EPH, defined as hysterectomy performed at the time of child birth or within 24 hours of child birth or at any time from childbirth to discharge from the same hospitalization [1], is a relatively infrequent procedure in present day obstetrics. It is performed in cases of intractable obstetric haemorrhage due to uterine atony or to prevent haemorrhage from a morbidly adherent placenta or placenta previa. Other indications include uterine rupture, cervical laceration, leiomyoma, postpartum uterine infection or invasive cervical cancer. Consequentially, the risk factors for EPH are similar to those that predispose to haemorrhage or abnormal placentation. The incidence of EPH ranges from 0.035% to 0.54% worldwide [2–11]. The incidence is high in developing countries when compared to developed nations. This could be attributed to the disparity in the accessibility and availability of various modern obstetric services like uterine artery embolisation, family planning and antenatal care facilities.
This retrospective study was conducted as a clinical audit of peripartum hysterectomies performed over a period of approximately 14 years at our institution. Through this audit, we aimed to assess the incidence of peripartum hysterectomies, identify the risk factors, indications and complications including the mortality and morbidity associated with the procedure. Audits of emergency obstetric procedures like EPH serve as a reflective practice for the authors and add to the existing literature regarding the changing trend of risk factors and incidence of EPH.
Materials and Methods
This retrospective study was conducted at a 650 bedded, tertiary care teaching hospital in southern India. Institute Ethical Committee clearance was obtained for this study and waiver of concent was granted (Ref. no. IEC:RC/16/66). No patient identifiable information was used in the study.
All women who underwent child birth and underwent hysterectomy for obstetric indications, either during child birth or within the immediate postpartum period between February 2002 and December 2015 were included in the study.
STATISTICAL ANAYLSIS
Their demographic characteristics, antenatal risk factors, antepartum, intrapartum and postpartum events, transfusion of blood and blood products, Intensive Care Unit-Length of Stay (ICU-LOS) and postoperative complications were entered in Microsoft excel spreadsheet and analysed using SPSS software version 22.0. For categorical variables, data was compiled as frequency and percent. For continuous variables, data was calculated as mean±SD.
Results
There were total of 16,473 deliveries over the study period and peripartum hysterectomy was performed in 12 cases making an incidence of 0.073%. The women were aged 20 to 40 years, with a mean age at the time of childbirth being 30.25±4.3 years. Among these women, 83% were multiparous and mean gestational age at child birth was 36.70±4.00 weeks. Six women had a previous Lower Segment Caesarean Section (LSCS) accounting for 50% of the cases [Table/Fig-1]. The most common indication of EPH was uterine atony followed by placenta percreta and traumatic postpartum haemorrhage due to uterine rupture [Table/Fig-2].
Risk factors for peripartum hysterectomy.
| Risk factors | Number of women (%) |
|---|
| Age (years)21-2526-3031-3536-40 | 3 (25.0)4 (33.3)4 (33.3)1 (8.3) |
| ParityP1P2P3P4P5 | 2 (16.7)4 (33.3)5 (41.7)0 (0)1 (8.3) |
| Previous caesarean deliveryNoneOneTwo | 6 (50)4 (33.3)2 (16.7) |
| Previous uterine cavity instrumentationNoYes | 9 (75.0)3 (25.0) |
| Twin gestationNoYes | 11(91.7)1 (8.3) |
| Maturity at delivery Preterm (<37weeks)Early term (37-38+6 weeks)Full term (39-40+6 weeks)Late term (41-41+6 weeks)Post term (>42weeks) | 5 (41.7)3 (25.0)4 (33.3)0 (0)0 (0) |
| Type of labourNo labourSpontaneousInduced | 1 (8.3)6 (50.0)5 (41.7) |
| Mode of deliverySpontaneous vaginalAssisted vaginalCesarean delivery | 2 (16.7)2 (16.7)8 (66.7) |
Indication for emergency peripartum hysterectomy.
| Indication | No. of cases (%) |
|---|
| Uterine atonicity | 7 (58.3) |
| Rupture uterus | 2 (16.7) |
| Adherent placenta (accreta, increta, percreta) | 2 (16.7) |
| Secondary postpartum haemorrhage | 1 (8.3) |
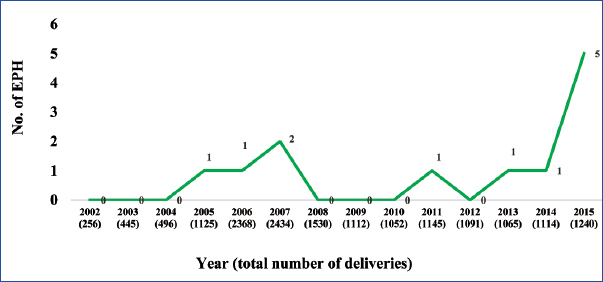
The most common type of child birth preceding hysterectomy was caesarean section, accounting for 66.6%. Subtotal hysterectomy was more commonly performed (66.6%) than total hysterectomy. There was one intrauterine foetal demise accounting for 8% of perinatal mortality and two women (16.6%) could not be revived even after hysterectomy. All 12 patients were admitted to the intensive care unit, for better monitoring. At least half of these women required inotropic support. Average length of ICU-LOS was 3.32±1.6 days and hospital stay was 14±6.7 days. There was an increase in incidence of peripartum hysterectomies noted over the years (2002-2005, 0.043%; 2006-2010, 0.035%; 2011-2015, 0.141%) with clustering of cases in one year (five cases in 2015) [Table/Fig-3]. The average requirement of blood and its products was 7.64±5.8 units.
Trends of emergency peripartum hysterectomy.
The various maternal complications were disseminated intravascular coagulation, Transfusion Related Acute Lung Injury (TRALI), pulmonary atelectasis, vocal cord palsy, bladder injury and acute kidney injury. Their incidences are depicted in [Table/Fig-4]. Uterine and internal iliac artery embolization was performed in two cases after hysterectomy as they continued to bleed postoperatively. However, these patients died due to disseminated intravascular coagulation.
Complications of peripartum hysterectomy.
| Complication | Number of women (%) |
|---|
| Maternal |
| Febrile morbidity | 5 (41.7) |
| Wound sepsis | 3 (25.0) |
| Coagulopathy | 5 (41.7) |
| Bladder injury | 1 (8.3) |
| Acute renal failure | 1 (8.3) |
| Pulmonary atelectasis | 2 (16.7) |
| TRALI* | 2 (16.7) |
| Vocal cord palsy | 1 (8.3) |
| ICU admission | 12 (100.0) |
| Need for vasopressors | 6 (50.0) |
| Mortality | 2 (16.7) |
| Foetal |
| Neonatal ICU admission | 4 (33.3) |
| Perinatal mortality | 1 (8.3) |
TRALI -Transfusion Related Acute Lung Injury
Discussion
The incidence of peripartum hysterectomy in the present study was 0.073%, which is slightly higher than those of the developed countries like UK and Nordic countries [2,4]. The incidence of EPH is much higher (0.2% to 0.54%) in studies from Northern India, Pakistan and Nigeria [10–12]. Atonic postpartum haemorrhage is a common complication of grand multiparity and the high percentage of grand multiparous and unbooked women in these studies may be the reason for a higher incidence of EPH. Grand multiparity is not as common as it was in some of the other studies due to the higher acceptability of family planning services (61%) in our region, especially female sterilisation after two successful child births [13].
The incidence of EPH in our study was observed to have increased over the years, from 0.043% between 2002-2005 to 0.141% between 2011-2015. A similar increasing trend was noted in a population based study by Orbach A et al., [14]. The factors contributing to this increasing trend in our study may be related to an increase in the caesarean delivery rates (both primary and repeat caesarean deliveries) at our centre, from 21% in 2002 to 31% in 2015. On the other hand, one study from China reported a decreased incidence of pH (0.157% in 2005 to 0.133% in 2008), which was attributed to a corresponding increase in rates of uterine artery embolization.
In the present study, half of the women had atleast one prior caesarean section. This is in agreement with most studies [3,5,6,8,9] from various parts of the world which found 50% to 83% of the women who underwent EPH had a prior caesarean section. The United Kingdom Obstetric Surveillance Study (UKOSS) which was population based study, concluded that the risk of an EPH rises with increasing number of previous caesarean sections [4].
The most common indication for EPH in our study was atonic postpartum haemorrhage, followed by adherent placenta and rupture uterus. This is consistent with studies reporting a similar low incidence of EPH [3,6]. In contrast, some studies reported rupture uterus to be the most common indication for EPH, followed by placental causes and uterine atonicity [8,10,12,15]. This observation could be related to the higher incidence of grand multiparity seen in these studies. Cho GJ et al., and Chen J et al., observed a change in most common indication from atony to abnormal placentation, which could be attributed to their high rate of caesarean sections [7,9].
The most common type of child birth preceding the EPH was a caesarean section rather than a vaginal delivery, as was the case with majority of studies [3,5,6,8]. The perinatal mortality was low in our study (8%), compared to other studies which reported rates of 37% to 64%. This may be due to higher rates of rupture uterus in these studies, which is known to have a detrimental effect on perinatal outcome [6,10,12,15].
Maternal mortality in our study was due to disseminated intravascular coagulation which was a consequence of the intractable haemorrhage. The maternal mortality reported in most studies was attributed to haemorrhagic shock or disseminated intravascular coagulation in the setting of massive obstetric haemorrhage which could not be controlled even after hysterectomy [3,6,8,11,12]. The UKOSS concluded that more than 150 women were managed successfully with an EPH for each woman who died after the procedure [4]. Deaths were due to the severity of the underlying haemorrhage for which hysterectomy was performed, rather than the procedure itself.
There has been a significant fall in the maternal mortality rates across the globe due to advancements in technology, uterotonics and surgical techniques. However, the most common reason for performing an EPH is still postpartum haemorrhage in developing countries. With increasing rates of caesarean section and its associated rise in placenta previa and placenta accreta, the incidence of EPH is expected to rise world over. Regular audits are needed to curb the caesarean section rates and its accompanying complications. Careful antenatal assessment and early recognition of risk factors for haemorrhage should be accompanied by arrangements for adequate uterotonics and blood products for early resuscitation.
The threshold for performing an EPH will depend on haemodynamic stability of the patient and the surgical expertise of the obstetrician with regard to conservative procedures like B-Lynch sutures, uterine and internal iliac artery ligation. Early intervention by a senior experienced obstetrician well versed with conservative measures to preserve the uterus where possible may prevent an overzealous inexperienced surgeon attempting an EPH. Subtotal EPH may be a better choice when surgery needs to be completed in a shorter time before the onset of haemodynamic instability. The complications following EPH like ICU admission and need for blood transfusions are also mostly due to the underlying haemorrhage. However, urological injuries, febrile morbidity, wound infection, prolonged hospital stay, due to the EPH is influenced by technique and skill of operating surgeon, availability of blood products, adequate antibiotic cover and intensive care management. Performance of EPH by an experienced surgeon is reported to significantly reduce the operating time, number of units of blood transfusion and hospital stay. An informed consent regarding the possibility of EPH and ensuring the availability of a consultants while managing a high risk parturient can prevent mortality. Although, EPH marks an abrupt end to the reproductive career of a woman, it is an acceptable alternative where expertise or facilities for more complex modalities of management, such as uterine artery embolization may not be available.
Limitation
It is a single centre retrospective study. Also, we could not determine the reason for the clustering of cases in the year 2015. It remains to be seen whether this is indicative of a further rising trend of EPH in the future or merely due to chance. It is also expected that the principal indication for EPH is likely to change to abnormal placentation as our caesarean section rates are rising.
Conclusion
Atonic postpartum haemorrhage was the most common reason for performing an EPH. Women with previous caesarean section are at increased risk, both due to atonic and traumatic postpartum haemorrhage. Peripartum hysterectomy is life saving, if performed at the appropriate time. Most of these patients require intensive monitoring. The need for a stringent protocol for managing postpartum haemorrhage cannot be overemphasised. Although EPH is infrequent in modern obstetrics, its rising incidence and its association with the mode of delivery and prior caesarean section reiterates the need for curtailing the caesarean section rates. Regular departmental audits are needed to formulate appropriate protocols to decrease mortality and near miss events like EPH.
*TRALI -Transfusion Related Acute Lung Injury