A bezoar refers to a mass of undigestible foreign material found in the gastrointestinal tract, mainly stomach. The second most common bezoar is the trichobezoar, which usually occurs in the young psychiatric female patients with history of trichotillomania and trichophagia. This is a case report of a 12 -year-old female patient came with complaints of diffuse abdominal pain, vomiting, and constipation. Ultrasound, Barium X-ray and Computed Tomography scan were done, which suggested trichobezoar. Thus, trichobezoar should be considered as differential diagnosis of abdominal pain in young female patients with associated psychiatric complaints. A review is presented here, as a high index of suspicion for better diagnostic facilities which can help in timely diagnosis and intervention, to prevent further complications like intestinal obstruction, perforation and mortality in such children.
Abdominal mass, Mental retardation, Trichobezoar
Case Report
A 12-year-old female presented to the Emergency Department with abdominal pain for 20 days, vomiting for four days and constipation for three days. She also had loss of appetite for two months. She was asthenic, pale and mildly dehydrated. She had no fever, her pulse rate was 100/minute and her blood pressure was 110/70 mmHg. On systemic examination, her cardiac and respiratory systems were normal. Abdominal examination revealed a globular, mobile, well defined mass of size 8 cm × 6 cm in the epigastrium and left hypochondrium. It was firm in consistency and tender on palpation.
Investigations like complete blood count, liver function test, renal function test and serology has been carried out with relevant findings, showing Haemoglobin (Hb) of 8.8 g/dl and peripheral smear shows microcytic normochromic anaemia.
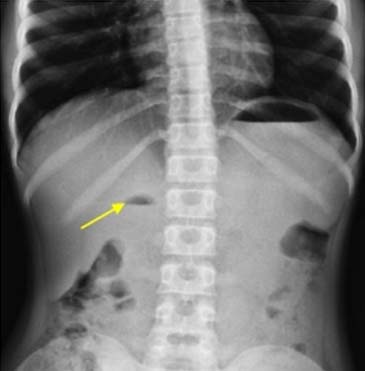
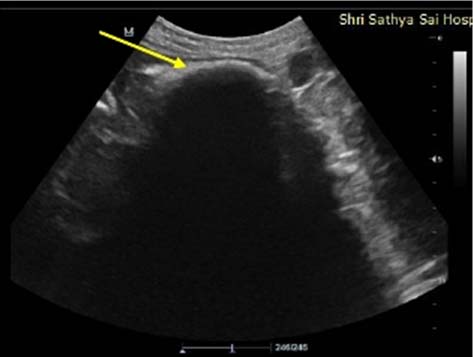
Patient was referred to the Radiology Department to rule out splenic mass. X-ray abdomen showed distended J shaped stomach with air-fluid level in the second part of duodenum [Table/Fig-1]. Ultrasonogram (USG) abdomen shows an echogenic curvilinear mobile shadow in the stomach with dense posterior acoustic shadow [Table/Fig-2].
Plain X-ray – Distended J shaped stomach with air fluid levels at the level of fundus and second part of duodenum.
USG abdomen: Curvilinear echogenic mobile shadow in the stomach with dense posterior acoustic shadow.
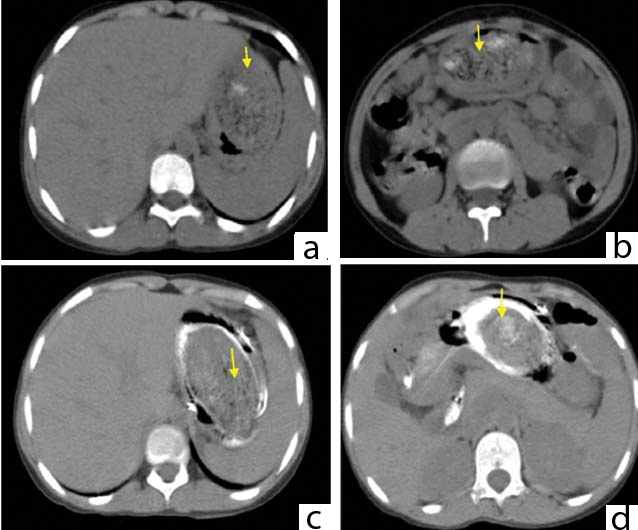
Barium meal follow through shows intraluminal filling defect with mottled gas pattern without attachment to stomach wall [Table/Fig-3a-e]. Computed Tomography (CT) abdomen showed a diffuse intragastric mass extending from the fundus of stomach till the second part of duodenum consisting of “compressed concentric rings” measuring 11 cm x 9.5 cm x 7.9 cm. The lesion appears heterogenous with entrapped air and food debris. The pylorus appears dilated with air-fluid level [Table/Fig-4a,b]. The contrast appears to be coating the lesion except for the most dependent part of the greater curvature [Table/Fig-4c,d].
a) Barium swallow oesophageal phase showing normal oesophagus and gastroesophageal junction; b,c) Supine radiograph follow through shows intraluminal defect with mottled gas pattern without attachment to stomach wall; d) Oblique view showing intralumianl defect; e) Supine view with intraluminal filling defect, contrast seen in duodenum.

a,b) Non contrast CT abdomen at the level of stomach shows a diffuse intragastric mass extending from the fundus of stomach till the second part of the duodenum consisting of “compressed concentric rings”. The lesion appears heterodense with entrapped air and food debris; c,d) Contrast enhanced CT shows contrast coating the lesion.
Other abdominal organs were normal. Based on imaging, she was diagnosed with trichobezoar. After which, the patient was referred to the Psychiatry department where she was diagnosed with low Intelligence Quotient (IQ) and mental retardation. Patient underwent gastrostomy, with retrieval of trichobezoar [Table/Fig-5] without any surgical complications. Postoperatively the patient is on regular psychiatric therapy and endoscopic follow up.
Postoperative specimen of trichobezoar measuring 8 cm x 3 cm x 4 cm with a thin strand of hair extending to the small bowel.

Discussion
Rapunzel syndrome was first described by Vaughan ED et al., [1]. It comes from the Grimm Brothers’ fairy tale of a 12-year-old princess who was shut into a tower with neither stairs nor doors by an enchantress who climbed up the tower’s walls with the help of Rapunzel’s long tresses [2].
In most cases, the trichobezoar is confined within the stomach. If trichobezoar extends through the pylorus into the jejunum, ileum or even colon it is called as Rapunzel syndrome.
People commonly affected by trichobezoars are young women between 13 and 20 years of age with mental retardation or psychiatric illness.
Trichobezoar has a glistening shiny surface due to the mucous covering it [3]. The putrid smell is due to decomposition and fermentation of fats in the interstices [4].
Usually, there are no symptoms until, it reaches substantial size. The most common features are abdominal pain, abdominal mass, gastrointestinal obstruction, weight loss and poor appetite. Complications include ulcers, perforation, peritonitis, intussusceptions, malnutrition, rarely obstructive jaundice, pancreatitis and fatalities [5].
Diagnostic procedures are commonly initiated owing to acute abdominal symptoms. Given the density of hair and mucus, identification on plain radiography can be difficult. Identifying the borders of the stomach, detecting gastric distension, mottled gas pattern, surrounding lucency and multiple air-fluid levels can be helpful in the diagnosis.
Investigations Done
Various radiological investigations are done [6] and findings are tabulated as shown in [Table/Fig-6].
Various radiological investigations and their findings.
| Radiological Investigations | Findings |
|---|
| Plain X-ray | Distended J shaped stomach with air-fluid levels at the level of fundus and second part of duodenum. |
| USG abdomen | Curvilinear echogenic mobile shadow in the stomach with dense posterior acoustic shadow. |
| Barium meal follow through | Intraluminal filling defect with mottled gas pattern without attachment to stomach wall. |
| CT Abdomen | Diffuse intragastric mass extending from the fundus of stomach till the second part of duodenum consisting of “compressed concentric ring”. The lesion appears heterogenous with entrapped air and food debris. The pylorus appears dilated with air-fluid level. |
| CECT Abdomen | Coating the lesion except for the most dependent part of the greater curvature. |
Differential Diagnosis
Pancreatic Pseudocyst – extraluminal smooth filling defect in stomach with no mottled appearance;
Gastrointestinal Stromal Tumours (GIST) – subepithelial mass (obtuse margin) with gastric wall in profile view and smooth circumscribed margin – enface view with mucosal ulceration;
Phytobezoar – intraluminal defect without constant attachment to bowel wall and clinical history.
Small trichobezoars can be removed by endoscopy. Endoscopic removal is difficult and risky, oesophageal perforations may occur. Bezoars can be fragmented or disrupted by various techniques – by biopsy device, water jet under direct vision, bezotome (monopolar diathermy knife with needle) or by using laser ignited mini explosive techniques and enzymatic therapy, before endoscopic removal [5].
Conclusion
The diagnosis of trichobezoar is possible only on imaging. The psychiatric and medical sequel of trichotillomania should not be under estimated, early diagnosis and treatment is really important to save the patient’s life and recurrence. Laparotomy is considered an excellent treatment option. Although, pharmacotherapy and behavioral assessment play a useful role in patient’s management.
[1]. Vaughan ED, Sawyers JL, Scott HW, The Rapunzel syndrome: An unusual complication of intestinal bezoarSurgery 1968 63(2):339-43. [Google Scholar]
[2]. Duke DC, Keeley ML, Geffken GR, Storch EA, Trichotillomania: a current reviewClin Psychol Rev 2010 30(2):181-93. [Google Scholar]
[3]. Sharma V, Sahi RP, Misra NC, Gastro-intestinal bezoarsJ Indian Med Assoc 1991 89(12):338-39. [Google Scholar]
[4]. Sidhu BS, Singh G, Khanna S, TrichobezoarJ Indian Med Assoc 1993 91(4):100-01. [Google Scholar]
[5]. Jeyasingh S, Sundari M, Kannan VV, Trichobezoar—two case reportsTEJMS 2011 2:41-42. [Google Scholar]
[6]. Prajapati NC, Kumar R, Gupta R, Pengoria R, Garg G, Rapunzel syndrome - A case reportJ MGIMS 2012 17(2):43-46. [Google Scholar]