Pesticides are a group of chemicals used worldwide predominantly in agriculture and against vectors of vector-borne diseases such as malaria, filariasis, etc. Farm workers are the population who are mostly exposed to pesticide. India is an agricultural country and also a major consumer and producer of pesticides. It is evident that the pesticides not only provide benefits to mankind in the field of agriculture by increasing the productivity and thereby the economy of the farmers but also produce undesirable and unwanted effects of its usage which cannot be ignored. Farmers are the backbone of the Indian agricultural economy. They face greater threats from pesticide exposure both acutely and chronically [1].
Indiscriminate use and improper handling of synthetic pesticides in agriculture have resulted into serious problems for human health in many developing countries [2]. Exposure to various types of farming occupation is associated with a number of respiratory problems which are both immunologic and non-immunologic in origin [3]. Farmers are at increased risk of development of respiratory symptoms compared to normal population [4,5]. Several earlier studies have reported increased risk of respiratory problems, such as asthma, wheeze and chronic bronchitis among agricultural workers [6,7]. Pesticides after reaching the lungs from the systemic circulation through inhalation and absorption, adversely affect the lung tissues [8]. Both obstructive and restrictive lung dysfunctions are reported in Organophosphorus (OP) poisoning [9].
The primary route by which pesticides enter the body are, accidental ingestion of pesticides mistaken for drink or flour, and through the respiratory tract when farmers enter into sprayed field immediately after spraying to collect firewood or animal feed, skin and eye contact with spray due to a change in wind direction during spraying or through a leaking sprayer [10]. Occupational exposure to pesticides not only affects agricultural workers in open fields but also farm worker households as they live near the farms and spends much of the time in close proximity to areas where pesticides were applied on regular basis [11]. Other family members were exposed to pesticide residues, that come from contaminated shoes, clothes of farm workers and that drift from outdoors when sprayed in the form of aerosols. The risk and severity of pesticide on adverse health effects depend on the type of pesticide, measures taken during application and also on age and health status of the subjects [12].
Lack of Personal Protective Equipment (PPE) like safety masks, gloves etc., during the aerial spraying of pesticides result in the entry of pesticides in the blood stream via respiratory tract through inhalation which can adversely affect respiratory system [8]. After-work hygiene practices, such as leaving work boots outside and changing promptly from work clothes, has also been found to affect pesticide levels in the homes of farm workers [10]. The chemical used are volatile and the finely dispersed drops of aerosol sprays after spraying remain suspended in the air can be inhaled by the workers, producing irritant effect and airway narrowing [13].
We know that cardiovascular system is closely associated with respiratory system in delivering oxygen to the tissues hence we also assess the basic cardiovascular parameters to know the effect of OP compounds on the cardiovascular system. However, there is paucity of data of such reports in rural population of southern India which are at higher risk. Protection of workers against the work related injuries and illnesses are of great importance since many years. Thus, to create awareness among the farmers regarding the ill effects of pesticides and to encourage using personal protective equipment, this study was chosen. Farmers can also be taught about the importance of organic farming, which may benefit not only the farmers but also the general public. Thus, this study was carried out to find the cardiorespiratory changes in farm workers exposed to organophosphorus pesticides.
Materials and Methods
This cross-sectional study was undertaken in CN Palayam, Naduveerpattu village of Cuddalore district, Tamil Nadu, India from March to May in the year 2014. A total of 35 farm workers were recruited by simple random sampling method based on the inclusion and exclusion criteria and 35 non farm workers were taken as controls. A total of 23 farmers and 26 non-farm workers belong to the age group between 20-40 years of age were recruited. Twelve farmers and 9 non-farm workers fall in the age group between 40-60 years. Among the 35 farmers, 11 were males and 24 were females. Among the 35 non-farmers, 16 were males and 19 were females. The control group does not belong to farming community but were involved in pottery selling business. All 35 farmers and 35 non farmers who entered the study were accounted.
The following formula was used for sample size calculation:
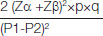
Where p, P1=56%(prevalence of respiratory disease among the farm workers) [14]:
q= 100-p
P2=20%
Zα=1.96
Zβ=0.842 for sample size calculation.
The minimum sample size required was coming around 28 and by adding 10% of failure rate it was coming around 31 so we have took 35 as sample size.
Inclusion criteria: Farm workers of both the sex who work six hours a day (average hours of working in the field per day) for atleast six days a week, age group 20-60 years.
Inclusion criteria for controls was non-farm workers of same age group and not exposed to organophosphorus compounds.
Exclusion criteria: Smokers, known asthmatic, hypertensives and cardiac patients, those who were on regular medications for any medical illnesses, < 6 months of exposure to OP compounds.
After getting the Institutional Ethical Committee clearance, subjects were recruited based on inclusion and exclusion criteria. Informed consent was obtained from all the subjects. Detailed medical history mainly the respiratory symptoms, duration of exposure, use of protective equipments if any (face mask, gloves, eye mask, special clothes, shoes and hat) and cleanliness habits (taking food in between the work without washing the hands, taking bath after working in the field) were noted from the study group. Measurements like height, weight, blood pressure, pulse rate, BMI, PEFR were recorded during 10 am-12 am in the morning for both study and the control group.
PEFR was measured using Wright’s mini Peak Flow Meter [15]. PEFR was measured by asking the subjects to sit comfortably and expire forcefully in to the peak flow meter after making deep inspiration to find the maximum velocity of airflow. The procedure was repeated three times and the maximum of the three readings were taken.
Statistical Analysis
Chi-square test was used to analyse the qualitative data. All values were expressed as Mean±SD. Students unpaired t-test was used to compare PEFR between two groups and to compare the duration of exposure and PEFR using GRAPH PAD PRISM. The p<0.05 was considered to be statistically significant.
Results
From [Table/Fig-1] it is seen that the study and the control group were age and BMI matched. Pulse rate and PEFR show a significant difference between study and the control group.
Cardiorespiratory parameters among the study and the control group.
| Parameters | Study group | Controls | p-value |
|---|
| Age (years) | 38.54±5.135 | 35.17±11.76 | 0.1247 |
| BMI (kg/m2) | 22.66±1.919 | 23.39±1.958 | 0.1177 |
| SBP (mm of Hg) | 121.1±7.329 | 117.1±9.778 | 0.0536 |
| DBP (mm of Hg) | 81.49±6.237 | 81.09±6.622 | 0.7955 |
| Pulse (beats/min) | 70.31±6.457 | 77.49±6.762 | <0.001* |
| PEFR (L/min) | 340.9±68.44 | 405.6±65.90 | <0.001* |
BMI- body mass index, SBP- systolic blood pressure, DBP- diastolic blood pressure, PEFR- peak expiratory flow rate. p< 0.001 –statistically significant*
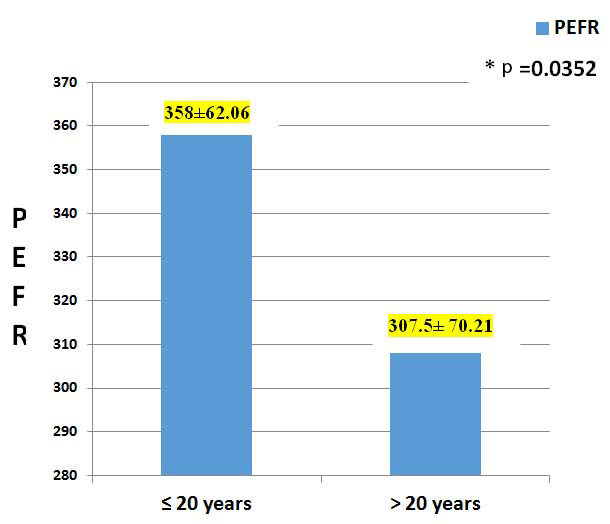
From [Table/Fig-2] it is clearly seen that there was a significant difference (p<0.05) in PEFR between the farmers who worked for ≤ 20 years (n=23) and those who worked > 20 years (n=12)
Relation between duration of exposure and PEFR among the farmers.
The Chi-square test between respiratory symptoms (cough, chest tightness, breathing difficulty) and duration of exposure did not show any significant difference among the farmers. As a whole 71% of the farm workers used one or more personal protective equipments. Among the 35 farm workers 65% used special clothes for working in the field, 31% used special gloves while working with the pesticides, 20% used face mask when they work in the pesticide sprayed field, 14% used special shoes when they work in the freshly pesticide sprayed field and 5% covered their head with cloth while working in the freshly sprayed field. About 22% of farmers had cough and breathing difficulty, 20% had chest tightness. Nearly 14% were taking food in between the work without washing the hands, 71% had the habit of taking bath after working in the field.
Discussion
There was a significant decrease in PEFR among the farmers when compared to the control group. This is similar to the results obtained by Jinky Leilanie Del Prado-Lu, and Chakraborty S et al., [16,17]. The PEFR seemed to have an inverse relation with the duration of exposure to pesticides. This could be due to entry of pesticides via inhalation and orally because of various unhealthy practices like not washing the hands immediately after work in the field [3,8]. Turabi A et al., also reported that farmers with mild pesticide poisoning fail to report to the health sector because of the fear of losing employment if they were found to have the disease. He also reported that chronic pesticide exposure was a problem among the poor rural population where they live and work in close proximity to the fields on which the chemicals were applied. He further emphasized that use of empty cans of pesticide as drinking water reservoir and bad hygiene were the expected sources of exposure [2].
Though pesticides can get access into the human body by various routes, it can enter more quickly via the respiratory tract causing impairement of lung function. Thus exposure of pesticides through inhalation among the farmers deserves particular attention [18]. Peiris-John RJ et al., further reported that absorption of pesticide is rapid via inhalation and most of the OP compounds directly enter the systemic circulation by passing the liver where they get metabolized [19].
Jinky Leilanie Del Prado-Lu, Chakraborty S et al., and Kesava-chandran C et al., reported that in developing countries like India, farmers get direct exposure to pesticides due to unsafe work practices like improper handling like spraying against the wind, wiping the sweat off the face, incorrect storage and poor housekeeping of the pesticides [16,17,20]. Chitra GA et al., further emphasized that the farmers had very poor knowledge about the ill effects of pesticides and the importance of personal protective equipments [21].
Volatile chemicals after spraying remain suspended in the air can be inhaled by the workers, producing irritant effect and airway narrowing [6]. This shows that the organophosphorus compounds trigger the bronchospasm and increase the airflow resistance among the agricultural farm workers [22]. These small droplets can also have an access to alveolar space and damage the alveolar capillary membrane and subsequently the diffusion of gases. Our findings are further supported by Eskenazi B et al., that OP pesticides cause respiratory diseases among the children through dysregulation of autonomic nervous system [23].
Reduction in PEFR on chronic exposure to OP compounds could be attributed to irreversibile binding to cholinesterase enzyme and its deactivation [19]. Some authors also reported that effect of OP compounds could also be due to the production of oxygen free radicals [24]. Fareed M et al., found that the cholinesterases levels decrease as the respiratory symptoms among the farmers increase [8]. In contrast Cotton J et al., reported that Erythrocyte Cholinesterase activity (EAChE) was reported as normal for mild to chronic exposure group due to wide reference range for EAChE activity [25]. Various animal studies also reported that vagally mediated broncho-constriction is due to decreased function of inhibitory M2 muscarinic receptors on parasympathetic nerves to the airway smooth muscle [26]. Both acute and subacute exposure of Wister rats to OP compounds increase the muscarinic effect on smooth muscles of the airways and the nicotinic effects on the muscles of respiration along with increase in affinity to acetylcholine (Ach) [27]. Our study was further supported by Kesavachandran C et al., who found that FVC, FEV1, PEFR were lower among the pesticide retailers [28].
Evidence suggests that organophosphorus (OP) compounds being highly volatile affects the dwellers around 25 kms radius from the agricultural field apart from farming community. Hence, control group were selected from urban area which is more than 25 kms from the field [2].
OP compounds are known to cause bradycardia and hypotension [8], but in this study both systolic and diastolic blood pressure did not show any significant difference between the two groups. The cardiovascular effects could be due to entry of pesticides in the blood stream via the respiratory tract or due to increased cholinergic activity in the nerve endings causing prolonged depolarization [29]. However, the pulse rate was decreased among the farmers which might be due to their regular physical activity.
Hoppin JA et al., reported that OP like coumaphos and parathion were associated with allergic asthma and wheeze [30]. Various studies found that respiratory symptoms and the bronchospasm among the farmers could be due to lack of using personal protective equipments like mask, gloves, etc., [10]. About 25% of farmers reported one or more respiratory symptoms compared to that of the controls.
From this study we found that 71% of the farmers were using personal protective equipments, but only 20% were using the face mask which prevents the entry of OP compounds into the respiratory tract. This might be the reason for decrease in PEFR as the duration of exposure increases.
Limitation
Farmers resisted to give their blood samples for analysis to the researcher outside their social setup. Sample size was limited.
Conclusion
Exposure of farm workers to OP pesticides do affect the cardio respiratory system in long run which can be prevented by educating the farmers to use personal protective equipment and following hygienic practices, because safe working environment will promote the physical, mental and social wellbeing of the workers at work places resulting in effective work output.
BMI- body mass index, SBP- systolic blood pressure, DBP- diastolic blood pressure, PEFR- peak expiratory flow rate. p< 0.001 –statistically significant*