Epituberculosis Revisited: Case Report and Review
Lavina Vishnu Mirchandani1, Sindhu S Kamath2, Jayalakshami Thelapurath Kutty3, Aparna Iyer4
1 Associate Professor, Department of Pulmonary Medicine, Dr. D.Y. Patil University, College of Medicine, Navi Mumbai, Maharashtra, India.
2 Resident, Department of Pulmonary Medicine, Dr. D.Y. Patil University, College of Medicine, Navi Mumbai, Maharashtra, India.
3 Professor, Department of Pulmonary Medicine, Dr. D.Y. Patil University, College of Medicine, Navi Mumbai, Maharashtra, India.
4 Assistant Professor, Department of Pulmonary Medicine, Dr. D.Y. Patil University, College of Medicine, Navi Mumbai, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Lavina Vishnu Mirchandani, Shyam kutir CHS, Flat # 302, 13th Road, TPS III, Plot 629, Khar West, Mumbai-400052, Maharashtra, India.
E-mail: drlavinamir@gmail.com
Primary pulmonary tuberculosis can involve regional lymph nodes which may resolve spontaneously or on treatment; or they may enlarge causing extrinsic bronchial compression; or cause endobronchial inflammation and ulceration; or a node may erode through the bronchial wall with extrusion of caseous materials into the bronchial tree, causing focal or lobar pneumonia. This erosion is seen radiologically as hilar lymphadenopathy, with atelectasis and consolidation and described as “epituberculosis”. It is more common in infants than older children. We hereby describe the case of a 13-year-old child with right hilar lymphadenopathy and right upper lobe consolidation on chest x-ray. We demonstrated by fibreoptic bronchoscopy that this epituberculosis resulted from perforation of a lymph node and discharge of caseous material into the upper lobe bronchus with resultant endobronchial obstruction. Thus a tuberculous ruptured lymph node may lead to clinical and radiological worsening, but this does not indicate development of drug resistance in these patients and they respond well to the same treatment regimen.
Atelectasis, Collapse, Consolidation, Hilar lymphadenopathy
Case Report
A 13-year-old female presented to us with complaints of continuous low grade fever with evening rise of temperature, not associated with chills and rigors. She had no weight loss but there was loss of appetite since about one month. Patient had no cough, expectoration, haemoptysis, chest pain, dyspnoea or joint pains.
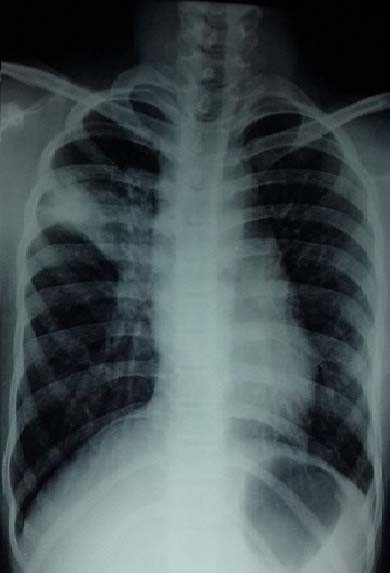
Patient gave history of having large, palpable cervical lymph node swelling seven months back for which she consulted a private physician. He advised Fine Needle Aspiration Cytology (FNAC) of the cervical lymph node and chest x-ray [Table/Fig-1]. X-ray chest showed right hilar and right small paratracheal lymph node but no parenchymal lesion. The Grunwald Geimsa stained smears of FNAC showed heterogeneous population of lymphocytes along with focal wall epitheliod cell granulomas suggestive of granulomatous lymphadenitis. Physician started the patient on Antituberculous Treatment (ATT), with weight adjusted doses of Ethambutol (E), Isoniazid (I), Rifampicin (R), Pyrazinamide (Z) for two months followed by two drugs (EHR) for four months. After three months of treatment, patient followed up for routine checkup with her treating physician. At that time she had no fever and the cervical lymph node had regressed in size, however the chest x-ray repeated by her doctor [Table/Fig-2] showed increase in size of hilar lymph node. The treating physician asked the patient to continue the same ATT for another three months.
X-ray chest (first) shows enlarged right hilar and paratracheal lymph node.

X-ray chest (after three months) shows increase in size of lymph node.

After one more month of ATT i.e., she had now completed intensive phase and two months of continuation phase of ATT; patient came to us at our hospital as she had started getting low grade fever. Her clinical examination revealed less than 1cm sized right anterior cervical lymph node and bronchial breath sounds in right upper lobe with crepitations. X-ray chest was advised which showed right upper lobe consolidation with signs of volume loss and right hilar lymph node [Table/Fig-3]. All blood investigations including complete blood count, liver function tests, and renal function tests were within normal limits. Sputum tests could not be done as patient had no expectoration.
X-ray chest (after four months) shows right upper lobe consolidation.

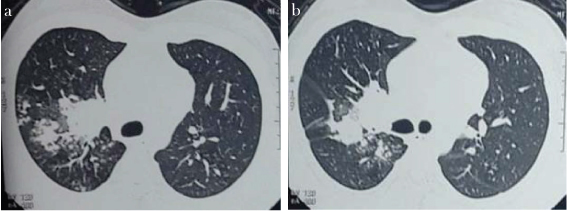
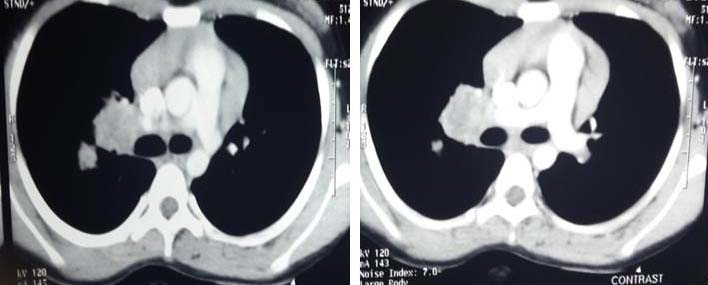
High Resolution Computed Tomography (HRCT) thorax was done which showed patchy consolidation with multiple tiny branching centrilobular nodules with tree in bud appearance in apical and posterior segment of right upper lobe and ground glass opacities in right lower lobe, superior and anterior basal segments. Pleural thickening was present along left lower lobe. Multiple enlarged necrotic lymph nodes were noted in pre/paratracheal, prevascular, right hilar and bilateral supraclavicular regions; largest measuring 3.5 x 3.3 cm at right hilum region [Table/Fig-4a,b,5a.b].
HRCT thorax lung window shows patchy consolidation, centrilobular nodules and tree in bud appearance.
HRCT thorax mediastinal window shows multiple enlarged necrotic lymph nodes in pre/paratracheal, prevascular, right hilar region.
Bronchoscopy done showed occlusion of right upper lobe by cheesy soft friable mass, which was biopsied [Table/Fig-6a-d]. Biopsy showed mainly bronchial mucosal wall with sparse alveolar lung tissue. There were caseating epithelioid granulomas in the mucosa suggesting tuberculosis but no Acid Fast Bacilli (AFB) were seen. Bronchoalveolar Lavage (BAL) was also negative for AFB and liquid Mycobacteria Growth Indicator Tube (MGIT) culture showed no growth of Mycobacterium Tuberculosis (M.TB). Bronchoalveolar Lavage (BAL) Gram stain and fungal culture also showed no growth of organisms. BAL cytology was negative for malignant cells. Post bronchoscopy sputum was also negative for AFB.
Endobronchial mass in right upper lobe on bronchoscopy.

Patient was started on Anti Kochs Treatment (AKT), Category (CAT) II i.e., five first line drugs (Streptomycin with HERZ) in weight adjusted doses for two months, followed by HERZ for one month, followed by HRE for five months, while being monitored continuously. She responded well to treatment, her symptoms subsided and her x-ray chest done one month [Table/Fig-7] and three months later [Table/Fig-8] showed dramatic improvement.
X-ray chest (after six months) shows resolving consolidation.
X-ray chest (after eight months) shows resolution.

Discussion
Primary infection with M.TB begins with deposition of infected droplets in the lung alveoli, followed by parenchymal inflammation which leads to an alveolar consolidation not usually visible on chest x-ray. It may sometimes be visible as a localized, sub pleural infiltrate traditionally called the primary focus or Ghon focus. From the primary focus, infection does spread to the central lymph nodes via draining lymphatic vessels, appearing on X-ray as linear interstitial pattern with enlarged lymph nodes, the primary complex or Ghon complex [1]. Usually this complex resolves spontaneously. In some cases, the involved lymph nodes continue to enlarge and there is caseation necrosis within the nodes. Such enlarged nodes may compress the regional bronchi and cause bronchial narrowing, obstruction, and emphysema or they can perforate a nearby bronchus and discharge caseous material into the bronchial tree, causing bronchogenic tuberculosis and focal or lobar pneumonia [2]. This erosion is seen radiologically as hilar lymphadenopathy, with atelectasis and consolidation and described as “collapse-consolidation,” “segmental lesions,” or “epituberculosis”. With appropriate treatment, most segmental lesions resolve completely [3]. As early as 1950, Brock RC also observed that the disease process resolves with little residual disease or disability [4]. Epituberculosis is more common in infants because they have soft and elastic bronchi [5], and tends to occur within months of the initial infection, however our case was unusual as it occurred in an older child.
Eliasberg and Neuland who had coined the term epi-tuberculosis, suggested that these pathological alterations were a reaction to toxins produced by a tuberculous focus [2]. Reichle HS assumed that epituberculosis is in many cases merely an extensive tuberculous pneumonia, differing from the ordinary type by undergoing complete reabsorption [6]. De Bruin M suggested that epituberculosis was due to atelectasis caused by occlusion of a main bronchus [7]. A recent study reevaluated the pathogenesis of epituberculosis, because most studies on epituberculosis have been done more than 50 years ago. It is confirmed with CT imaging and bronchoscopy that epituberculosis is the atelectasis of lobe or segment which occurs mostly due to compression of bronchi by the enlargement of mediastinal and/or hilar lymph nodes especially after starting chemotherapy [8]. Perforation of lymph nodes partially contributes to the formation of epituberculosis as confirmed by bronchoscopic findings in this study. Thus, the distal parenchymal shadow following tuberculous lymphadenitis may be due to the extruded caseous material causing obstruction and atelectasis, and/or due to acute hypersensitivity response to extruded material and/or caseating pneumonia due to the extruded material. In our case, x-ray and HRCT chest demonstrated necrotic lymph nodes and collapse-consolidation of right upper lobe. Bronchoscopy showed occlusion of right upper lobe bronchus by cheesy soft friable mass which was probably the perforated lymph node, which had led to collapse-consolidation of right upper lobe.
Epituberculosis may occur despite adequate chemotherapy. It is well known that the enlargement or appearance of new lymph nodes during or after chemotherapy does not necessarily indicate failure of the treatment or relapse or drug resistant TB. In fact, it may be due to hypersensitivity to tuberculoproteins released from disrupted macrophages [9]. Similarly, nodal perforation into an airway with endobronchial aspiration of allergic products causes an acute hypersensitivity response (epituberculosis) with dense consolidation [10]. This consolidation does not need any change in ATT and resolves completely within months, without permanent sequelae. A response to the same anti-tubercular treatment substantiates the diagnosis, as was reported in a similar case from India [9]. Our patient also has responded well to first line ATT both clinically and radio logically.
Conclusion
We report this case to emphasize that involvement of lymph nodes can occur in older children leading to collapse consolidation i.e., epituberculosis due to erosion of the lymphnode into the bronchus and subsequent acute hypersensitivity response to the tuberculoproteins released. This may lead to clinical and radiological worsening; however, this does not mean that patients are developing drug resistant TB. Such patients require close observation and thorough investigation, and if they have epituberculosis, they usually respond well without any change in their anti TB regimen.
[1]. Kim WS, Choi J-I, Cheon J-E, Yeon KKM, Lee HJ, Pulmonary tuberculosis in infants: radiographic and ct findingsAJR 2006 187:1024-33. [Google Scholar]
[2]. Morrison JB, Natural history of segmental lesions in primary pulmonary tuberculosis: Long-term review of 383 patientsArch Dis Child 1973 48(2):90-98. [Google Scholar]
[3]. De Villiers RV, Andronikou S, Van de Westhuizen S, Specificity and sensitivity of chest radiographs in the diagnosis of paediatric pulmonary tuberculosis and the value of additional high-kilovolt radiographsAustralas Radiol 2004 48(2):148-53. [Google Scholar]
[4]. Brock RC, Post-tuberculous bronchostenosis and bronchiectasis of the middle lobeThorax 1950 5:5-39. [Google Scholar]
[5]. Nakazono T, Ogata H, Mizutani S, Kino T, A case of epituberculosis in the adult femaleKekkaku. Tuberculosis 1994 69(9):565-69. [Google Scholar]
[6]. Reichle HS, Resolving exudates in pulmonary tuberculosis of childhoodAm J Dis Child 1933 46:969 [Google Scholar]
[7]. De Bruin M, EpituberculosisArch Dis Child 1936 11(62):65-76. [Google Scholar]
[8]. Kondo S, Miyagawa T, Ito M, Reevaluation of pathogenesis of epituberculosis in infants and children with tuberculosis, KekkakuTuberculosis 2007 82(7):569-75. [Google Scholar]
[9]. Dhingra VK, Rajpal S, Kumar R, Epituberculosis responding without change of treatment regimen: a case reportIndian J Allergy Asthma Immunol 2001 15(2):111-16. [Google Scholar]
[10]. Marais BJ, Gie RP, Schaaf HS, Hesseling AC, Obihara CC, Starke JJ, The natural history of childhood intra-thoracic tuberculosis: a critical review of literature from the pre-chemotherapy eraInt J Tuberc Lung Dis 2004 8(4):392-402. [Google Scholar]