Right Pulmonary Venous Atresia: A Rare Cause for Recurrent Unilateral Pneumonia
Prashant P. Patil1
1 Consultant, Department of Paediatric Cardiology, Lotus Children Hospital, Hyderabad, Telangana, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Prashant P. Patil, Flat No G 901, Jade Block Rainbow Vista @ Rock Garden, Green Hills Road, Opp IDL Factory Compound, Moosapet, Hyderabad-500072, Telangana, India.
E-mail: drprashant 1981@gmail.com
Recurrent unilateral pneumonia poses a diagnostic dilemma for all paediatricians. Isolated pulmonary venous atresia is an uncommon entity, which presents with recurrent unilateral pulmonary infections, dyspnoea on exertion and haemoptysis. It is associated with significant mortality and morbidity. Owing to rarity of condition, there may be some difficulties in the diagnosis and therapy. Pulmonary angiography is the investigation of choice. However, the current multislice CT scanners may obviate the need for pulmonary angiography. We report a two-year-old child with this rare congenital malformation and discuss diagnostic modalities and management options.
Congenital, Multislice CT scan, Pulmonary angiography, Pulmonary vein
Case Report
A two-year-old girl child, weighing 6.8 kg presented at the outpatient clinic for severe failure to thrive and history of recurrent lower respiratory tract infection since early infancy. She was born to non-consanguineous marriage with no significant antenatal history. Her birth weight was 2.9kg. She required hospitalization thrice over last one year due to right sided pneumonia without relief of symptoms. In view of tuberculosis contact, she was treated for pulmonary kochs for six months.
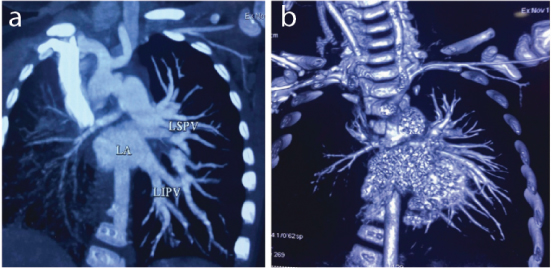
On physical examination, the child had severe respiratory distress with room air saturation of 94%. On respiratory system examination, she had decreased air entry on right side with crackles. Cardiovascular examination revealed cardiomegaly with right ventricular predominance. On auscultation, there was no murmur with loud second heart suggestive of pulmonary hypertension. Chest radiograph revealed small right hemithorax with increased opacity throughout the right lung and rightward shift of trachea and mediastinum due to reduced volume of the right lung. Also it revealed kyphoscoliosis with cardiomegaly with Cardio Thoracic (CT) ratio of 0.65 [Table/Fig-1]. Transthoracic Doppler echocardiographic examination revealed dilated right heart with severe tricuspid regurgitation. Estimated systolic pulmonary pressure was 88 mm Hg. Interventricular septum was intact with paradoxical motion. Right pulmonary artery was hypoplastic with normal sized left pulmonary artery. The right pulmonary veins could not be visualized with normal left pulmonary venous drainage. A 124 slice Computed Tomography (CT) pulmonary angiography revealed hypoplastic right pulmonary artery with absent pulmonary veins on right side. Right lung was hypoplastic with interlobar fissure thickening. Left pulmonary artery had a normal caliber with pulmonary venous drainage to left atrium [Table/Fig-2 a,b]. So, diagnosis of right pulmonary venous atresia was confirmed. A cardiothoracic surgeon opinion was taken, who advised for right pneumonectomy but parents refused to undergo the procedure. She was started on diuretics and digoxin and asked to follow up regularly. On follow up after one year, patient continued to be symptomatic with severe pulmonary hypertension.
Chest radiograph shows small right hemithorax with increased opacity throughout the right lung and rightward shift of trachea and mediastinum. Also it reveals kyphoscoliosis with cardiomegaly.

Coronal Maximum Intensity Projection (MIP) CT angiography images depict complete absence of the right-sided pulmonary veins.
Discussion
Pulmonary venous atresia is a rare condition, which is associated with congenital heart defects in around 1/3 of the cases [1,2]. Isolated pulmonary venous atresia is rare, which can be congenital or acquired in origin. Failure of incorporation of the common pulmonary vein into the left atrium is likely the cause of congenital pulmonary vein atresia [3,4]. Acquired pulmonary vein atresia can be seen as complication of intrathoracic surgery, infections and intracardiac tumours/thrombi [5].
In adults, the reported complaint of unilateral pulmonary venous atresia is dyspnoea on exertion and haemoptysis, whereas in infants recurrent pulmonary infections are the basic feature. Dyspnoea on exertion and haemoptysis are the presenting complaint in reported adult cases [1,2,6]. Cyanosis is not expected unless associated with other congenital malformations [5]. Pulmonary hypertension is a frequent association.
On histological examination of pulmonary veins in affected individuals, there is severe medial hypertrophy with intimal fibrosis, causing inadequate gas exchange and ventilation perfusion mismatch [2,6,7]. A 124 slice Computed tomography and magnetic resonance imaging are very helpful diagnostic tools in suspected cases obviating need for cardiac cauterization [8]. Pulmonary artery wedge angiography will help in confirming diagnosis and to see any systemic pulmonary collaterals [2] . The absence or reversal of pulmonary blood flow in the affected lung is strongly suggestive of unilateral pulmonary vein atresia [7,8].
Pulmonary venous atresia carries a grave prognosis in infant due to its rarity and difficult diagnoses. If left untreated, mortality rate is reported to be as high as 50% [5]. As there are very few cases reported, follow up in many cases were missing. We followed up the indexed case for one year but later patient was lost to follow up.
The treatment of unilateral pulmonary vein atresia is challenging and controversial. On the basis of current evidence, three therapeutic approaches are available. The first is conservative approach for those, who do not have significant symptoms and pulmonary hypertension. The second option is pneumonectomy, for patients with symptoms such as recurrent pulmonary infection, significant haemoptysis or pulmonary hypertension. Available evidence indicates that the outcome of pulmonary resection is satisfactory [2,5,9]. The third approach is reparative surgery. Experience with reparative surgery is very limited and reported outcome with this type of surgery is not good [5]. However, when this condition is detected early in life, before irreversible changes develop in pulmonary tissue and circulation, this approach can be considered [5,6].
In present case, patient was advised for right pneumonectomy, due to symptoms and pulmonary hypertension but patient refused to undergo any surgery. Patient had recurrent right sided lung infection with loss of lung volume and nodular opacities on x-ray, so previously were treated for pulmonary kochs. Detailed cardiovascular examination, cardiomegaly on x-ray with small lung volume was pointer towards cardiac cause. So, it is advisable to get echocardiography done in suspected cases. A 124 slice CT scan/magnetic resonance tomography can assist in concluding diagnosis.
Conclusion
Pulmonary venous atresia is a rare condition which is usually associated with congenital heart defects. Isolated venous atresia is very rare. A high index of suspicion in recurrent pneumonia coupled with appropriate diagnostic modalities will help in the early diagnosis and treatment. Newer non-invasive modalities such as 124 slice CT scan/MRI angiography are replacing invasive investigation such as cardiac catheterization for diagnosis of pulmonary venous atresia.
[1]. Heyneman LE, Nolan RL, Harrison JK, McAdoms HP, Congenital unilateral pulmonary vein atresia- radiologic findings in three adult patientsAJR Am Roentgenol 2001 177(3):681-85. [Google Scholar]
[2]. Pourmoghadam KK, Moore JW, Khan M, Madan N, Wolfson BJ, De Chadarevian JP, Congenital unilateral pulmonary venous atresia: definitive diagnosis and treatmentPaediatr Cardiol 2003 24(1):73-79. [Google Scholar]
[3]. Reller MD, McDonald RW, Gerlis LM, Thornburg KL, Cardiac embryology: basic review and clinical correlationsJ Am Soc Echocardiogr 1991 4(5):519-32. [Google Scholar]
[4]. Tissot C, Corbelli R, Aggoun Y, Beghetti M, Da Cruz E, Bronchoscopic diagnosis of asymptomatic unilateral pulmonary vein atresia in an infantPaediatr Cardiol 2008 29(5):976-79. [Google Scholar]
[5]. Shimazaki Y, Nakano S, Kato H, Ohtake S, Ikawa S, Miura T, Mixed type of total anomalous pulmonary venous connection with hemi-pulmonary vein atresiaAnn Thorac Surg 1993 56(6):1399-401. [Google Scholar]
[6]. Argueta-Morales IR, Garg R, DeCampli WM, Diagnosis and management of congenital right pulmonary venous atresiaCardiol Young 2009 19:648-51. [Google Scholar]
[7]. Dixit R, Kumar J, Chowdhury V, Case report: Isolated unilateral pulmonary vein atresia diagnosed on 128-slice multidetector CTIndian Journal of Radiology and Imaging 2011 21(4):253-56. [Google Scholar]
[8]. DeMastes-Crabtree CS, Kim E, Morton RL, Unilateral pulmonary vein atresia: A rare case of haemoptysis.. Unilateral pulmonary vein atresia: A rare case of haemoptysisRespiratory Medicine Case Reports 2015 15:83-84. [Google Scholar]
[9]. Narayanan R, Shankar B, Paruthikunnan S, Isolated unilateral pulmonary vein atresiaLung India 2016 33(5):571-72. [Google Scholar]