mucous in the floor of the mouth. The sublingual-submandibular and submandibular ranula group represent the plunging ranula. This occurs due to herniation of the mucous content through the mylohyoid muscle [2,4]. The prevalence of congenital ranula is 0.74% [5].
Simple ranula is common during the first and second decade of life while plunging ranula occurs frequently during the third decade of life. Females are more commonly affected than males with a ratio of 1:1.4 [3,4]. If left untreated it can cause difficulty in speech and mastication. Acute airway obstruction can also occur in rare cases [6].
The diagnosis of ranula can be made through clinical characteristics, fine needle aspiration and various imaging techniques such as Magnetic Resonance Imaging (MRI) or Computed Tomography (CT). The imaging techniques are useful in knowing the extent of the lesion [4].
Various methods are available for the management of oral ranula. A simple ranula can be treated by marsupilization or sclerotherapy or complete excision of the associated salivary gland [7]. Incidence of recurrence is high in certain type of management.
The aim of this study was to systematically review various techniques that are available in the literature for the management of paediatric oral ranula and to present an analysis on the risk and benefits in each technique.
Materials and Methods
Protocol was developed initially which illustrated the structured question and precise eligibility criteria for selection of articles.
Selection Criteria
Articles which described the clinical management of paediatric oral ranula were entitled for inclusion. Case reports, case series, observational or longitudinal studies were included in the systematic review. Studies on management of ranula in adults, animal studies and reviews were excluded. The intervention and outcome parameters were in accordance with the following PIO criteria.
Structured Question
What is the best mode of management of paediatric oral ranula?
PIO Analysis
Population: Children undergoing treatment for oral ranula.
Intervention: Surgical or chemical management of oral ranula.
Outcome: Success rate or recurrence rate of oral ranula after its management.
Literature Search Strategy
The electronic search was entitled from the inception of database to August 2016. It was carried out in the PubMed, Cochrane Library, Science Direct and Google Scholar databases without language or publication date restriction. The search algorithm was as follows: (Children {Mesh} and Oral Ranula {Mesh}) and Chemical or Surgical intervention {Mesh}. In addition to the electronic search, back referencing of the selected articles were also done. Any article which correlated with the search question was evaluated and their references were manually verified.
Data Collection and Analysis
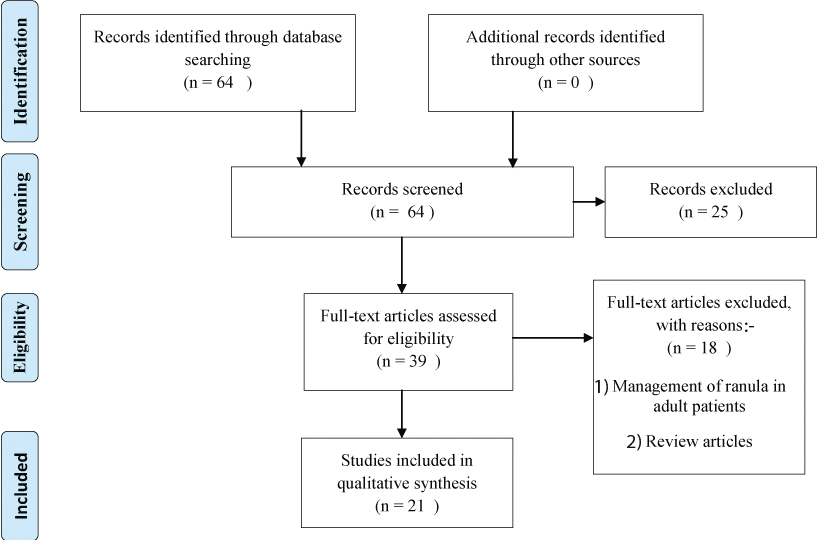
Selection of studies: The articles were primarily evaluated for relevance to the research question on the basis of their title and abstract by two independent reviewers. Based on the preset eligibility criteria, the significant articles were yielded to full text evaluation. Any disagreement was resolved through discussion until a consensus was reached. Ultimately, the acknowledged full text articles were subjected to data extraction, quality assessment and data analysis as depicted in [Table/Fig-1].
Data extraction: Data extraction and assessment was done by two reviewers independently. The following characteristics were assessed: author, year of publication, study design, sample size, intervention, adverse effects and follow up period. In case of any disagreement, joint evaluation was held by the observers until a term was reached.
Results
The search strategy resulted in recovery of 64 articles. After application of the preset eligibility criteria, a total of 21 articles were relevant to present study. The included studies consisted of the following study design: Seven articles were prospective clinical study [4,7-12], four articles were retrospective review [13-16], five articles were case series [17-21] and five articles were case report [6,22-25] as depicted in [Table/Fig-2]. Higher predilection for ranula was seen in female population with a prevalence of 53.56% [12,15].
Description and summary of all included literature data.
| S. No | Author/Year | Patient Detail | Study Design | Finding/Summary | Adverse Effect | Follow Up (in months) |
|---|
| Age (in years) | Sex |
|---|
| 1. | Yang Y and Hong K / 2014 [4] | 0-19 | F-7 M-5 | Prospective cohort study | Intraoral approach for removal of plunging ranula along with the associated salivary gland is a safe and effective surgical approach as a primary treatment modality for plunging ranula. | Nil | 8-43 |
| 2. | Clyburn VL et al., / 2009 [6] | 9 | M -1 | Case report | Resection of the submandibular gland must be considered when there is extension of the ranula into the neck and parapharyngeal space via transcervical approach. | Nil | 60 |
| 3. | Mahadevan M and Vasan N / 2006 [7] | 6-16 | F-7 M-14 | Prospective cohort study | Surgical excision of the sublingual gland and pseudocyst via transoral approach is an effective and safe method for management of paediatric plunging ranula. | Dehydration and haematoma | 24-36 |
| 4. | Fukase S et al., / 2003 [8] | 6-16 | M-9 F- 9 | Prospective cohort study | OK-432 (Picibanil) intracystic injection can replace surgical therapy as it can be done for out patients, its efficacy is high and it is relatively safe. | Fever and local pain in 17 patients. | No recurrence |
| 5. | Roh J-L and Kim HS /2008 [9] | 4-14 | F-5 M-4 | Prospective cohort study | OK-432 intracystic injection is a safe and effective alternative to surgical approach. | Local pain for 2-4 days after treatment | 14-45 |
| 6. | Garofalo S et al., / 2007 [10] | 2 months- 12 | M-4 F-4 | Prospective cohort study | Homotoxicological therapy with nickel gluconate mercurious heel potentised swine organ preparation is an effective primary treatment for management of pediatric oral ranula. | Increased volume and tension for 24 hours and asthenia | 4-32 |
| 7. | Liu Z and Wang B /2015 [11] | Unclear | F-3 M-2 | Prospective cohort study | Anterograde excision of the sublingual gland is a new technique for the management of ranula based on the anatomical characteristics as it reduces the risk of postoperative complication. | Nil | 6-24 |
| 8. | Garofalo S et al., / 2014 [12] | 1-16 | Medical F-8 M-12 Surgical F-9 M-8 | Prospective cohort study | Medical treatment with oral nickel gluconate. Meercurium heel and glandular submandibular sinus injection is more effective than marsupialization with packing because of its lower recurrence rate and fewer side effects. | Swelling, tension, asthenia. Duration of side effect - 2 days | Medical: 18-91 Surgical: 39-57 |
| 9. | Zhao Y-F et al., / 2004 [13] | 1-18 | F-133 M-110 | Retrospective cohort study | Surgical excision of the sublingual gland via an intraoral approach reduced the recurrence of ranula. | Nil | 6 |
| 10. | Yuca K et al., / 2005 [14] | 7-15 | F-6 M-3 | Retrospective cohort study | Marsupialisation is an effective method for management of pediatric oral ranula and in case of recurrence, it should be combined with sublingual gland. | Nil | 16 |
| 11. | Lee H-M et al., / 2006 [15] | 6-16 | F-8 M-5 | Retrospective cohort study | Ok-432 intracystic injection is a safe and effective primary treatment for paediatric oral ranula. | Nil | 5 |
| 12. | Lee DH et al.,/2015 [16] | Unclear | F- 14 M - 10 | Retrospective cohort study | Surgical excision of ranula along with sublingual gland via intraoral approach is the optimum treatment for simple ranula. | Nil | 44 |
| 13. | Hidaka H et al., / 2003 [17] | 5, 18 | F-2 | Case series | Surgical extension of the cyst along with the sublingual gland via intraoral approach is the best approach for the management of plunging ranula. | Nil | 10 |
| 14. | Kobayashi T et al., / 2003 [18] | 9,10 | F-2 | Case series | Surgical excision of the cyst along with the sublingual gland via the intraoral approach must be considered as the first approach for the management of plunging ranula and cervical approach can impair the marginal mandibular branch. | Nil | 16-65 |
| 15. | Ohta N et al., / 2014 [19] | 4-11 | F-3 M - 1 | Case series | OK-432 intracystic injection can be used as a first line of treatment for ranula extending into the parapharyngeal space and the presence of adverse effect such as pain and fever were resolved in few days. | Nil | 12-36 |
| 16. | Bozena S et al., / 2015 [20] | 10 years and 7 months | M-2 | Case series | Surgical excision of the cyst along with the sublingual gland using the transcervical approach. | Nil | Nil |
| 17. | Lai JB and Pooncy /2009 [21] | 6, 30, 32 | F-2 M-1 | Case series | Carbon dioxide laser excision of ranula is safe with minimal or no recurrence. | Nil | Nil |
| 18. | Bernhard MK et al., / 2007 [22] | 33 weeks | M-1 | Case report | Congenital cysts must be observed for potential resolution for several months in uncomplicated cases. | Nil | 4 |
| 19. | Rashmi SC et al., / 2014 [23] | 14 | F-1 | Case report | Marsupialisation of the cyst was done. | Nil | 24 |
| 20. | Aybars O et al., / 2013 [24] | 15 days | F-1 | Case report | Surgical excision of the cyst was done. | Nil | 10 |
| 21. | Sirin M et al., / 2016 [25] | 4 months | F-1 | Case report | Surgical excision of the cyst along with the sublingual gland using the transcervical approach. | Nil | Nil |
Various methods of management of paediatric ranula were given. Surgical management was described in detail in 13 articles [4, 6, 7, 11, 13, 14, 16-18, 20, 23-25]. Two types of non surgical management were described in five articles [8-10,15,19]. Management of paediatric ranula by OK-432 (picibanil) was described in four articles [8,9,15,19]. The other article described the use of oral Nickel gluconate, mercurius heel and glandula submandibularis suis D10/D30/D200 for non surgical management [10]. One article compared the treatment outcome of surgical management with that of non surgical manangement (nickel gluconate) [12]. The use of carbon dioxide laser was described by one author [21]. Gradual regression of ranula on its own in an infant was evaluated in one article [21].
Harmful outcome such as fever and local pain was associated after administration of OK-432 for two to four days [8,9]. Postoperative deleterious outcome that was associated with oral administration of nickel gluconate mercurius-heel and glandula submandibularis suis D10/D30/D200 was increase in volume and tension of the swelling, which diminished in 24 hours [10,12]. The negative consequences, such as haematoma and dehydration were observed in three children after surgical approach [7,18]. The follow up period of all cases, varied from three weeks to 91 months.
Discussion
Ranula is a cystic lesion that arises in the floor of the mouth. Formation of the cyst is attributed to the traumatic rupture of the excretory salivary duct [2,4]. This leads to extravasation and accumulation of the saliva within the tissue. This was represented by the experimental design conducted by Bhaskar SN et al., [26]. The sublingual and submandibular spaces are separated by the mylohyoid muscle. Presence of mylohyoid boutonnieres and the projection of salivary tissue through these defects can result in plunging ranula.
Only 21 articles fulfilled the preset eligibility criteria for our current systematic review. The majority of the published articles consisted of prospective cohort study with a few being case report, case series and retrospective cohort study. This can limit the reliability of our result to a certain extent. This places a constraint on doing a quality appraisal of the selected articles.
The prevalence of paediatric ranula was 1.15:1 (F:M) in our review with a slight predilection towards the female population. This is similar to the result given by Langlois NEL and Kolhe P [27]. Patient were symptomatic in case of extensive plunging ranula, in which, they exhibited difficulty in breathing when the cyst extended into the parapharyngeal space [6]. Out of 17 studies, only two articles reported the aetiology of ranula [10,17]. The most common aetiology was attributed to previous surgery and trauma.
Diagnosis
The diagnosis of ranula can be done by aspiration technique (FNAC), MRI, Ultrasound or CT. In FNAC, the aspirated liquid appears to be highly viscous in nature, with salivary content [19]. This was employed in three studies after application of topical anaesthesia [7,19,24]. CT scan was done in four studies to know the extent of plunging ranula [9,11,16,20]. The investigation method which does not require exposure to radiation was ultrasound and MRI which was utilized in a single and five selected articles respectively [6,9,10,12,17,18]. Therefore, it can be recommended that the choice of investigation can depend on the size of the lesion. If the size of the cyst is greater than 2 cm in diameter, or of plunging type, investigation such as MRI, CT or ultrasound is advocated. If the cyst size is less than 2 cm, FNAC was employed to aid in the diagnosis of the condition [19].
Management
The management of ranula initially was done by surgical method. With the advent of technology, newer non invasive medical management and use of laser have gained acknowledgement in the management of ranula [21]. In case of congenital ranula, the patient should be under observation for six months, before proceeding with any treatment, as reported by Berhnard MK et al., [22].
The prevalence of surgical technique for the management of ranula was 80.47%., which was employed in 13 selected articles [4,6,7,11,13,14,16-18,20,23-25]. The most common advocated technique for the management of ranula in earlier days was marsupialisation. It had high recurrence rate of 61%-89% as the cyst was not completely excised. In some instances, it served as a precursor for plunging ranula. The packing of the ranula cavity with gauze after marsupialisation was found to be effective in curtailing the recurrence rate. It is generally recommended for cyst less than 2 cm in diameter [28].
In order to evade this problem, Yang Y and Hong K recommended removing the cyst along with the sublingual gland [4]. Removal of submandibular gland was recommended in plunging ranula, extending into the parapharyngeal space [6]. The surgical excision can be carried out via transcervical or transoral approach. Transcervical approach is commonly employed in en bloc resection of the cyst, as it is difficult to obtain a substantial cervical extension through intraoral approach. Probability of injury to the marginal mandibular, lingual and hypoglossal nerves are common in transcervical approach. Also, there is a risk of orocervical fistula formation and cervical scar in the cervical approach. The choice of incision should be based on the extension of cyst to avoid unwanted complications [4,13,17].
OK-432: Ogita S et al., introduced OK-432 (lyophilized streptococcal preparation) for lymphangioma [29,30]. As ranula is a cystic disease resembling lymphangioma, with a thin cyst wall, it was considered as an alternative approach to surgical management. This technique was employed by four authors, with a prevalence of 11.6% [8, 9, 15, 19]. It is administered in form of injection with a dose of 0.1 mg-0.2 mg [9]. Picibanil causes inflammatory reaction, which leads to the collapse of the pseudocyst wall [31, 32]. The complications associated with this are fever and pain which subsided within two to four days [8, 9].
Homotoxicological drug: Another non invasive technique to overcome the side effect of OK-432 was nickel gluconate- mercurius heel- potentised swine organ preparation (a homotoxicological drug). This homotoxicological drug was tested by two authors, with a frequency of 7.3% [10,12].
The duration of oral administration of the drug varied from six weeks to a maximum of months. These drugs accelerate pseudocyst resorption, glandular repairing and physiological function [10]. They showed higher success rate in large lesion, as there is increased sensitivity to the action of drugs due to high vascularity. The side effect associated with this, are, increased volume and tension in the swelling for 24 hours and asthenia [10,12].
Laser: In 1985, Frame JW introduced laser for the treatment of ranula [33]. Ranula has a high water content, which is vaporized by carbon dioxide laser. The heat generated causes coagulation of blood vessels resulting in haemostasis. It has enhanced depth perception when compared to scalpel. There is decreased risk of injury to the nerve and submandibular duct. There is a chance of less tissue scarring and this is required for normal tongue movement during speech and swallowing. This method was explained by Lai JB and Pooncy had a high success rate [21].
Based on the above included articles, it can be concluded that marsupialisation can be carried out, if the cyst size is less than 2 cm. More information is needed on medical management of ranula with well formulated study design and the availability of medicine in the market. Carbon dioxide laser is effective in management of paediatric ranula, with limited side effects but many randomized trials are required. In case of recurrence of ranula, surgical approach with the removal of associated salivary gland is the best treatment option. Medical management had a recurrence rate of 0.52% [9,10].
Limitation
The paucity of original research in the management of paediatric ranula and the low level of evidence in the selected articles limit the ability to make decision on preferred management. In some cases, the sample size was small with limited follow up period. This may lead to the ignorance of long term side effect of each management and their reversal. Information regarding the allergic nature of the drugs was limited.
Conclusion
The data obtained from the review, display a lack of high quality study, with proper sample size and adequate follow up period. Further, randomized clinical trials are required, for forming a reliable scientific evidence, that can guide the paedodontist in formulating a best treatment option in case of paediatric oral ranula.