Introduction
Preterm delivery remains a challenge in Obstetrics as it is responsible for significant cause of perinatal morbidity and mortality. At present there is no standard test for prediction of preterm labour for timely referral to a center with NICU facilities.
Aim
To evaluate the effectiveness of the cervical phosphorylated insulin like growth factor binding protein-1(phIGFBP-1), cervical length measurement and combination of phIGFBP-1 with cervical length for Predicting Preterm Labour (PTL).
Materials and Methods
It was a observational prospective study done from January 2014 to April 2015 in Department of Obstetrics and Gynaecology, NDMC Medical College and Hindu Rao Hospital, Delhi, India. A total of 100 women with singleton pregnancy, between 24 and 36 weeks of gestation with complaint of uterine contractions were randomly selected. These women were subjected to detect phIGFBP-1 in cervical secretions and cervical length measurement by Transvaginal Sonography (TVS). Result of the test, cervical length and time lapse between test and delivery was noted and the results were analysed. The cervical length less than 25 mm was used as a cut off point for predicting pre-term delivery. Data was analysed using SPSS software version 20.0.
Results
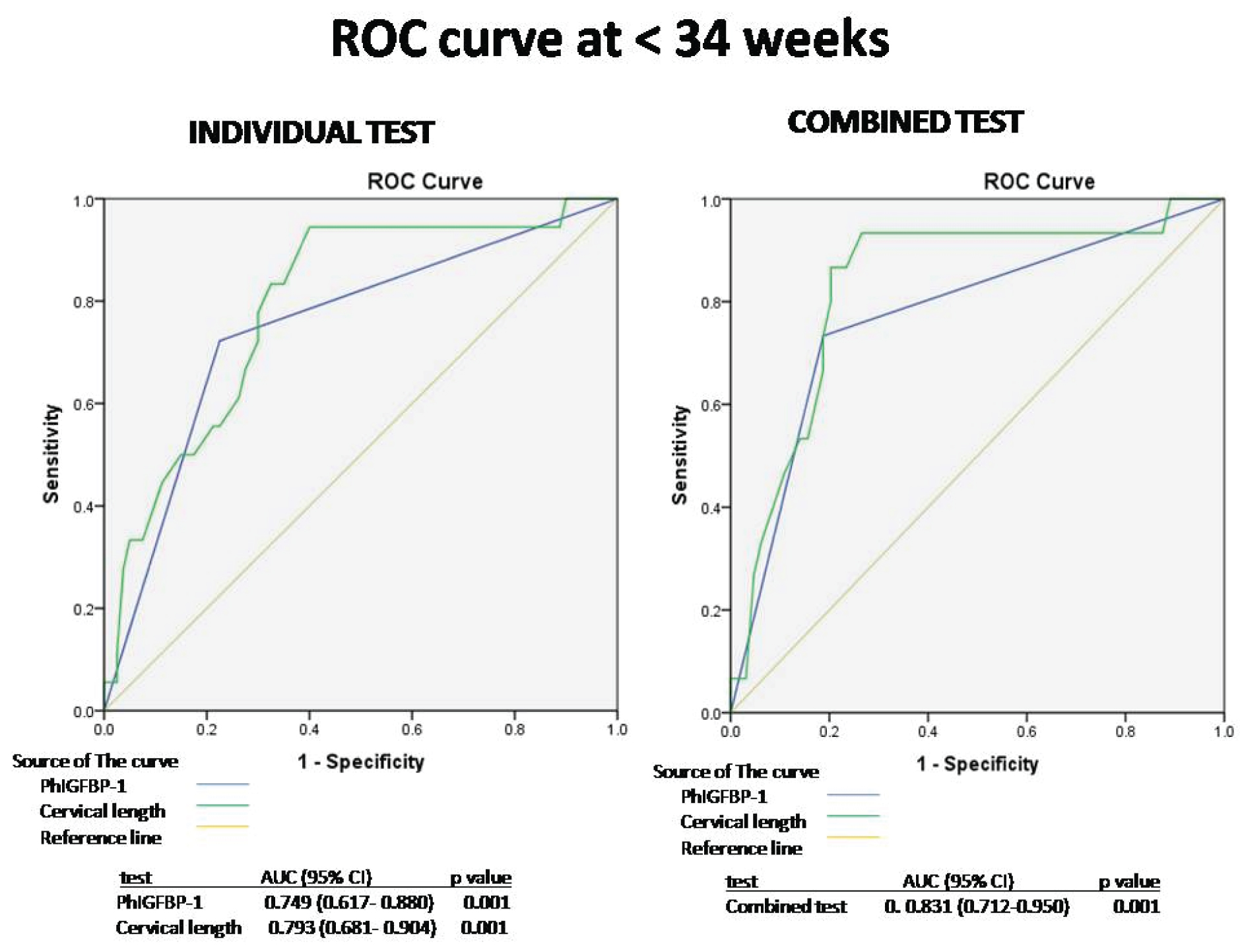
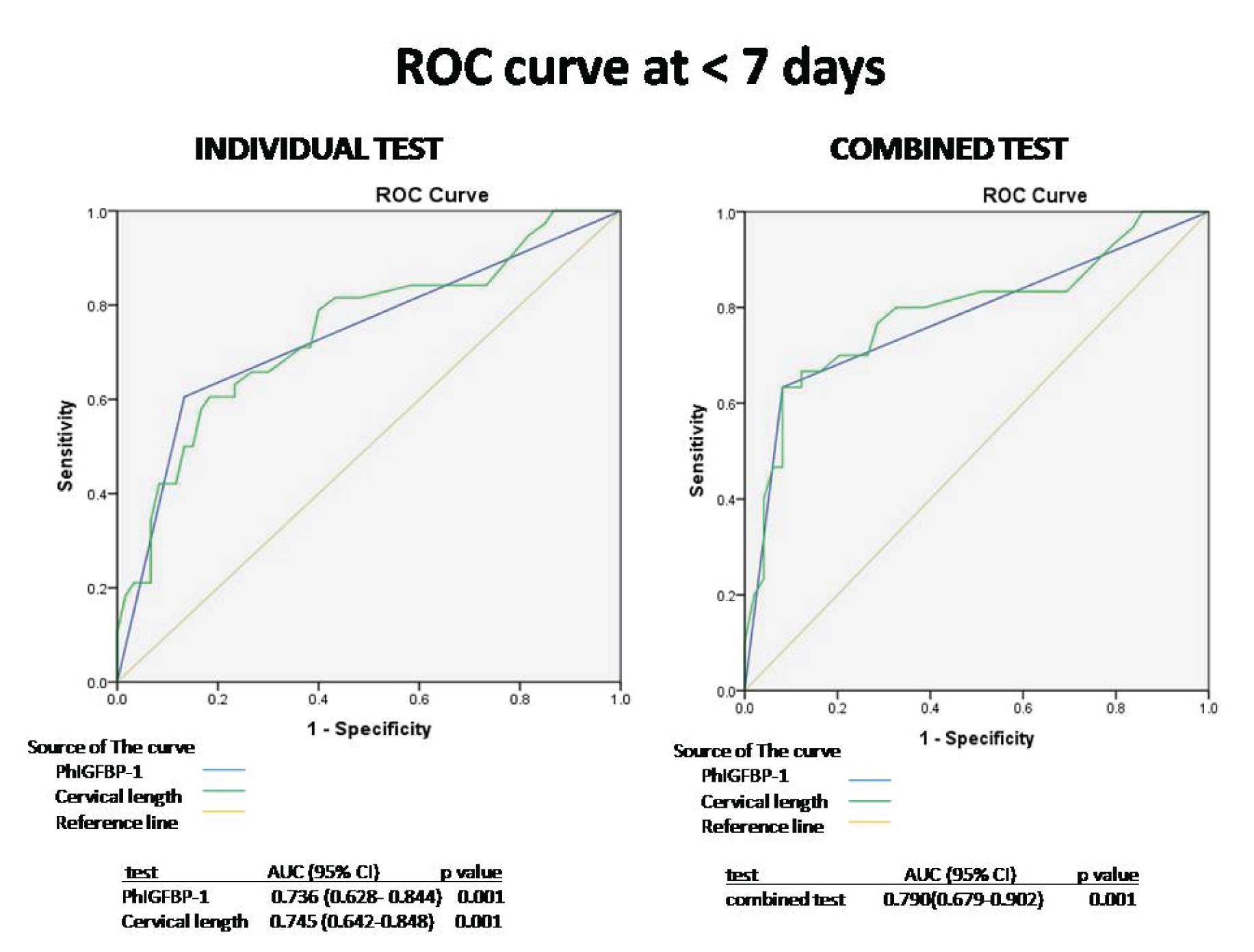
The Negative Predictive Value (NPV) of phIGFBP-1 and cervical length was similar (95.2% vs 94.05%) respectively for prediction of preterm labour within one week of admission and 93.92% vs 94.80% at 37 weeks of gestational age. Combined test had higher NPV of 96.38% at 34 weeks of gestation and 94% within two days of admission. Positive Predictive Value (PPV) was low for both the test and combining the two-test did not have any advantage as far as PPV was concerned. Receiver Operating Characteristic (ROC) curve showed that the combined test had a superior result in predicting PTL compared to either phIGFBP-1 or cervical length. The combined test had steepest ROC curve at < 34 weeks of gestation (AUC-0.83 with 95% CI).
Conclusion
The phIGFBP-1 test and cervical length have an almost equivalent ability to predict preterm delivery independently. The combined use of phIGFBP-1 and TVS for cervical length shows an increase in efficacy in predicting preterm labour.
Introduction
PTL is defined as labour occurring after 20 weeks but before 37 completed weeks of gestation [1]. The incidence of PTL remains constant over recent years, varying from 5%-10% in different populations [2]. In India, the incidence of preterm birth is approximately 13% [3]. It is the most common cause of perinatal morbidity and mortality.
Prediction of PTL is important, so that women can be moved to a higher center for safe confinement as nursery care is of utmost importance for the preterm neonate.
Preterm labour is difficult to predict. At present there is no standard parameter for prediction of PTL. There has been considerable interest in means of identifying women at risk of delivering prematurely by clinical symptoms and signs, biochemical markers and cervical length by digital examination and ultrasound. To achieve this goal, a risk scoring system, biochemical markers derived from different body fluids, tissues and radiological parameters like cervical length have been used.
The risk scoring system based on demographic characteristics like socioeconomic status, antenatal care, maternal age, nutrition, smoking, drug abuse, alcohol, physical work, genetic predisposition, uterine malformations, previous surgery on cervix, short cervix, preterm premature rupture of membranes, multiple pregnancy is not reliable. In primi gravida, this scoring system cannot be used as there is no past obstetric history.
A shortened or open cervix between 24 and 28 weeks indicates an elevated risk for PTL [4]. A shortened cervical length detected by TVS below the 10th percentile for gestational age, increased the risk of PTL prior to 35 weeks by 6 folds [5]. A review of 35 studies using sonographically assessed cervical length to predict preterm delivery in asymptomatic women found sensitivities ranging from 68% to 100% and specificities from 44% to 79% with wide variations in their predictive values [6]. A more recent meta-analysis of 28 studies assessing cervical length (<15 mm) in symptomatic women with threatened PTL found sensitivities ranging from 53% to 67% and specificities ranging from 89% to 92% for delivery within one week [7]. Due to limitations in ultrasound availability and operator expertise, cervical length alone cannot be reliably utilized to predict preterm labour or used as a routine screening tool [8]. Therefore, the current evidence and practice do not allow the development of a consensus on use of TVS alone for prediction of preterm labour.
Various body fluids, tissues have been used for prediction of preterm labour like blood, urine, saliva, amniotic fluid, and cervical secretion. In cervical secretion foetal Fibronectin (fFN) and phosphorylated insulin-like growth factor binding protein-1 (phIGFBP1) have been used as biochemical marker. fFN, a glycoprotein produced by trophoblast, has a 78%–89% sensitivity and 86% specificity in symptomatic women. Due to its limitations like amniotic fluid contamination, vaginal bleeding, and unprotected sexual intercourse, it has limited application. Therefore, it is used clinically for its negative predictive value [9].
Identification of phIGFBP-1 in cervical secretions, has been proposed as an option in predicting preterm delivery in threatening preterm labour. The phIGFBP-1 is part of the insulin like growth factor system synthesized in the decidua and liver. Amniotic fluid contains non- phosphorylated and lesser amount of phosphorylated isoform. As the delivery approaches, foetal membrane begins to detach from the decidua parietalis and phIGFBP-1 leaks into cervical secretion. Advantage of using phIGFBP-1 in contrast to fFN, is that only minimal amounts of phIGFBP-1 are present in urine and seminal plasma [10]. Therefore, recent intercourse and urine contamination do not limit the use of the phIGFBP-1 test. The sensitivity, specificity, PPV and NPV for the phosphorylated IGFBP-1 test are 78%, 87%, 73% and 90% [10]. Thus, use of phIGFBP-1 alone in predicting preterm labour is limited. We therefore, plan to study prediction of preterm labour using both the parameters cervical length by TVS and testing of phIGFBP-1 in cervical secretion.
Materials and Methods
A prospective observational study was conducted from January 2014 to April 2015 in Department of Obstetrics and Gynaecology at tertiary care institute NDMC Medical College and Hindu Rao Hospital, Delhi, India, after approval from Institutional Ethical Committee (HRH/ 14014 dated 5/11/13) of the hospital. Informed written consent was taken from all the participants.
Inclusion criteria: Women who presented to casuality/Gynae OPD with complaints of uterine contractions between 24 and 36 weeks of gestation suspected to have threatened labour, were included in the study.
Exclusion criteria: Women with Premature Rupture of Membranes (PROMs), active labour, multifoetal pregnancy, antepartum haemorrhages (placental abruption, placenta previa), gestational hypertension, pre-eclampsia, eclampsia, foetal distress (non- reassuring foetal heart rate in cardiotocograph tracing), history of cervical surgery, cervical incompetence or presence of a cerclage suture, chronic maternal diseases (hypertension, diabetes, renal or cardiac diseases), genital tract anomalies of the women, genetic or anatomical defects of the foetus, or digital examination within 24 hours of examination were excluded from the study.
Sample size calculation (n) = Z2α/2 P (1-P)/d2
Z α/2 = is standard normal variant, α = the level of significance. For α = 0.05, Z α/2 = 1.96, P=Expected proportion in population based on previous studies, d= Absolute error /precision. On the basis of studies, P=0.13, d=0.03. On the basis of formula, we calculated sample size of 90 (approximately), and for convenience, sample size of 100 was taken.
Women with history of preterm labour pains were evaluated with detailed history, physical examination, obstetric examination, per speculum examination for confirmation of diagnosis of threatened preterm labour (uterine contraction without change in cervical dilatation). Demographic details such as age, Body Mass Index (BMI), gravidity, previous history of Preterm Delivery (PTD), history of spontaneous abortions, gestational age at enrollment, gestational age at delivery were noted in a pre-designed proforma.
Cervical secretion were tested for phIGFBP-1 (Actim® Partus) followed by TVS for cervical length measurement.
Test for phIGFBP-1: It is a visually interpreted, qualitative immune chromatographic dipstick test. It has two monoclonal antibodies to human phIGFBP-1 on the dipstick. The kit contains sterile polyester swab, specimen extraction solution in a tube. The extraction solution contains bovine serum albumin and protease inhibitors. A speculum was inserted in vagina and the external cervical os was visualized to rule out leaking of amniotic fluid. Cervical secretions were taken by keeping swab at the external cervical os for 10-15 seconds. The swab was then placed in the extraction solution tube and shaken for approximately 10 seconds. Swab was pressed against the wall of the extraction solution tube to squeeze out liquid. The swab was then discarded and dipstick placed into the extracted specimen until liquid reaches the result area. The result was read either negative (control line only) or positive depending upon presence of two blue lines (a control line and a test line) in the result area. A blue line, test line appears in the result area if the concentration of phIGFBP-1 in the sample exceeds 10 mcg/l. A second blue line, control line confirms correct performance of the test.
Measurement of cervical length: After collection of the cervical sample, TVS was done for measurement of cervical length. It was measured with 5 MHz vaginal probe placed in the anterior fornix of the vagina. The distance between the external and internal os was taken as the cervical length. An average of three readings was taken. The cervical length less than 25 mm was used as a cut off point for predicting pre-term delivery.
After TVS, digital examination was done to know dilatation and effacement. Women with more than 3 cms dilatation and 100% effacement and leaking were excluded from the study.
All women were given Injection betamethasone and tocolysis for 48 hours for lung maturity. Women were followed up till the time they delivered.
Statistical Analysis
Maternal demographic characteristics were evaluated by Student’s t-test for two groups, with the values being expressed as the mean±SD. Chi-square test was used to analyse the categorical variables. Receiver–Operating Characteristics (ROC) curves were constructed and the Area Under the Curve (AUC) was used to compare the predictive value of phIGFBP-1 and cervical length at different gestational ages in predicting spontaneous preterm delivery at <2 days, <7 days and <14 days of admission and at <34 weeks and <37 weeks of gestation and to determine the most useful cutoff point (with highest overall accuracy) for cervical length in predicting preterm delivery. Sensitivity, specificity, positive predictive value, negative predictive value and positive and negative Likelihood Ratio (LR) and Confidence Intervals (CIs) were also calculated. This analysis was done in Statistical Software SPSS version 20.0 and a p-value <0.05 was considered as statistically significant.
Results
Out of 100 women enrolled in study, results of 98 women were analysed as two women had repeated invalid phIGFBP-1 test kit result. Demographic profile given in [Table/Fig-1] is comparison between different groups with respect to age, BMI etc., except for number of women with history of previous preterm delivery.
Maternal demographic and obstetrics characteristics of study population.
| Demographic and obstetrical Variables | phIGFBP-1 | Cervical Length |
|---|
| Positive | Negative | *p-value | <2.5 cm | ≥2.5 cm | *p-value |
|---|
| n=31 | n=67 | n=34 | n=64 |
|---|
| Age (years) | 23.16±3.29 | 24.55±3.71 | 0.373 | 23.80±3.31 | 24.28±3.8 | 0.918 |
| BMI (kg/m2) | 26.08±3.58 | 24.45±3.7 | 0.082 | 25.59±3.68 | 24.64±3.76 | 0.543 |
| Gravidity | 1.97±0.91 | 1.85±0.89 | 0.832 | 1.85±0.89 | 1.91±0.89 | 0.676 |
| Previous Preterm Delivery n=21 | 1.42±0.50 | 1.16±0.48 | 0.001 | 1.32±0.47 | 1.20±0.51 | 0.019 |
| Previous Abortion n=23 | 1.35±0.66 | 1.28±0.57 | 0.802 | 1.24±0.55 | 1.34±0.62 | 0.603 |
| Cervical Length (cm) | 2.18±0.88 | 3.51±0.86 | 0.7 | - | -- | - |
| Gestational age at Enrollment (weeks) | 32.60±2.43 | 32.83±2.24 | 0.68 | 32.42±2.88 | 32.93±1.92 | 0.073 |
| Gestational age at Delivery (weeks) | 34.32±3.10 | 37.19±2.42 | 0.001 | 34.63±2.99 | 37.17±2.56 | 0.001 |
| Enrollment to Delivery Interval (days) | 9.10±16.89 | 28.81±21.35 | 0.001 | 11.91±19.87 | 28.23±21.06 | 0.001 |
*p < 0.05= significant, chi-square test, student t-test
Mean maternal age was 24.11±3.6 years. The number of primi gravida in study population was 46%. Mean BMI was 24.9±3.74 kg/m2. Mean gestational age at enrollment was 32.75±2.29 weeks; mean age at delivery was 36.29±2.96 weeks.
The cervical length less than 2.5 cm was recorded as positive. Mean cervical length of study group (98) was 3.09±1.06 cm. Mean cervical length for those women who tested phIGFBP-1 positive was 2.18±0.88 cm and for phIGFBP-1 negative was 3.51±0.86 cm.
Of 31 women with phIGFBP-1 positive test, 61.3% (19/31) delivered within 2 days and 12.9% (4/31) delivered between 3 to 7 days of admission. Among 67 women who had phIGFBP-1 negative test, 14.9 % (10/67) delivered within 2 days and 7.46% (5/67) delivered between 3 to 7 days. There were 34 women with cervical length of <2.5 cm, 52.9% (18/34) delivered within 2 days and 14.7% (5/34) delivered between 3 to 7 days. Of 64 women who had cervical length ≥2.5 cm, 17.1 % (11/64) delivered within 2 days and 6.25 % (4/64) delivered between 3 to 7 days. There were 23 women with both phIGFBP-1 positive and cervical length <2.5 cm, 65.21% (15/23) delivered within 2 days and17.39% (4/23) delivered between 3 to 7 days [Table/Fig-2].
Relationship of the test with time of delivery.
| Test | Time of delivery |
|---|
| 2 days | 3-7days | 8-14 days | >14 days |
|---|
| *phIGFBP-1(+), n=31 | 19 | 4 | 2 | 6 |
| phIGFBP-1 (-), n=67 | 10 | 5 | 5 | 47 |
| Cervical length<2.5 cm, n=34 | 18 | 5 | 3 | 8 |
| Cervical length≥ 2.5 cm, n=64 | 11 | 4 | 4 | 45 |
| †Combined test, n=23 | 15 | 4 | 2 | 2 |
* phosphorylated insulin-like growth factor-binding protein-1 † phosphorylated insulin-like growth factor-binding protein-1 positive and cervical length < 2.5 cm
ROC curves show that the combined test had a superior result in predicting PTL compared to either phIGFBP-1 or cervical length. The combined test has steepest ROC curve at < 34 weeks of gestation (AUC-0.831 with 95% CI). [Table/Fig-3,4].
Comparison of phIGFBP-1, cervical length and combined test by ROC-curve.
| Test Result Variable(s) | Parameter | Area | Std. Error | Asymptotic Sig. | Asymptotic 95% Confidence Interval |
|---|
| Lower Bound | Upper Bound |
|---|
| <2 days | phIGFBP-1 | 0.741 | 0.059 | 0.001 | 0.626 | 0.856 |
| Cervical length | 0.739 | 0.055 | 0.001 | 0.632 | 0.845 |
| Combined test | 0.793 | 0.058 | 0.001 | 0.681 | 0.906 |
| <7 days | phIGFBP-1 | 0.736 | 0.055 | 0.001 | 0.628 | 0.844 |
| Cervical length | 0.745 | 0.053 | 0.001 | 0.642 | 0.848 |
| Combined test | 0.790 | 0.057 | 0.001 | 0.679 | 0.902 |
| <14 days | phIGFBP-1 | 0.721 | 0.054 | 0.001 | 0.616 | 0.826 |
| Cervical length | 0.742 | 0.051 | 0.001 | 0.641 | 0.842 |
| Combined test | 0.774 | 0.056 | 0.001 | 0.665 | 0.883 |
| <34 weeks | phIGFBP-1 | 0.749 | 0.067 | 0.001 | 0.617 | 0.880 |
| Cervical length | 0.793 | 0.057 | 0.001 | 0.681 | 0.904 |
| Combined test | 0.831 | 0.061 | 0.001 | 0.712 | 0.950 |
| <37 weeks | phIGFBP-1 | 0.658 | 0.055 | 0.008 | 0.550 | 0.765 |
| Cervical length | 0.711 | 0.052 | 0.001 | 0.609 | 0.813 |
| Combined test | 0.7270.058 | 0.058 | 0.001 | 0.614 | 0.840 |
ROC curve by their sensitivity and specificity (<34weeks).
Discussion
Preterm delivery is a major cause of neonatal morbidity and mortality. Preterm labour has multiple aetiologies and there is no single marker to predict preterm labour. This study was conducted on 100 symptomatic women. The main outcome of our study is that pre-term birth is unlikely when the results of both tests, i.e., phIGFBP-1 and cervical measurements are negative. Based on the results of the present study, the absence of phIGFBP-1 in cervical secretions and cervical length of > 2.5 cm in symptomatic pregnant women are at low-risk for preterm delivery. This will avoid unnecessary admissions and reduce burden on health facilities. It also gives time to transport baby in utero to medical facility with nursery.
The rapid tests which can be done in cervical secretions are fetal fibronectin and phIGFBP-1. fFN is used clinically for its negative predictive value, which exceeds 95% in some studies [11]. The phIGFBP1 test has a comparable NPV to the fFN test in predicting spontaneous PTL within seven days in symptomatic women (phIGFBP1 92% vs. fFN 97%) [12].
This study was done to know whether combining phIGFBP-1and cervical length (two independent variables) [13] will improve prediction of preterm labour. Present study evaluated 98 symptomatic women, NPV at less than 34 weeks of gestation for phIGFBP-1, cervical length and combined test were quite high (91.4%, 90.3%, 96.38% respectively) [Table/Fig-5]. PPV was quite low at all stages of gestation for phIGFBP-1, cervical length and combined test (45.49%, 35.90%, 37.06% respectively at 34 weeks gestation). Azlin M et al., has reported PPV of 51.1%, 23.8% and 80% respectively [14].
Diagnostic accuracy of phIGFBP-1, cervical length and combined test.
| Tests | Time of Delivery | Period of Gestation |
|---|
| <2 Days | <7 Days | < 14 Days | <34 Weeks | < 37 Weeks |
|---|
| phIGFBP-1 | Sensitivity | 60.5% | 74.20% | 80.60% | 41.90% | 80.60% |
| Specificity | 85.10% | 77.60% | 70.10% | 92.50% | 44.80% |
| *PPV | 37.60% | 33.10% | 28.71% | 45.49% | 17.91% |
| †NPV | 93.50% | 95.26% | 96.02% | 91.40% | 93.92% |
| ‡LR(+) | 4.06 | 3.31 | 2.69 | 5.58 | 1.46 |
| LR(-) | 0.46 | 0.33 | 0.27 | 0.62 | 0.43 |
| Cervical length | Sensitivity | 52.90% | 67.60% | 76.50% | 35.30% | 79.40% |
| Specificity | 82.80% | 76.60% | 71.00% | 90.60% | 56.20% |
| PPV | 30.90% | 30.15% | 28.27% | 35.90% | 21.13% |
| NPV | 92.13% | 94.05% | 95.28% | 90.35% | 94.80% |
| LR(+) | 3.07 | 2.28 | 2.63 | 3.75 | 1.81 |
| LR(-) | 0.57 | 0.42 | 0.33 | 0.71 | 0.36 |
| Combined test | Sensitivity | 72.0% | 70.0% | 64% | 80.0% | 61.0% |
| Specificity | 74.0% | 79.61% | 81.4% | 79.7% | 81.0% |
| PPV | 29.0% | 33.35% | 33.9% | 37.06% | 32.0% |
| NPV | 94.0% | 94.63% | 93.78% | 96.38% | 93.0% |
| LR(+) | 2.74 | 3.34 | 3.43 | 3.94 | 3.11 |
| LR(-) | 0.38 | 0.53 | 0.44 | 0.25 | 0.49 |
*PPV- Positive predictive value, †NPV- Negative predictive value, ‡LR Likelihood ratio
Study by Hadzi-Lega M et al., correlated cervical length, phIGFBP-1 in spontaneous preterm birth up to 14 days from sampling in 58 patients with symptoms suggestive of preterm labour, and found that patients with a positive test had an average cervical length of 18.5±4.63 mm, which is significantly lower than patients with a negative test 23.43±7.39 mm [15]. However, in our study the mean cervical length was 2.18±0.88 cm and 3.51±0.86 cm in phIGFBP-1 positive women and negative women respectively which was not significant (p-value > 0.05).
Danti L et al., studied 102 consecutive symptomatic women with singleton pregnancies and reported that a positive phIGFBP-1 significantly increased risk of delivery before 34 weeks in women with a cervix ≤3.0 cm (likelihood ratio 2.32). The likelihood ratio for risk of delivering within 7 days in women with a cervical length of <2.5 cm was 2.28 in our study, which was lower than study by Danti L et al., (likelihood ratio 3.64) because the cutoff for cervical length in our study was taken as 2.5 cm [16].
The ROC curves were used to compare the performance of phIGFBP-1, cervical length and combining both variables. Cervical length and pIGFBP-1 had almost similar AUC (0.745, 0.736 respectively) for prediction of delivery at 7 days time [Table/Fig-3,6], whereas Aziln MI et al., had more AUC for phIGFBP-1 (0.867) than for cervical length (0.759) [14].
ROC curve by their sensitivity and specificity (<7 days).
For prediction of delivery <34 weeks of gestation, the AUC for pIGFBP-1 was 0.749 in our study similar to study by Bittar RE et al., (AUC 0.75) [17].
The ROC curve shows that the combined use of phIGFBP-1 and cervical length had a better result at 34 and 37 weeks gestation (AUC 0.831, 0.727 respectively) in predicting PTL compared with either phIGFBP-1(0.749, 0.658 respectively) or cervical length alone (0.793, 0.711 respectively).
Limitation
Controls (asymptomatic pregnant women) were not included in the study. Various risk factors for preterm labour were not taken into consideration. Combined use of phIGFBP-1 and cervical length had a better result and has best negative predictive value and should be recommended to women with threatened preterm labour.
Conclusion
Rapid phIGFBP-1 tests and cervical length have an almost equivalent ability to predict preterm delivery independently. The combined use of phIGFBP-1 and cervical length shows an increase in efficacy in predicting PTL as compared with either indicator alone. The negative phIGFBP-1 and cervical length > 2.5 cm can be reassuring sign that a woman is unlikely to give preterm birth.
*p < 0.05= significant, chi-square test, student t-test
* phosphorylated insulin-like growth factor-binding protein-1 † phosphorylated insulin-like growth factor-binding protein-1 positive and cervical length < 2.5 cm
*PPV- Positive predictive value, †NPV- Negative predictive value, ‡LR Likelihood ratio
[1]. Roman AS, Current Diagnosis & Treatment Obstetrics & Gynaecology. 11e > Chapter 14>Late Pregnancy Complications > Preterm Labour [Google Scholar]
[2]. Altinkaya O, Gungor T, Ozat M, Danisman N, Mollamahmutoglu L, Cervical Phosphoryalted insulin-like growth factor-binding protein-1 in prediction of preterm deliveryArchives of Gynaecology & Obstetrics 2009 279(3):279-83. [Google Scholar]
[3]. Eds CP, Howson Kinney MV, Lawn JE, World Health Organization Geneva. Born Too Soon: The Global Action Report on Preterm Birth 2012 Apr 3 [Google Scholar]
[4]. Papiernik E, Keith LG, Bouyer J, Dreyfus J, Lazar P, Risk factors identified during prenatal consultations. Effective prevention of preterm birth: the French Experience measured at HuguenauMarch of Dimes Birth Defects Foundation 1989 25(1)New YorkWhite Plains [Google Scholar]
[5]. Norwitz ER, Robinson JN, A systematic approach to the management of preterm labourSeminars in Perinatology 2001 25(4):223-35. [Google Scholar]
[6]. Watson WJ, Stevens D, Welter S, Day D, Observations on the sonographic measurement of cervical length and the risk of premature birthJournal of Maternal-Fetal Medicine 1999 8(1):17-19. [Google Scholar]
[7]. Sotiriadis A, Papatheodorou S, Kavvadias A, Makrydimas G, Transvaginal cervical length measurement for prediction of preterm birth in women with threatened preterm labour: a meta-analysisUltrasound in Obstetrics and Gynaecology 2010 35(1):54-64. [Google Scholar]
[8]. Berghella V, Baxter JK, Hendrix NW, Cervical assessment by ultrasound for preventing preterm deliveryCochrane Database of Systematic Reviews 2013 1:CD007235 [Google Scholar]
[9]. Leitich H, Egarter C, Kaider A, Hoblagschwandtner M, Berghammer P, Husslein P, Cervicovaginal fetal fibronectin as a marker for preterm delivery: a meta-analysisAmerican Journal of Obstetrics and Gynaecology 1999 180(5):1169-76. [Google Scholar]
[10]. Akercan F, Kazandi M, Sendag F, Cirpan T, Mgoyi L, Terek MC, Value of cervical phosphorylated insulin like growth factor binding protein 1 in the prediction of pre-term labourJ Reprod Med 2004 49(5):368-72. [Google Scholar]
[11]. Leitich H, Egarter C, Kaider A, Hoblagschwandtner M, Berghammer P, Husslein P, Cervicovaginal fetal fibronectin as a marker for preterm delivery: a meta-analysisAmerican Journal of Obstetrics and Gynaecology 1999 180(5):1169-76. [Google Scholar]
[12]. Ting HS, Chin PS, Yeo GS, Kwek K, Comparison of bedside test kits for prediction of preterm delivery: phosphorylated insulin-like growth factor binding protein-1 (pIGFBP-1) test and fetal fibronectin testAnn Acad Med Singap 2007 36:399-402. [Google Scholar]
[13]. Riboni F, Vitulo A, Plebani M, Dell’Avanzo M, Battagliarin G, Surico N, Phosphorylated insulin-like growth factor binding protein-1 in cervical secretions and sonographic cervical length in the prediction of spontaneous preterm deliveryUltrasound Obstet Gynaecol 2009 34(4):437-40. [Google Scholar]
[14]. Azlin MI, Bang HK, An LJ, Mohamad SN, Mansor NA, Yee BS, Role of phIGFBP-1 and ultrasound cervical length in predicting pre-term labourJ Obstet Gynaecol 2010 30(5):456-59. [Google Scholar]
[15]. Hadzi-Lega M, Markova AD, Stefanovic M, Tanturovski M, Correlation of cervical length, fetal fibronectin, phIGFBP-1, and cytokines in spontaneous preterm birth up to 14 days from samplingJ Perinat Med 2015 43(5):545-51. [Google Scholar]
[16]. Danti L, Prefumo F, Lojacono A, Corini S, Testori A, Frusca T, The combination of short cervical length and phIGFBP-1 in the prediction of preterm delivery in symptomatic womenJournal of Maternal-Fetal and Neonatal Medicine 2011 24(10):1262-12. [Google Scholar]
[17]. Bittar RE, da Fonseca EB, de Carvalho MH, Martinelli S, Zugaib M, Predicting preterm delivery in asymptomatic patients with prior preterm delivery by measurement of cervical length and phosphorylated insulin-like growth factor-binding protein-1Ultrasound Obstet Gynaecol 2007 29:562-67. [Google Scholar]