Dengue is a vector borne viral fever and has varied ocular affections. We report two cases of Dengue Associated Maculopathy (DAM). The first patient was a 22-year-old lady with dengue fever, presented with diminution of vision in the left eye with best corrected visual acuity of 20/40. Fundus revealed soft exudates and streak haemorrhages at the macula in the left eye. Optical Coherence Tomography (OCT) showed cystoid macular oedema. She recovered completely within four days. The second patient was a 33-year-old lady with dengue, with blurred vision in the left eye and with a visual acuity of 20/80. Fundus examination in the left eye revealed elevated fovea with a yellow well circumscribed lesion with surrounding striations. OCT showed features suggestive of foveolitis. She improved spontaneously over the next 21 days to a visual acuity of 20/20p. DAM is usually a self-limiting condition with favourable prognosis. This report highlights the importance of anticipating visual morbidity in patients with dengue and a thorough evaluation and follow-up in spite of its benign behaviour. Also, this report highlights the importance of OCT in differentiating various presentations of DAM.
Central scotoma, Cystoid macular oedema, Dengue associated maculopathy, Foveolitis
Case Report
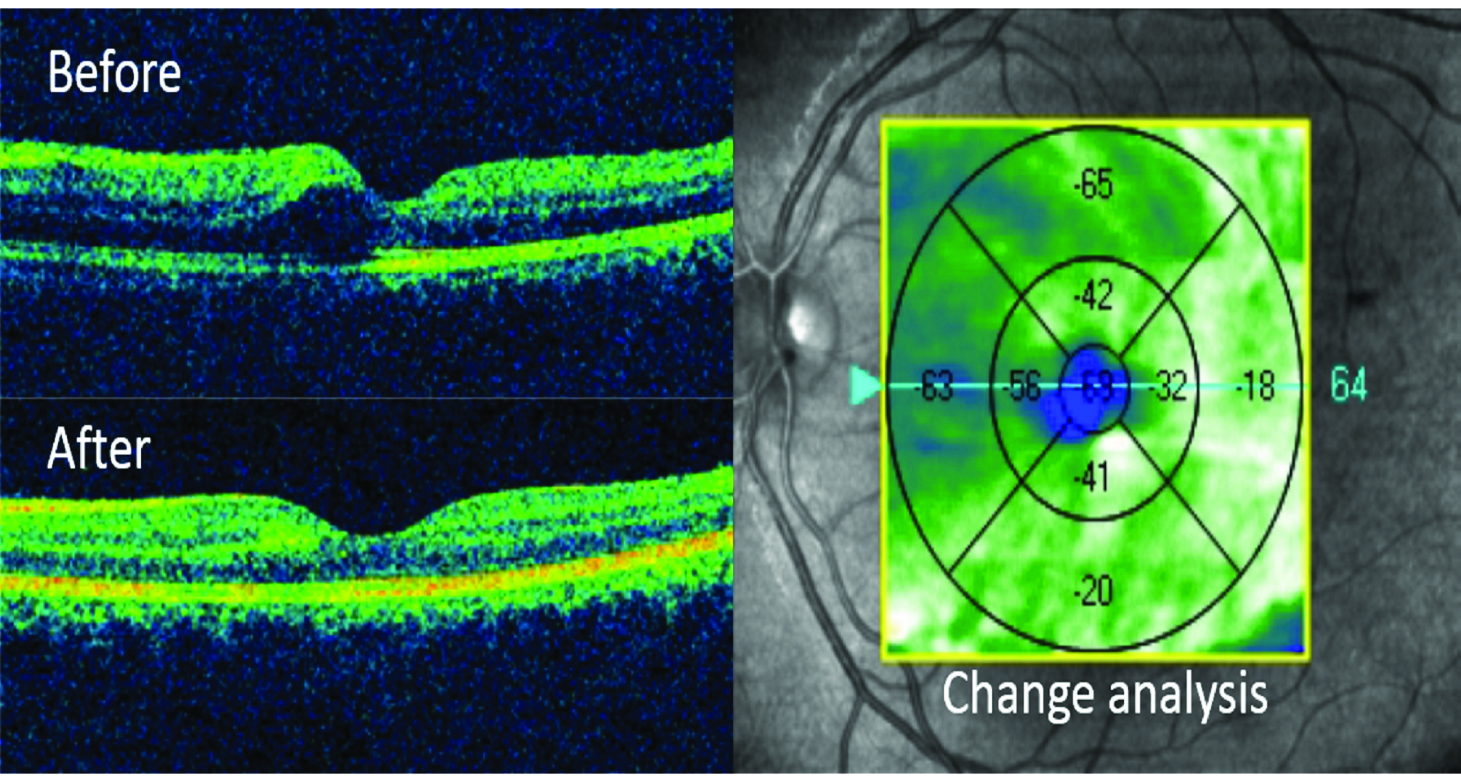
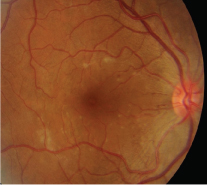
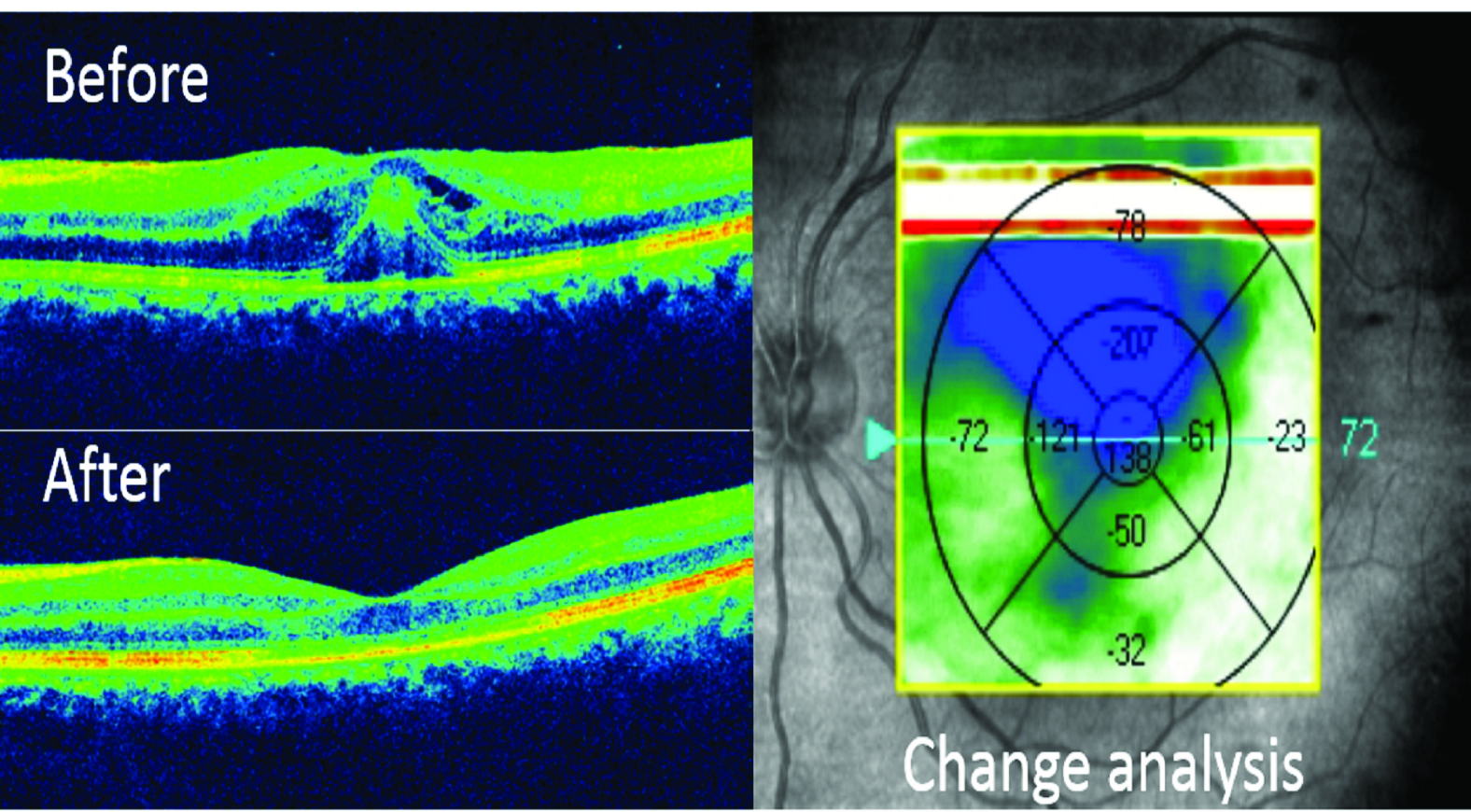
A 22-year-old girl with dengue fever and thrombocytopenia (64,000/cu. mm) was referred for unilateral sudden painless diminution of vision on the fourth day of fever, when she was convalescing from the infection. On examination, best corrected visual acuity in the right eye was 20/20 and in left eye was 20/40. Amsler grid showed a central scotoma in the left eye. Anterior segment and intra ocular pressure were well within normal limits. Fundus examination revealed increased reflexes at the macula in the right eye, whereas there were streak macular haemorrhages with soft exudates, in the left eye [Table/Fig-1,2]. An Optical Coherence Tomography (OCT) was performed. Right eye macula was normal, however left eye showed cystoid spaces in the outer nuclear layers suggestive of cystoid macular oedema [Table/Fig-3]. Other causes of cystoid macular oedema were ruled out, there was no history of trauma, intraocular surgery and Erythrocyte Sedimentation Rate (ESR) and blood sugars were normal. However, other causes of vasculitis were not ruled out. On the basis of this clinical framework, a diagnosis of DAM was made. As there are no proven treatment guidelines, we opted for observation. She recovered remarkably with full anatomic resolution over the next four days, without specific treatment. Visual acuity was 20/20 and central scotoma had disappeared. OCT was within normal limits [Table/Fig-4], her platelet count being 1,78,000 /cu.mm.
Fundus of the right eye, in patient 1: demonstrating increased reflexes at the macula, inferior to fovea, rest of the fundus is unremarkable.
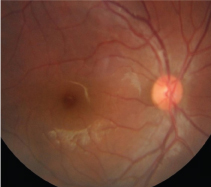
Fundus of the left eye, in patient 1: streak haemorrhages at macula with soft exudates, absence of foveolar reflex, rest of the fundus is unremarkable.
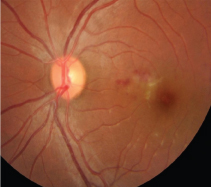
Optical coherence tomography, macular thickness profile (patient 1) showing normal foveal curvature in the right eye (above insert) with a normal central subfield thickness (274μm) and left eye had cystoid space in the inner retinal layers with nasal macular thickening (below insert) and a central subfield thickness of 294 μm.
Optical coherence tomography (patient 1) of left eye demonstrating a macular thickness change analysis from before (above insert) with cystoid space in the inner layer of retina to normal foveal contour after four days of observation. (below insert)
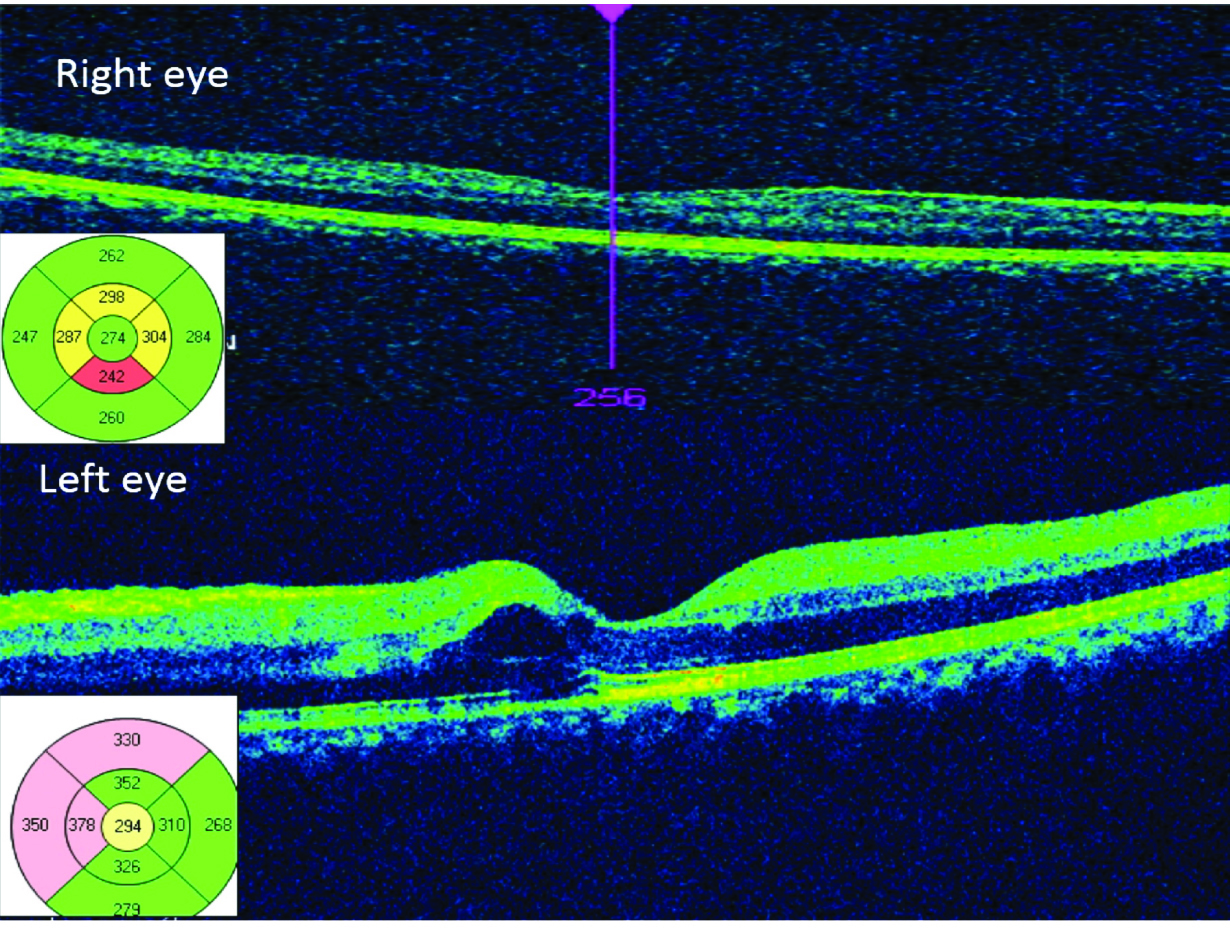
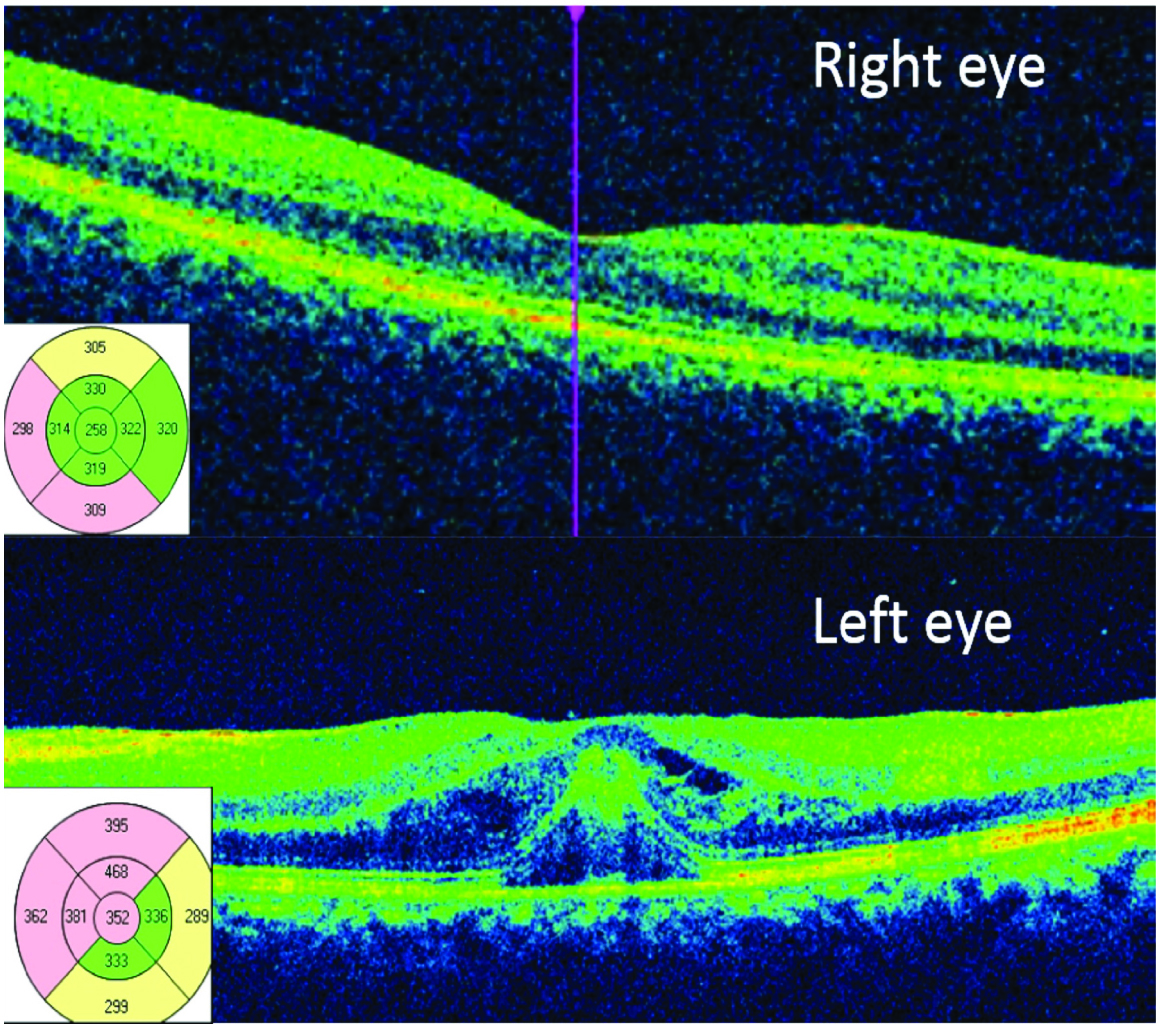
The second patient was a 33-year-old lady, referred by her physician for assessment of low visual acuity in the left eye that commenced on the seventh day of fever, when she was convalescing from dengue. Her serial platelet count was at its nadir of 68,000/cu.mm. On examination, best corrected visual acuity in the right eye was 20/20 and in the left eye was 20/80. Amsler grid showed a central scotoma. Anterior segment and intraocular pressure were normal. Fundus examination of the right eye revealed hyperemic disc and a few blot haemorrhages were noted temporal to the disc. Macula had a few discrete subretinal yellow lesions in the right eye. However, fovea was normal [Table/Fig-5] in the left eye, disc was mildly elevated and was hyperemic, subretinal discrete yellow lesions in the macula, with interspersed splinter haemorrhages were noted. The fovea was elevated with a yellow well circumscribed lesion at the centre surrounded by striations [Table/Fig-6]. OCT was essentially normal in right eye, whereas in the left eye, showed distortion of the foveal contour, cystoid pockets in the inner retinal layers and an elevated hyper reflective lesion arising from the inner segment-outer segment junction entering the outer nuclear zone consistent with foveolitis [Table/Fig-7]. Foveolitis, though inflammation of the fovea, is self limited. Since there are no proven effects of steroids or anti-inflammatory drugs, we opted for observation. She was followed up every week and showed signs of recovery spontaneously over the next 20 days, without specific treatment, Unaided visual acuity improved to 20/20p in the left eye but with a relentless central scotoma. OCT was repeated on the 21st day and showed normal foveal contour; however had thinning [Table/Fig-8].
Fundus of the right eye, in patient 2: demonstrating hyperemic disc and a few blot haemorrhages temporal to the disc, rest of the fundus is unremarkable.
Fundus of the left eye, in patient 2: hyperaemic disc, subretinal discrete yellow lesions in the macula, with interspersed splinter haemorrhages. The fovea has a well circumscribed yellow lesion surrounded by striations.
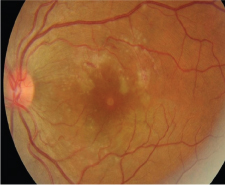
Optical coherence tomography, macular thickness profile (patient 2) showing normal foveal curvature in the right eye (above insert) with a normal central subfield thickness (258μm) whereas left eye has distorted foveal contour, cystoid spaces in the inner retinal layers and an elevated hyper reflective lesion arising from the inner segment-outer segment junction entering the outer nuclear zone consistent with foveolitis. Macular thickening noted at fovea and superonasal to fovea.
Optical coherence tomography (patient 2) of left eye demonstrating a macular thickness change analysis from before (above insert) with foveolitis to a thinned foveola after 20 days of observation. (below insert)
Discussion
In recent years, dengue has become a major public health concern. Its global prevalence has increased tremendously in recent decades, being endemic in more than 100 countries, especially in Southeast Asia, which continues to show a dramatic rise [1].
Dengue fever is known to manifest myriad of complications that encompass the spectrum of life threatening to self-limiting conditions. Worth noting is the ubiquitous nature of the dengue virus and its expanding clinical profile, which is constantly unravelling; resulting in these unconventional manifestations being accounted for more commonly these days. Ocular complications of dengue are rare, but not unheard of [2]. The dengue virus which has the propensity to kill; can sometimes cause blindness. Our patients are a living testimony of this vector-borne virus’ ability to affect vision. In view of the rarity and crippling nature of one such complication- dengue associated maculopathy, we reported two such cases, complicating classical dengue fever, which coincided with the nadir of thrombocytopenia and resolved spontaneously without treatment.
The purview of ophthalmic associations of dengue, encompass a plethora of manifestations- including anterior chamber and vitreous inflammatory cells, intraretinal and peripapillary haemorrhages, Roth’s spots, intraretinal lesions, maculopathy with diffuse oedema, vasculitis, blurring of the optic disc margins. Persistent visual impairment has also been demonstrated, secondary to maculopathy and optic neuropathy [2-4]. Other manifestations include papillodema secondary to cerebral veinous thrombosis, retinal artery occlusion, subhyaloid haemorrhage, bilateral vitreous haemorrhage, bilateral choroidal effusion, optic neuropathy, choroidal neovascularisation secondary to immune damage, and even panophthalmitis [5].
Borne by the female mosquito Aedes aegypti, dengue is caused by an arbovirus, which belongs to the flaviviridae family. There are four serotypes of flaviviridiae viruses that are closely-related but antigenically distinct which do not confer cross-immunity: DEN-1, 2, 3 and 4. After infection with one serotype, individuals are not protected from the other serotypes. Worldwide cases of illness exceed 100 million per year [6,7].
Data on DAM in literature is limited, and its exact prevalence is unknown. OCT is an indispensable tool for monitoring and prognostication of visual defects in DAM. Three OCT patterns of maculopathy have been described: diffuse retinal thickening, cystoid macular oedema and foveolitis [8].
Prognosis for dengue associated maculopathy is variable. Visual recovery is usually good. Spontaneous recovery of DAM has been previously reported [9]. In some cases, visual recovery may be prolonged or scotomata may persist even at two years [10].
The pathogenesis of ocular involvement has not been conclusive yet, although an immune mediated mechanism has been postulated [3]. The vast spectrum of manifestations of dengue fever suggests that several pathophysiologic mechanisms may be involved. Low serum complement three levels have been found to be significantly associated with the presence of dengue maculopathy [11].
The six-seven day delay in the onset of visual symptoms from the acute viral infection corresponds to the time of onset of antibody production or immune complex deposition. Occurrence of ophthalmic manifestations in the convalescent stage of the infection points to its immune mediated mechanism, rather than direct invasion or infection by the virus [3]. It is uncertain whether DAM is associated with the production of autoantibodies against retina, Retinal Pigment Epithelium (RPE) or choroidal antigens [12].
A similar case report has been reported in Malaysia, where one eye with macular oedema showed improvement of visual acuity whereas the other eye with foveolitis had no improvement of visual acuity [13]. Thus, foveoilitis may point to a slower recovery, as evidenced by the second patient in our report. A Singaporean retrospective study, however reported visual improvement with corticosteroids and immunosuppressives in dengue maculopathy. A conclusion whether the visual recovery was due to therapy or due to the nature of the disease was not clearly made [14].
Conclusion
Dengue has various ophthalmic manifestations. This article describes two cases of self-limited dengue associated maculopathy with two different patterns as seen on OCT. In the patient with macular oedema, oedema fully resolved so did the central scotoma, however the foveola showed thinning and a positive scotoma remained in the patient with foveolitis, suggestive of a probable exaggerated response to dengue antigens.
[1]. Dengue and severe dengue - Fact sheet. Accessed from: http://www.who.int/mediacentre/factsheets/fs117/en/. Updated July 2016. Last accessed on 21/3/2017 [Google Scholar]
[2]. Siqueira RC, Vitral NP, Campos WR, Orefice F, de Moraes Figueiredo LT, Ocular manifestations in dengue feverOcul Immunol Inflamm 2004 12:323-27. [Google Scholar]
[3]. Lim WK, Mathur R, Koh A, Yeoh R, Chee SP, Ocular manifestations of dengue feverOphthalmology 2004 111:2057-64. [Google Scholar]
[4]. Haritoglou C, Dotse SD, Rudolph G, Stephan CM, Thurau SR, Klauss V, A tourist with dengue fever and visual lossLancet 2002 360:1070 [Google Scholar]
[5]. Moreker SR, Dengue eye diseaseBMJ 2015 351:h4661 [Google Scholar]
[6]. Halstead SB, Global epidemiology of dengue haemorrhagic feverSoutheast Asian J Trop Med Public Health 1990 21:636 [Google Scholar]
[7]. Halstead SB, Mosquito-borne haemorrhagic fevers of South and South-east AsiaBull World Health Organ 1966 35:3 [Google Scholar]
[8]. Teoh SC, Chee CK, Laude A, Goh KY, Barkham T, Ang BS, Eye Institute Dengue-related Ophthalmic Complications Workgroup. Optical coherence tomography patterns as predictors of visual outcome in dengue-related maculopathyRetina 2010 30:390-98. [Google Scholar]
[9]. Loh BK, Bacsal K, Chee SP, Cheng BC, Wong D, Foveolitis associated with dengue fever: a case seriesOphthalmologica 2008 222:317-20. [Google Scholar]
[10]. Lai TY, Mohamed S, Chan WM, Lai RY, Lam DS, Multifocal electroretinography in dengue fever-associated maculopathyBr J Ophthalmol 2007 91:1084-85. [Google Scholar]
[11]. Su DH, Bacsal K, Chee SP, Flores JV, Lim WK, Cheng BC, Prevalence of dengue maculopathy in patients hospitalized for dengue feverOphthalmology 2007 114(9):1743-47. [Google Scholar]
[12]. Lin CF, Lei HY, Shiau AL, Liu CC, Liu HS, Yeh TM, Antibodies from dengue patient sera cross-react with endothelial cells and induce damageJ Med Virol 2003 69:82-90. [Google Scholar]
[13]. Juanarita J, Raja Azmi MN, Azhany Y, Liza-Sharmini AT, Dengue related maculopathy and foveolitisAsian Pac J Trop Biomed 2012 2(9):755-56. [Google Scholar]
[14]. Bacsal KE, Chee SP, Cheng C, Dengue associated maculoapthyArch Ophthalmol 2007 125(4):501-10. [Google Scholar]