Pulp vitality normally represents the integrity of vascular supply to the tooth. Pulp dentin complex is also richly innervated by sensory fibers, predominantly A-delta and C fibers [1,2]. Most of the vitality tests in everyday practice such as thermal tests and electric tests are dependent on the stimulation of these nerve fibers. It is more reliable to name them as pulp sensitivity tests rather than pulp vitality tests as they fail to assess the blood supply to the tooth.
Limitations of these routine vitality tests include they are subjective responses and clinical symptoms and radiographs over the time is the only method to objectively determine the pulpal status. They also give false positive and false negative response for example in traumatized teeth, necrotic teeth, patients with psychotic disorders and under the influence of drugs or alcohol. They give no information on the degree of inflammation of the pulp and its state of vascularity [3]. These inaccurate tests always lead to unnecessary endodontic procedures.
To overcome these unpleasant and unpredictable diagnostic tests, some non invasive, true vitality tests were evolved. Some of them are thermography, transmitted light photoplethysmography, laser doppler flowmetry and pulse oximetry [4-7]. Among them, pulse oximetry is one of the most reliable, non invasive diagnostic device which rely on measuring the oxygen saturation levels of arterial blood [8]. It is completely an objective test requiring no subjective responses to eliminate the bias. It consists of a probe with two light emitting diodes, one transmits red light and the other infrared light. The relationship between the pulsatile change in the absorption of red light and infrared light is assessed by pulse oximeter to measure the oxygen saturation levels of arterial blood.
Many of the studies in the literature have focused on efficacy of pulse oximetry in measuring the oxygen saturation levels of teeth in different conditions like traumatic cases, vital, non vital and teeth with open apices [9,10]. It had been proven that pulse oximetry is a significant and prompt true vitality testing device compared to conventional vitality tests. Setzer FC et al., conducted a study assessing pulp oxygen saturation levels in only posterior teeth with different pulpal inflammations which prompted us to study the effectiveness of pulse oximetry on anterior teeth with different pulpal conditions [11].
Research hypothesis of present study was to determine whether there was any significant difference in oxygen saturation levels of different pulpally inflamed anterior teeth measured by pulse oximetry.
Hence, the present study was done to diagnose different pulpal inflammation by measuring oxygen saturation levels of anterior teeth by pulse oximetry which is clinically diagnosed as RP, IP and PN.
Materials and Methods
This was a diagnostic study carried out in the Department of Conservative Dentistry and Endodontics, Narayana Dental College and Hospital, Nellore, Andhra Pradesh, India, during the time period May 2015 to June 2015. The study was approved by the Ethical Committee of Institute. Patients were selected based on the following inclusion criteria as follows, patients who are volunteered to take part in the study with age group 25-40 years, anterior teeth, patients having healthy teeth with normal pulp status, patients having an endodontically treated tooth, patients having teeth with dental caries. Exclusion criteria were as follows, patient’s teeth affected by trauma, patients with discolored teeth, periodontal problems, orthodontic braces/prosthetic crowns.
Sample size was determined using G Power 3.1.2 software with power of 0.9 and p ≤ 0.05 was considered as significant and sample size arrived as 18 per group. In order to compensate for the drop out participants, the sample size was set as 20 per group.
A total of 100 patients were recruited in the study and the patients were given informed consent forms before the commencement of the study. All the patients had been explained about the nature of procedure and the possible discomforts and risks.
Patient’s medical and dental histories was evaluated, specifically history of pain was recorded both in terms of quality and quantity.
Both cold and heat tests were performed for the test tooth. Cold test was performed by ethyl chloride spray (Icy spray, DETAX GmbH & Co, GERMANY). Tooth was isolated and dried by cotton rolls, ice spray was used by small cotton pellets and pliers. These pellets were placed on the incisal surface of the tooth. Heat test was performed by gutta-percha sticks (GC, JAPAN). After proper isolation, heated stick was placed on the incisal tooth surface for testing. Radiographs of each tooth was taken and analysed for any degeneration or resorptive process in the pulp, thickening of the periodontal ligament and for any peripaical changes. Electric pulp testing was not included in this study as it stimulates mostly C fibers. Thermal tests excite A-delta fibers which are oxygen dependent and will give more reliable interpretation of oxygen depletion in the pulp [12].
Pulpal analysis was done as per the following conditions of the test tooth [
11]
1. Healthy pulp (PC): No past history of pain, a normal cold response and any clinical or radiographic signs or symptoms.
2. Reversible Pulpitis: A pronounced response to cold, pain subsides quickly after the removal of stimuli, with causative aetiology for reversible pulpitis.
3. Irreversible Pulpitis: A past history of severe, dull, lingering, or spontaneous pain and pain could be elicited on heat
4. Pulpal Necrosis: A past history of severe, dull, lingering, or spontaneous pain; no thermal response; pain on percussion; and pain on palpation.
5. Negative control group: Root canal treated teeth with no abnormality detected in radiographs and with no response to thermal tests.
Based on above mentioned criteria, different experimental groups were categorized. All the 100 patients were included in the study with no further drop outs.
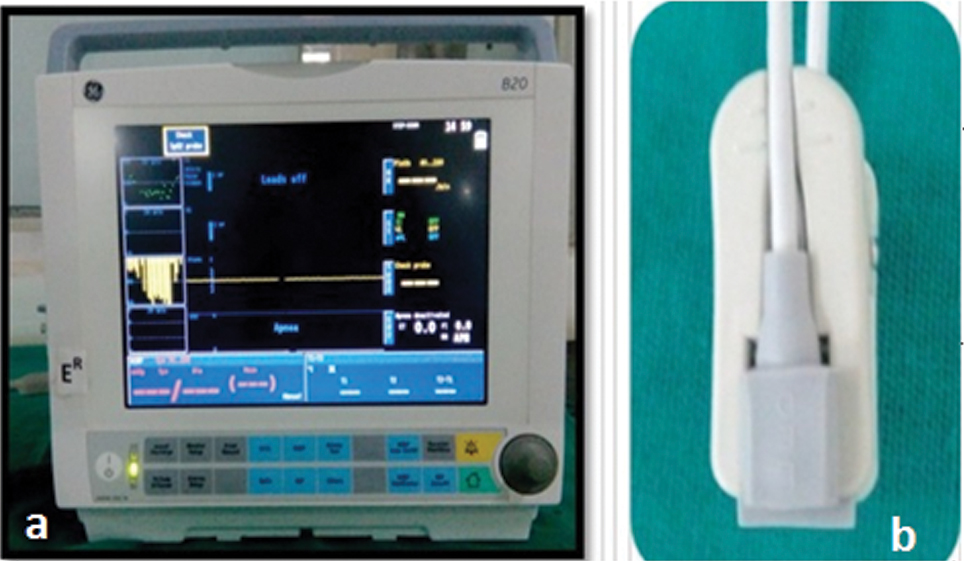
Oxygen saturation levels of all the groups were recorded by pulse oximeter monitor (GE, Finland) [Table/Fig-1a] and pulse oximeter sensor (GE, Finland) [Table/Fig-1b]. Measurements were also taken for each patient index finger to monitor the accuracy of the pulse oximetry device. Each tooth to be evaluated was isolated with cotton rolls. Light emitting diode of the sensor was placed on labial surface of anterior teeth parallel to that of receptor diode which was placed on palatal surface of same teeth. Both the diodes of sensor were confined to middle third of anterior teeth without touching adjacent soft tissues [Table/Fig-2]. Care was taken to avoid any movement during the procedure to maintain parallel alignment of two diodes throughout the procedure. As followed by Giovanella LB et al., in each patient two readings were taken, first one 30 seconds after stabilization of probe and the second one 30 minutes after first reading [13]. All the data collected were subjected to statistical analysis.
a) Pulse oximetry monitor (B20, GE, Finland); b) Pulse oximetry sensor (B20 sensor, GE, Finland).
Placement of pulse oximetry sensor on patient’s tooth.

Statistical Analysis
All the collected data were statistically analysed using software Statistical Package for Social Sciences version 21.0 (SPSS Inc, Chicago, IL)). The Pearson correlation coefficient (95% CI) was used to evaluate the correlation between two readings after 30 seconds and after 30 minutes. The Pearson coefficient analysis was done for all the five groups. Interpretation of coefficient values were done with Dancey CP and Reidy J categorization, 2004 [14]. For multiple comparisons between the groups, Analysis of variance and Tukey HSD tests were used for statistical analysis of teeth measurements with p<0.01 as the level of significance.
Results
Fifty two male and forty eight female patients participated in the study. In the experimental groups, a total of 30 maxillary central incisors, 20 maxillary lateral incisors, 10 maxillary canines, 20 mandibular central incisors, five mandibular lateral incisors and 15 mandibular canines were tested.
The oxygen saturation levels for each patient were correlated with the index finger of the patient. In all the patients, the average oxygen saturation levels of index finger were 98.4% which was more than the tested teeth.
The Pearson’s correlation coefficients (r-values) revealed that there was moderate correlation in RP, PC groups and weak correlation in IP and PN group [Table/Fig-3].
Pearson correlation coefficient between two readings at different time intervals for all the groups (r value).
| Groups | r value | p-value |
|---|
| Reversible pulpitis | 0.546 | 0.013* |
| Irreversible pulpitis | 0.345 | 0.137 |
| Pulpal necrosis | 0.193 | 0.415 |
| Positive control | 0.684 | <0.001* |
| Negative control | - | - |
r=Pearson correlation coefficient,
= Significant
Further the Analysis Of Variance test showed statistically significant difference between oxygen saturation levels in the experimental and positive and negative control groups (p<0.001).
The mean pulse oxygenation values for the three experimental and two control groups were as follows: RP: 85.45%, IP:81.6%, PN:70.7%, PC:94.6%, and NC:0%. Further the Tukey HSD test revealed that there is statistical difference between all the five groups RP, IP, PN, PC and NC (all p< .01) [Table/Fig-4].
Descriptive measures and comparison of mean SpO2 readings (%) between the groups.
| Groups | N | Mean Spo2 (%) | S.D | Between groups | Within groups |
|---|
| RP | 20 | 85.45 | 1.09 | p-value* | p-value* |
| IP | 20 | 81.60 | 0.85 | <0.001 | <0.001 |
| PN | 20 | 70.70 | 0.87 |
| PC | 20 | 94.60 | 1.95 |
| NC | 20 | 0 | 0 |
| *ANOVA test |
| (I) Pulp vitality | (J) Pulp vitality | Mean difference (I- J) | p-value* |
| RP | IPPNNCPC | 4.10 | <0.001 |
| 12.95 |
| 85.45 |
| -9.30 |
| IP | PNNCPC | 8.85 | <0.001 |
| 81.35 |
| -13.40 |
| PN | NCPC | 72.50 | <0.001 |
| -22.25 |
| NC | PC | -94.75 | <0.001 |
| * Tukey HSD post hoc test |
Discussion
In the literature, several studies were carried out by pulse oximetry on evaluating oxygen saturation levels. The oxygen saturation levels of pulp in different inflammatory conditions serve as a useful tool in diagnosing the diseases of pulp [11]. Many studies have been done for measuring the oxygen saturation levels of pulp which have been tabulated in the [Table/Fig-5] [15-18].
Outcome of previous studies on pulse oximetry in literature.
| S.NO | Author/Year/Journal | Methodology | outcome of the study |
|---|
| 1 | Calil E et al., (2008) [15] | Assessed the pulp vitality in terms of oxygen saturation levels of 32 maxillary central incisors and 32 maxillary canines and 10 root filled tooth and index finger. | No statistically significant difference between the pulse oximetry values between maxillary incisors and canines. |
| 2 | Siddheswaran V et al., (2011) [16] | Measured the pulp oxygenation rates of maxillary central incisors of 50 children and 50 adults and 20 patients with non vital anterior teeth. | Pulse oximetry has an immediate clinical value in providing baseline data of vitality of pulp in both primary and permanent tooth. |
| 3 | Setzer FC et al., (2012) [11] | Assessed the oxygenation rates of premolar and molars with clinical diagnosis of pulpal inflammation. | Determined that pulse oximetry values are significant in evaluating the different pulpal inflammation. |
| 4 | Bargrizan M et al., (2016) [17] | Measured the oxygen saturation of immature permanent teeth with closed apex and open apex. | Oxygen saturation decreases with the tooth development. |
| 5 | Kosturkov D et al., (2015) [18] | Measured the pulse oximetry readings and electric pulp tester readings on 1058 teeth in both upper and lower jaw. | Teeth with larger values of oxygenation values and electric pulp tester values are seen in larger teeth with relatively larger pulp chambers. |
| 6 | Present study | Assessment of pulp oxygen saturation levels by pulse oximetry for pulpal diseases in anterior teeth. | Significant difference in the oxygen saturation levels between different pulpally inflammed anterior teeth. |
Some of the drawbacks of pulse oximetry include it is very expensive, may give false positive responses when the sensor was not held properly with the interference of gingival oxygen levels, background absorption associated with venous blood and tissue constituents which is not differentiated.
The sensitivity and specificity of pulse oximetry in positive and negative control groups were equal to 1 in the present study. There were no false positive and false negative readings in negative control group and positive control group respectively. Sensitivity value was similar to study by Gopikrishna V et al., which was equal to 1 whereas specificity value was higher when compared to Gopikrishna V et al., which was 0.95 because author selected teeth with irreversible pulpal changes [19].
The results of the present study which showed oxygen saturation levels of RP, IP and PN groups were in consistent with the study done by Setzer FC et al., [11].
The oxygen saturation levels for each patient were correlated with the index finger of the patient. In all the patients the oxygen saturation levels of index finger were 98.4% which is more than the tested teeth, these findings were in accordance with the previous studies [11,20].
The findings of this study have shown that the oxygen saturation levels were inversely proportional to the severity of the disease. Thus, in the present study, the mean oxygen saturation levels for RP group is 85.4%, IP group is 81.6%, PN group is 70.7%. These findings were in accordance with the previous study of Setzer FC et al., where the saturation levels of different groups were as follows: RP:87.4%, IP:83.1%, PN: 74.6%, PC: 92.2% and NC:0 [11]. Decreased oxygen saturation levels for teeth with a clinical diagnosis of RP and IP are mainly by the degree of intense inflammatory processes and decrease vascularity in the pulp tissue [21].
The results of the present study vary with the study of Setzer FC et al., because of variation of study design [11]. The present study assessed the oxygen saturation levels of anterior teeth, which vary in anatomy of pulp chamber and number of roots with that of posterior teeth. Teeth with large pulp chambers had shown increased pulse oximetry values [17]. This might be the reason for variation of readings between present study and a study by Setzer FC et al., [11].
The presence of decreased levels of oxygen saturation in PN group may be due to some remnant blood flow inside the tooth [22], which could not be detected by thermal tests. This shows that diagnosing vitality of pulp rather than its sensitivity by contemporary methods prevents unnecessary endodontic invasive treatment.
As modern era of endodontics progresses towards regeneration of dental pulp, the technology of pulse oximetry can be a better objective evaluation of vitality which helps in endodontic regenerative procedures.
Limitation
Limitations of the study include design of the probe used in the study limits its usage only for anterior teeth as the sensors should conform to the size, shape and anatomy of the tooth and that the LED and photo detector be parallel to each other and should be held firmly. Hence, it needs a separate probe for posterior teeth which have different shape and contours. Findings of the study have to be correlated with more studies of larger sample size to interpolate the data to the clinical scenario.
Conclusion
It was concluded that pulse oximetry is a true vitality testing device in diagnosing different pulpal inflammatory conditions. Pulse oximetry serves in detecting the vitality of pulpally necrosed teeth which cannot be detected by thermal tests. Practice of using pulse oximetry in dental setting scenario helps to improve quality of endodontic diagnosis.
r=Pearson correlation coefficient,
*= Significant