Making Nutrition Management Scientific, Objective and Simple with the Help of Technology
Sanjith Saseedharan1, Edwin Joseph Pathrose2
1 Head, Department of Intensive Care Unit, S.L. Raheja Hospital (A Fortis Associate), Mumbai, Maharashtra, India.
2 Registrar, Department of Intensive Care Unit, S.L. Raheja Hospital (A Fortis Associate), Mumbai, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sanjith Saseedharan, Head, Department of Intensive Care Unit, S.L. Raheja Hospital (A Fortis Associate), Raheja Rugnalaya Marg, Mahim West, Mumbai-400016, Maharashtra, India.
E-mail: sanjith@rahejahospital.com
Nutrition management is one of the cornerstones of care in the management of hospitalized patients, especially, for those who are critically ill. Significant numbers of hospitalized patients have alteration in appetite and the function of the gastrointestinal tract. Calculating the caloric goal, prescribed proteins to be delivered in a finite amount of water at a certain rate is the need of the hour and it becomes a daunting task to complete daily. With the help of technology such tasks can be completed easily and accurately. This suggestion based software called as “iNutriMon” helps to screen out the patients which are at risk of malnutrition, formulate a plan, monitor and manage enteral nutrition of patients by calculating calories, proteins and water intake as per the patient requirement.
Critical care, Dietitian, Enteral, Feeds
Introduction
Nutrition forms an important component of every individual’s lifestyle pattern. It becomes even more significant in a hospitalized individual as they have history of reduced appetite from days to weeks prior to hospitalization and also as it forms an integral part of the treatment regime. Studies have revealed that underfeeding occurs in up to 30% of hospitalized patient and as many as 50% of ICU patients [1,2]. This malnutrition leads to increase length of intensive care unit stay, hospital stay and increased rate of infections thus increasing morbidity. Hence, optimization of nutritional support is very crucial [3-7]. Enteral Nutrition (EN) is clearly the feeding of choice when it comes to providing nutrition to hospitalized patients [8,9]. A number of countries (especially developing) around the world are still using blenderized kitchen diet rather than commercial feeding formulae. The evidences of superiority and safety of commercial feeding formulae (with defined composition) over blenderized kitchen feeds are clearly emerging especially in the critical care units [10,11,12]. Such form of enteral feeding could be either bolus or continuous. Based on expert consensus, American Society of Parenteral and Enteral Nutrition suggested that for high-risk patients or those shown to be intolerant to bolus gastric EN, delivery of EN should be switched to continuous infusion [13-15]. Use of continuous feeding will not be possible with kitchen based feeds as these cannot be hung for more than two hours due to concerns over food safety and bacterial contamination [16,17].
Current nutrition practice: The present flow of nutrition care in majority hospitals involves a dietitian or physician estimating the calorie and protein requirements based on the body weight by simple predictive equations. Very few units around the world use formulae like the Harris benedict equation and fewer utilize indirect calorimetry for the estimation of calorie and protein requirement [18]. If calculated by the simple predictive equations the value is further multiplied by a stress factor which is dependent on the patient’s condition [19]. (However, the evidence for use of stress factors is not very robust and many units across do not utilize stress factors in the calculation). After assigning the caloric and the protein goals the next task would be to prescribe a finite number of scoops of the commercially available feeding formula in a finite amount of water as prescribed by the doctor and then run it at a rate prescribed and safe for the patient. More often multiple preparations need to be mixed to get the actual number of calories and proteins in the prescribed amount of water. However, each commercial feeding formula has defined amount of water in which the powder needs to be reconstituted failing which the feed consistency may change markedly causing problems. Hence, this task of defining the number of scoops, from different commercial feeding powders with prescribed and recommended amount of water to be delivered at a certain rate, becomes difficult. Moreover, it is known that when the powder is mixed with water the actual volume of the finished product is likely to be 10%-20% more than what was used in the preparation. This, in a critically ill patient, is extremely important as these patients require a right balance of fluids and these changes if overlooked can lead to fluid and electrolyte imbalance. It is also important to tightly control the electrolytes namely sodium and potassium in the feeding formulae. According to the American Society for Parenteral and Enteral Nutrition (ASPEN) guidelines, the protein requirement in a critically ill adult patient is in the range of 1.2–2.0 gm/kg/day or the presumptive non-protein calories to nitrogen ratio (NPC:N ratio) is about 70:1 to 100:1 [15]. The current common standard enteral formulas have a high NPC:N ratio. Therefore, additional protein supplements may be required to provide an adequate amount of protein. However, this calculation is rarely done in the diet prescription and hence alarming levels may get unnoticed by the person prescribing the doses. The reconstituted powder feed is discarded within six hours (hang time) of preparation as per industry specifications. Hence, it is advisable that the 24 hour feeding schedule is further broken down to four feeding schedules throughout the day of six hours each. Hence, automatically the feed should finish in six hours and the bags should be refilled with the new feed. Prescribing this kind of routine is definitely time consuming for the dietitian and the physician.
Once the feed has been started there is likely to be a number of interruptions owing to procedures the patient is subjected to, visits to the scanners, operation theatre visits etc. Every time this happens, it leads to non delivery of the feeds leading to some amount being left behind in the bag. This involves loss of a defined amount of proteins, calories and water. Calculation of this deficit becomes difficult especially in the event that multiple feeds are involved. If this deficit is not replaced this leads to cumulative deficits day after day and at the end leads to massive protein and caloric deficits over a number of days which ultimately is linked to prolonged length of stay, increased infection risk etc.
Analysis of data for further improvement of practices is difficult. The evidence in parenteral nutrition supplementation is also getting stronger and hence, more and more intensive care units are supplementing parenteral nutrition if not given totally.
At such times, dose calculation when combining with enteral becomes a difficult task as many dietitians are not very much aware of parenteral nutrition. Needless to say, often both over nutrition and under nutrition are seen in the hospitals. So from the above discussion it becomes obvious that in order to provide nutrition in a scientific evidenced based form, we need to be either superiorly fast and brilliant or we should resort to some kind of help.
The above mentioned problems are seen in many Indian hospitals. This problem was also faced by the author in his institution. Over a period of six months, a new software called iNutriMon [20] was developed and an attempt to address all the above points was made.
How use of software helps: iNutriMon is a web based app that allows doctors/dietitians/nurses to manage the enteral nutrition of patients by calculating calories, proteins and water intake as per the patient requirement and suggesting the optimal feeding programme [Table/Fig-1].

Some examples of the use of the use of iNutriMon: Patient X, 60 kg, known case of ischemic heart disease presents to the hospital with pulmonary oedema. This patient also needs haemodialysis for a failing kidney. In this stage, the patient requires calories of 1500 kcal and around 90 grams of protein as per predictive equations. The clinicians now decide to have fluid restriction to 800 ml in view of the heart failure.
At this stage, it becomes tedious to calculate the commercial feeding formula in the prescribed quantity of water as kitchen feeds would not be able to supplement the requirements.
The software would easily and quickly give us the right amount of scoops in the right amount of water to match the requirements.
Example number 2: Patient Y was receiving 1500 kcal in form of 7 scoops of formula in 400 ml of water at the rate of 60 ml/hour. His feeding was stopped for one hour since he had to go for a CT scan. At this stage it is difficult to calculate the deficit of feeding that has taken place.
With the iNutriMon the nurse/doctor just needs to stop the feeding in real time on the software and restart the feed at a later time when decided. The deficit (of calories, proteins and water) in this case would automatically be calculated and displayed on screen in graphical analysis.
Presently, there is no monitor of this nature in India or any part of world has developed, which comprehensively deals with nutritional support and delivery as the one shown, especially in powder formulae food as the apps on Google play are more towards Liquid based– premixed formulae food. The salient features of this software that makes nutrition prescription and management scientific and simple are enumerated below.
Helps in calculating, suggesting and monitoring total calorie and protein delivered after certain duration of feeding by adjusting the feeding rate or calorie density of the feed to catch up if required.
Helps in calculating, suggesting and monitoring total protein delivered along with calories which enable to include an additional form of nutritional supplement if required.
Helps in calculating, suggesting and monitoring the fluid intake.
Helps in deciding the number of scoops of a particular formula depending upon the calorie and protein requirement.
Helps in monitoring the reason for stopping the feed in the nurses nutrition monitor sheet thus, helping in planning more efficiently thereby delivering at the optimum level.
Assists in using the prevailing guidelines in enteral nutritional support thus translate evidence to practice.
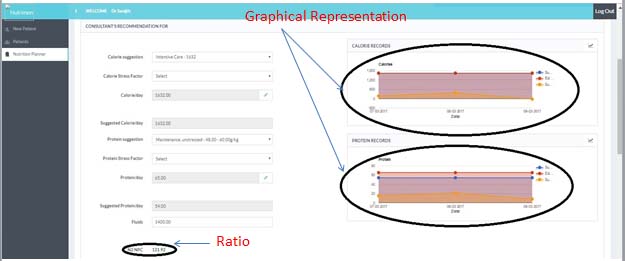
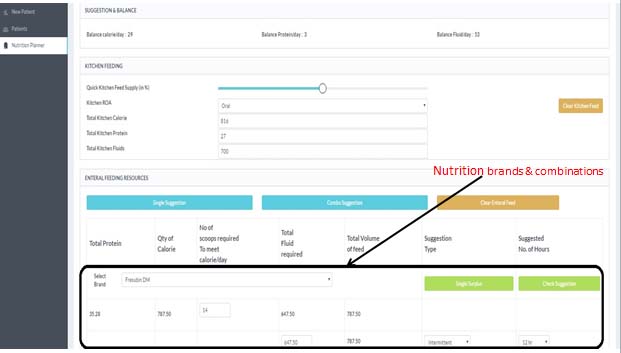
In the planning phase for the dietary prescription the monitor assists the physician/dietitian in the following [Table/Fig-2,3].
Graphical representation and NPC:N ratio.
Nutrition brands and combinations.
- Calculate Height, Ideal Weight and Adjusted Weight
- Calculate BMI, Select Stress Levels of Patient
- Check NPC: N ratio
- Suggests Calorie and Protein Required
- Suggests Nutrition Brands and Combinations
- Suggests Scoops and Water Intake
- Plan Intermittent or Continuous feed
- All suggestions can be edited based on Doctor’s/ Nutritionists’ acumen
In the management phase the nurse physically enters the parameters (like a flow chart). These parameters are then assessed and thus the software has the following capabilities:
- Numerical value for total calorie and protein delivered is shown;
- Reason for stopping feed by nurses is noted;
- Prompts regarding adjustment of feeding rate or calorie density of feed to catch -up if required;
- Add previous deductions or suggest new planner
- Check graphs for calorie and protein record of each patient;
- Records a library of every patient’s planners;
- Gives visual cue of caloric and protein debts by graphs;
- Solves the disparity between the feed prescribed to feed actually delivered.
Software of this kind is an excellent research tool to conduct various studies in view of large retrievable database and graphical representation.
As a result of application of this software in the intensive care unit, several practical benefits were observed by the author. Several studies have been initiated and are in the data collection phase which will prove the efficacy of use of this software. The benefits are enumerated below:
Enables better time management and reduces number of working hours in feeding calculations;
Nurses are better aware of the quantity and quality of the enteral/parenteral solution to be prepared;
Enables a simpler flow rate;
Water can be adjusted in the solution accordingly;
Pivotal scientific values like BMI, Nitrogen-Protein calorie intake can be calculated effectively;
Helps in giving information on the catch up nutrients if required (real time);
Gets objectivity in delivering nutrition to patients;
Imparts physician satisfaction on the nutrition prescription.
Conclusion
In this era of evidence based medicine, it is very important to be extremely scientific and objective in every aspect of care in hospitalized patients. Nutrition plays an important role in the management of these patients.
Utilization of technology in the form of software (like the one described and used in the author’s institute) seems to be a good way to improve the way nutrition is managed, the ultimate goal being to make nutrition therapies scientific, safe and simple.
[1]. Lazarus C, Hamlyn J, Prevalence and documentation of malnutrition in hospitals: a case study in a large private hospital settingNutr Diet 2005 62(1):41-47. [Google Scholar]
[2]. Pirlich M, Schütz T, Kemps M, Luhman N, Minko N, Lübke HJ, Social risk factors for hospital malnutritionNutrition 2005 21(3):295-300. [Google Scholar]
[3]. Caccialanza R, Klersy C, Cereda E, Cameletti B, Bonoldi A, Bonardi C, Nutritional parameters associated with prolonged hospital stay among ambulatory adult patientsCMAJ 2010 182(17):1843-49. [Google Scholar]
[4]. Isabel M, Correia TD, Waitzberg D, The impact of malnutrition on morbidity, mortality, length of hospital stay and costs evaluated through a multivariate model analysisClinNutr 2003 22(3):235-39. [Google Scholar]
[5]. Banks M, Bauer J, Graves N, Ash S, Malnutrition and pressure ulcer risk in adults in Australian health care facilitiesNutrition 2010 26(9):896-901. [Google Scholar]
[6]. Shahin ES, Meijers JM, Schols JM, Tannen A, Halfens RJ, Dassen T, The relationship between malnutrition parameters and pressure ulcers in hospitals and nursing homesNutrition 2010 26(9):886-89. [Google Scholar]
[7]. Faisy C, Lerolle N, Dachraoui F, Savard JF, Abboud I, Tadie JM, Impact of energy deficit calculated by a predictive method on outcome in medical patients requiring prolonged acute mechanical ventilationBr J Nutr 2009 101(7):1079 [Google Scholar]
[8]. Heyland DK, Dhaliwal R, Drover JW, Gramlich L, Dodek P, Canadian Critical Care Clinical Practice Guidelines Committee. Canadian clinical practice guidelines for nutrition support in mechanically ventilated, critically ill adult patientsJPEN J Parenter Enteral Nutr 2003 27(5):355-73. [Google Scholar]
[9]. Gramlich L, Kichian K, Pinilla J, Rodych NJ, Dhaliwal R, Heyland DK, Does enteral nutrition compared to parenteral nutrition result in better outcomes in critically ill adult patients? A systematic review of the literatureNutrition 2004 20(10):843-48. [Google Scholar]
[10]. Sullivan MM, Sorreda-Esguerra P, Platon MB, Castro CG, Chou NR, Shott S, Nutritional analysis of blenderized enteral diets in the PhilippinesAsia Pac J Clin Nutr 2004 13(4):385-90. [Google Scholar]
[11]. Jalali M, Sabzghabaee AM, Badri SS, Soltani HA, Maracy MR, Bacterial contamination of hospital-prepared tube feeding formulas in Isfahan, IranJ Res Med Sci 2008 14(3):149-56. [Google Scholar]
[12]. Borghi R, Dutra Araujo T, Airoldi Vieira RI, Theodoro de Souza T, Waitzberg DL, ILSI task force on enteral nutrition; estimated composition and costs of blenderized dietsNutr Hosp 2013 28(6):2033-38. [Google Scholar]
[13]. Ibrahim EH, Mehringer L, Prentice D, Sherman G, Schaiff R, Fraser V, Early versus late enteral feeding of mechanically ventilated patients: results of a clinical trialJPEN: J Parenter Enteral Nutr 2002 26(3):174-81. [Google Scholar]
[14]. MacLeod JB, Lefton J, Houghton D, Roland C, Doherty J, Cohn SM, Prospective randomized control trial of intermittent versus continuous gastric feeds for critically ill trauma patientsJ Trauma 2007 63(1):57-61. [Google Scholar]
[15]. McClave SA, Taylor BE, Martindale RG, Warren MM, Johnson DR, Braunschweig C, Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (ASPEN.)JPEN: J Parenter Enteral Nutr 2016 40(2):159-211. [Google Scholar]
[16]. McAtear CA, Arrowsmith H, McWhirter J, Current perspectives on enteral nutrition in adults. A report by the British Association for Parenteral and Enteral NutritionMaidenhead: BAPEN 1999 [Google Scholar]
[17]. Klein MD, Morris SE. In: Homemade Blended Formula, Mealtime Notions, LLC, Tucson, AZ, 2007 [Google Scholar]
[18]. Roza AM, Shizgal HM, The Harris Benedict equation reevaluated: resting energy requirements and the body cell massThe American Journal of Clinical Nutrition 1984 40(1):168-82. [Google Scholar]
[19]. Reeves MM, Capra S, Bauer J, Davies PS, Battistutta D, Clinical accuracy of the MedGem indirect calorimeter for measuring resting energy expenditure in cancer patientsEur J Clin Nutr 2005 59(4):603-10. [Google Scholar]
[20]. iNutriMon (http://www.inutrimon.com) [Google Scholar]