Periodontitis is a chronic multifactorial disease which is characterized by the destruction of periodontium and loss of alveolar bone. Various modifiable and non-modifiable risk factors are associated with periodontal disease. Smoking, diabetes mellitus, microorganism, obesity, drug-induced disorders and stress are the modifiable risk factors while non-modifiable risk factors include age, gender, host response, pregnancy, genetics etc [1]. CVD is one of the foremost modifiable risk factor of periodontitis. Both periodontal disease and CVD share many common risk factors such as smoking, diabetes mellitus, age, ethnicity, sex, socioeconomic status, stress and obesity, which would possibly result in confounding any association between them [1].
A possible mechanism by which periodontitis may affect cardiovascular health is chronic oral inflammation that may lead to increased blood cholesterol levels [4].Oral bacterial infections may result in the release of proinflammatory mediators such as Interleukin-1β (IL-1β), IL-6 and Tumour Necrosis Factor alpha (TNF –α) which may get released into the systemic circulation and this may further alter fat metabolism and promote atherosclerosis by directing the activation of monocytes and alteration in the lipoproteins to a more atherogenic profile [4].
Various systemic inflammatory markers such as C- Reactive Protein (CRP), TNF-α, IL-1, IL-6, and IL-8 have been established as an inflammatory biomarkers for periodontitis and CVD [5]. Recently A2 (Lp-PLA2) has been explored as a potential biomarker for CVD. The human Lp-PLA2 is a serine-dependent, Ca2+- independent enzyme [5]. It hydrolyses oxidised phospholipids, which could lead to inflammatory cell chemotaxis, dysfunction of endothelial cell and smooth muscle cell apoptosis. It is suggested that it mayplay a direct role in the atherosclerotic disease process [6]. As Lp-PLA2 is closely associated with inflammation, it is suggested that it may influence the development and progression of periodontitis as well. Though, studies in the past have shown the association of Lp-PLA2 and CVD, however little information is available regarding the relationship between Lp-PLA2 and periodontitis, thereby contributing towards cardiovascular events [2,3]. Hence, the aim of the present study was to evaluate the periodontal status, serum lipid profile and Lp-PLA2 serum levels in systemically healthy CP subjects and compare them with healthy controls.
Materials and Methods
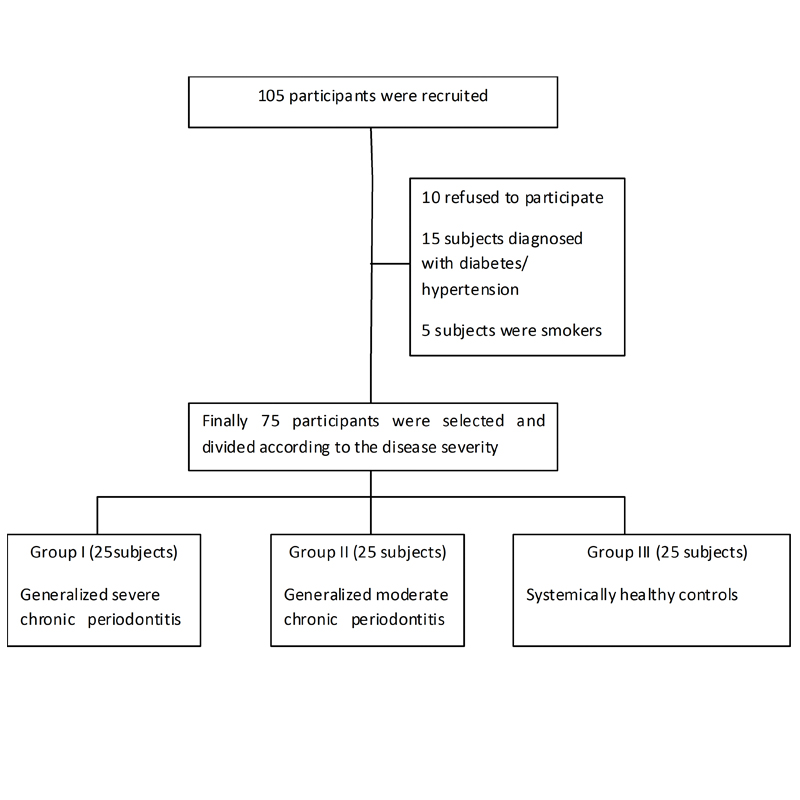
In this cross-sectional study, a total of 105 subjects were recruited from Department of Periodontology, Meenakshi Ammal Dental College and Hospital, Chennai, Tamil Nadu, India, for the present study. Out of these, 10 subjects refused to participate in the study, 15 subjects were excluded as they were diagnosed with diabetes and hypertension. Five subjects were smokers, hence were also excluded from the present investigation. Finally, 75 participants were selected based on the inclusion and exclusion criteria and were divided into three groups. The power of the study was calculated which came out to be 90%. The groups consisted of Group I- systemically healthy subjects with generalized severe CP, Group II- systemically healthy with moderate CP and Group III- systemically and periodontally healthy volunteers who served as controls [Table/Fig-1]. The “Institutional Ethics Committee” and “Institutional Review Board”- MAHER University [MADC/IRB-IX/2016/193], Chennai, approved the study following the Declarations of Helsinki [7]. The study was conducted from February 2nd 2015 to 26th November 2015 (Clinical trials.gov identifier: NCT03041480). The written informed consent was obtained from all participants enrolled in the current investigation.
Flow chart of study population.
The inclusion criteria included the subjects with (i) age ≥ 35 years and (ii) presence of at least 24 teeth (iii) CAL ≥ 5 mm in more than 30% of sites in Group I (iv) CAL between 3 mm-4 mm in more than 30% of sites in Group II [8] (v) healthy and intact periodontium in Group III. The exclusion criteria included (i) presence of any systemic disease or conditions that could affect periodontal tissues. e.g. diabetes mellitus, CVD, liver diseases, metabolic syndrome or other endocrine diseases (ii) history of periodontal treatment in past six months (iii) smoking and alcoholism (iv) anomalies of blood and immune system such as anaemia andleukaemia (v) systemic medication or antibiotic treatment for the previous six months. (vi) pregnant females.
Demographic Variables
A brief case history was taken, which included patient’s chief complaint, medical and dental history. Demographic data such as age, gender, income, height, weight and Body Mass Index (BMI) were recorded. BMI was calculated according to the formula [9]:
BMI = Body mass (kg)/Body height (m2)
Clinical Data Collection
All subjects were seated comfortably in an upright position and underwent a full-mouth periodontal examination. The periodontal examination included probing of six sites (distofacial, facial, mesiofacial, distolingual, lingual and mesiolingual) per tooth (third molars excluded), using a Williams periodontal probe by a calibrated examiner. The following periodontal parameters were recorded (i) PI [10] BOP four sites (distofacial, facial, mesiofacial and lingual) per tooth were assessed, with a positive score if bleeding occurred on probing [11] (iii) PD, was recorded as the distance from the free gingival margin to the base of pocket, at the nearest mm. (iv) CAL, was measured as the distance from the cemento-enamel junction to the base of the pocket, at the nearest mm.
Sample Collection
In order to estimate the fasting blood sugar levels, all the subjects were asked to fast 8-10 hours before collecting the blood in the morning. This was done to rule out the diabetes mellitus. Blood samples (5 ml) were then collected by venepuncture of the cubital vein in the anticubital fossa by using a 5 ml disposable syringe and 23 gauge needle. It was then collected in sterile vacutainer tubes with no added anticoagulant. From the collected blood samples, serum was separated and transferred into 2 ml vial and stored at 20°C- 80°C for later analysis. TC, TG and High-Density Lipoprotein Cholesterol (HDL-c) were measured by enzymatic assay using the SL-150 UV spectrometer. The results were expressed in mmol/. Low-Density Lipoprotein Cholesterol (LDL-c) was calculated using Friedewald’s formula [9]:
LDL-c = TC – [HDL-c + (TG/5)].
Serum level of Lp-PLA2 was determined using a commercially available ELISA kit (Bio Assay Technology Laboratory, China) according to Cia A et al [12].
Statistical Analysis
The collected data was analysed with IBM.SPSS statistics software 23.0 version. One-way ANOVA was used to compare the difference of the mean demographic values and level of significance was calculated. Chisquare test was used to calculate the gender distribution within the study group [Table/Fig-2]. Mean and standard deviation was calculated to compare the lipid profile and Lp-PLA2 levels in all the subject groups. Pearson correlation coefficient was calculated to assess the relationship between the lipid profile and Lp-PLA2 levels in each study group. In order to find the multivariate analyses of the lipid profile and Lp-PLA2, Tukey’s Post hoc test was done. The probability value of 0.05 was considered as significant.
Gender distribution among the Group I, Group II and Group III.
| GROUP | Female n (%) | Male n (%) | χ2-value | p-value |
|---|
| I | 11 (44%) | 14 (56%) | 0.325 | 0.85 (NS) |
| II | 12 (48%) | 13 (52%) |
| III | 10 (40%) | 15 (60%) |
Results
Demographic variables in all the groups: The mean age was more or less similar in all the groups, However, it was found to be a little higher in CP patients which was significant. Weight, height and BMI was found to be high in the healthy controls. Monthly income and gender were similar in all the groups and hence was found to be non-significant [Table/Fig-3].
Demographic variables in different groups of study population.
| Demographic parameters | Mean ± Std. deviation | p-value |
|---|
| Group I | Group II | Group III |
|---|
| Age (years) | 41.08 ± 7.19 | 43.4 ± 7.97 | 37 ± 4.42 | 0.004** |
| Height (m) | 1.61 ± 6.35 | 1.66 ± 7.2 | 1.64 ± 8.12 | 0.042** |
| Weight (kg) | 59.6 ± 8.68 | 66.56 ± 9.69 | 66.16 ± 12.49 | 0.035** |
| BMI (kg/m2) | 22.27 ± 2.44 | 23.76 ± 2.18 | 24.3 ± 3.3 | 0.027** |
| Income (Rs) | 10220± 3382.18 | 11260 ± 5206.4 | 11180± 4339.45 | 0.65 (NS) |
| Gender distribution |
| Group | Female n (%) | Male n (%) | χ2-value | p-value |
| I | 11 (44%) | 14 (56%) | 0.325 | 0.85 (NS) |
| II | 12 (48%) | 13 (52%) |
| III | 10 (40%) | 15 (60%) |
Correlation of clinical parameters with Lp-PLA2 and lipid profile in different groups: When the clinical parameters (PI, BOP, PD, CAL), lipid profile (TC, TG, HDL, LDL and VLDL) and Lp-PLA2 were compared, no significant correlation was found between the variables in Group I [Table/Fig-4]. However, a statistically significant correlation was found between PI and LDL in Group II [Table/Fig-5]. PI was significantly correlated with LDL and HDL, and BOP was again correlated with TG and VLDL in Group III which was found to be statistically significant [Table/Fig-6].
Pearson correlation of clinical parameters with Lp-PLA2 and lipid profile in Group I.
| Clinical parameters | TC | TG | HDL | Lp-PLA2 | LDL | VLDL |
|---|
| PI | Pearson correlation | -0.067 | -0.124 | -0.109 | -0.129 | -0.022 | 0.199 |
| Sig. (2-tailed) p-value | 0.750 (NS) | 0.555 (NS) | 0.604 (NS) | 0.540 (NS) | 0.918 (NS) | 0.314 (NS) |
| BOP | Pearson correlation | 0.160 | -0.169 | -0.042 | -0.094 | 0.151 | -0.043 |
| Sig. (2-tailed) p-value | 0.445 (NS) | 0.419 (NS) | 0.843 (NS) | 0.654 (NS) | 0.470 (NS) | 0.838 (NS) |
| PD | Pearson correlation | 0.219 | 0.095 | 0.089 | 0.058 | 0.152 | -0.202 |
| Sig. (2-tailed) p-value | 0.293 (NS) | 0.650 (NS) | 0.672 (NS) | 0.781 (NS) | 0.468 (NS) | 0.333 (NS) |
| CAL | Pearson correlation | 0.177 | 0.008 | 0.018 | 0.127 | 0.139 | -0.072 |
| Sig. (2-tailed) p-value | 0.398 (NS) | 0.970 (NS) | 0.933 (NS) | 0.547 (NS) | 0.507 (NS) | 0.733 (NS) |
Pearson correlation of clinical parameters with Lp-PLA2 and lipid profile in Group II.
| Clinical parameters | TC | TG | HDL | Lp-PLA2 | LDL | VLDL |
|---|
| PI | Pearson correlation | -0.307 | 0.156 | 0.140 | 0.088 | -0.444 | 0.126 |
| Sig. (2-tailed) p-value | 0.136 (NS) | 0.457 (NS) | 0.505 (NS) | 0.674 (NS) | 0.026* | 0.547 (NS) |
| BOP | Pearson correlation | -0.224 | -0.052 | 0.056 | 0.073 | -0.277 | -0.051 |
| Sig. (2-tailed) p-value | 0.282 (NS) | 0.804 (NS) | 0.791 (NS) | 0.730 (NS) | 0.180 (NS) | 0.838 (NS) |
| PD | Pearson correlation | -0.039 | 0.066 | 0.146 | -0.096 | -0.136 | 0.067 |
| Sig. (2-tailed) p-value | 0.853 (NS) | 0.754 (NS) | 0.487 (NS) | 0.647 (NS) | 0.515 (NS) | 0.750 (NS) |
| CAL | Pearson correlation | 0.297 | -0.176 | 0.163 | -0.042 | 0.268 | -0.165 |
| Sig. (2-tailed) p-value | 0.149 (NS) | 0.399 (NS) | 0.437 (NS) | 0.842 (NS) | 0.195 (NS) | 0.429 (NS) |
Pearson correlation of clinical parameters with Lp-PLA2 and lipid profile in Group III.
| Clinical parameters | TC | TG | HDL | Lp-PLA2 | LDL | VLDL |
|---|
| PI | Pearson correlation | -0.153 | 0.272 | 0.397 | -0.219 | -0.401 | 0.267 |
| Sig. (2-tailed) p-value | 0.465 (NS) | 0.188 (NS) | 0.049* | 0.292 (NS) | 0.047* | 0.197 (NS) |
| BOP | Pearson correlation | 0.139 | 0.473 | 0.214 | -0.077 | -0.108 | 0.471 |
| Sig. (2-tailed) p-value | 0.508 (NS) | 0.017* | 0.304 (NS) | 0.716 (NS) | 0.606 (NS) | 0.017* |
| PD | Pearson correlation | 0.365 | -0.018 | -0.003 | -0.003 | 0.246 | -0.030 |
| Sig. (2-tailed) p-value | 0.073 (NS) | 0.933 (NS) | 0.989 (NS) | 0.989 (NS) | 0.237 (NS) | 0.888 (NS) |
| CAL | Pearson correlation | 0.365 | -0.018 | -0.003 | -0.003 | 0.246 | -0.030 |
| Sig. (2-tailed) p-value | 0.073 (NS) | 0.933 (NS) | 0.989 (NS) | 0.989 (NS) | 0.237 (NS) | 0.888 (NS) |
Comparison of Lp-PLA2 and the lipid levels among the groups: In all the groups, Lp-PLA2 was found to be statistically significant. TG was also found to be statistically significant when compared among Group I and Group II. Similarly, when mean VLDL was compared among Group I and Group II, it was found to be statistically highly significant. Also, when Group II and Group III were compared for VLDL, it was found to be significant. TC and LDL levels were found to be higher in Group I when compared to the other groups but were statistically non significant [Table/Fig-7].
The Lp-PLA2 and lipid levels in different groups.
| Biochemical parameters | Group I | Group II | Group III | Comparison between Group I and II (p-value) | Comparison between Group II and control (p-value) | Comparison between Group I and control (p-value) |
|---|
| Lp-PLA2 μg/l) | 59.75 ± 10.68 | 28.74 ± 5.020 | 12.66 ± 3.54 | 0.000** | 0.000** | 0.000** |
| TC (mmol/l) | 185.56 ± 24.39 | 178.56 ± 27.82 | 175.48 ± 31.91 | 0.656 (NS) | 0.421 (NS) | 0.921 (NS) |
| TG (mmol/l) | 129.88 ± 17.37 | 113.28 ± 18.08 | 120.48 ± 27.90 | 0.023* | 0.281 (NS) | 0.472 (NS) |
| HDL (mmol/l) | 51.16 ± 14.71 | 51.48 ± 13.94 | 64.68 ± 32.88 | 0.999 (NS) | 0.088 (NS) | 0.099 (NS) |
| LDL (mmol/l) | 107.32 ± 30.73 | 104.36 ± 24.63 | 86.68 ± 48.46 | 0.955 (NS) | 0.114 (NS) | 0.200 (NS) |
| VLDL (mmol/l) | 27.08 ± 3.2 | 22.72± 3.66 | 24.12 ± 5.61 | 0.002** | 0.045* | 0.485 (NS) |
Discussion
Periodontal disease occurs as a consequence of mixed microbial infections within which definite groups of pathogenic bacteria coexist that follows an inflammatory host response secondary to infection [13]. On the other hand, CVD is the most prevalent disorder responsible for high morbidity and mortality among individuals [14]. Several studies suggest that CVD is associated with increased risk of periodontitis [15,17].
To identify individuals who are at high risk of inflammation, new diagnostic tests have been developed. Several inflammatory markers such as high-sensitivity CRP (hs-CRP) and white blood cells, have been studied as predictors of future cardiovascular events [18].
Lp-PLA2, also known as platelet-activating factor acetylhydrolase, is an enzyme that hydrolyses oxidized phospholipids and is largely associated with LDL. Recent evidence suggests that Lp-PLA 2is an independent cardiovascular risk factor and an addictive risk factor for cardiovascular mortality [19].
To the best of our knowledge, only very few studies have been reported on the relationship between Lp-PLA2 and periodontitis worldwide [5,9,20]. This is the first study to evaluate the level of Lp-PLA2 in CD among South Indian population thereby contributing towards CVD.
The demographic variables such as age, height, weight and BMI was found to be statistically significant. The mean age in Group I and Group II was higher when compared to Group III [Table/Fig-2]. This was in accordance with Zhou SY et al., [9] and Faddy MJ et al.,[21], where mean age was higher in both CD subjects with and without hyperlipidaemia when compared to periodontally healthy individuals. It is suggested that the risk of being affected by periodontitis is 2.3 times more for persons above 35 years of age [22]. Hence, age can be considered as another non-modifiable risk factor for both periodontal and CVD.
According to WHO classification, BMI was calculated based on height and weight [23]. Though, these values were under normal BMI range, still they were found to be statistically significant (p=0.027). The mean BMI in Group III was higher when compared to Group I and Group II [Table/Fig-2]. This may be due to better periodontal health in Group III when compared to the other groups. This is in accordance with Hu HY et al., who found a significant positive correlation of BMI with all-cause mortality in underweight patients [24]. In our study, the lower BMI in Group I may be due to impaired mastication leading to improper intake of nutritious diet because of severe periodontitis. A low BMI can prevent normal eating in some cases on the basis of there being real functional difficulties [25].
The mean income in Group I, Group II and Group III was found to be similar [Table/Fig-2]. Gundala R and Chava VK found a positive association between higher socioeconomic groups and better periodontal health [26]. In our study, the mean income for all the groups was found to be similar, hence there was no difference among the groups.
The gender distribution was not significant among the different groups [Table/Fig-2]. This was in accordance with the study done by Zhuo SY et al.,[9] and Taleghani F and Shamaei M [27] where there was no significant difference in gender among CP subjects with and without hyperlipidaemia and periodontally healthy subjects. However, in our study, the reason may be because the ratio of male and female in all the groups was more or less similar.
Lipids are significant structural and bioregulatory constituents of human cells and plasma lipoproteins. The major blood lipid plasma concentration is determined by the regulation mechanism of their cell synthesis and by intricate metabolic response within their transportation pathway in the body. In periodontal disease, Gram negative infections produces systemic inflammation and have been associated in the development of hyperlipidaemia, which is an important risk factor for development of CVD. According to Katz J et al., hypercholesterolemia and cardiovascular diseases are related to periodontal disease [28].
When periodontal parameters were compared with lipid and Lp-PLA2, no significant correlation was found between the periodontal parameters such as PI, BOP, PD, CAL, lipid profile and Lp-PLA2 in Group I [Table/Fig-3]. This was in accordance with the study done by Morita M et al., who also found that the TC and LDL were not statistically significant in periodontal cases when compared to periodontally healthy subjects [29]. In Group II, only PI showed a positive correlation with LDL [Table/Fig-4]. This was in concordance with the study done by Fentoglu O et al., who reported the mean PI to be positively correlated with LDL in CP subjects with hyperlipidemia when compared to healthy controls [30]. In Group III, PI showed a significant correlation with HDL and LDL. With the reduction in PI, high levels of HDL and low levelsof LDL were found [Table/Fig-5]. It is stated that HDL neutralizes Lipopolysaccharides (LPS) in the circulation and prevents LDL oxidation, as well as antagonizes cholesterol transport, because it accepts cholesterol from the cell membrane during elimination, hence it is considered anti-atherogenic [30]. High density lipoprotein cholesterol is esterified in the blood circulation and it is directly transported to the liver via LDL for excretion. Thus, a failure in cholesterol elimination by HDL route might lead to early atherosclerosis type lesions in blood vessels [30].
BOP is an important criterion to diagnose gingival inflammation. In our study, BOP was significantly correlated with TG and VLDL in Group III [Table/Fig-5]. Despite of lower BOP score in periodontally healthy subjects (Group III), increase in TG and VLDL was seen. This may be due to intake of fat rich diet and increase in BMI which was seen in Group III when compared to Group I and Group II with compromised periodontium. In our study, BOP did not show any correlation with the lipid profile in periodontitis subjects (Group I and Group II). Overall no significant correlation was found between the clinical parameters such as BOP, PD, CAL with Lp-PLA2 and lipid profile in periodontitis subjects when compared with periodontally healthy subjects. The disagreement observed in the study may be due to the great number of variables involved such as eating, physical activity habits, obesity, age, socioeconomic conditions and stress, as these are environmental factors in which the individual survive, and hence may interfere with the study results, as these are the situations that are difficult to control.
Lp-PLA2 is regarded as one of the most important biomarker for predicting atherosclerosis risk [31,32]. Clinical studies have reported that plasma Lp-PLA2 activity is strongly associated with atherogenic lipids and vascular risk [17, 18]. Dohi J et al., [33], Blake GT et al., [34] and Pruzanski W et al.,[35] stated that acute inflammation increases the LDL content of Lp-PLA2. These observations led to the hypothesis that Lp-PLA2 activity levels could be used as biomarkers of periodontal disease and that inhibition of the activity could lower the inflammation and offer an attractive therapeutic strategy [17].
In our study, Lp-PLA2 was significantly correlated among the study groups [Table/Fig-6]. When comparison was done among all the three groups, Lp-PLA2 was found to be significantly higher in severe and moderate CP than healthy controls. This was in concordance with the study done by Zhou SY et al.,[9] and Losche W et al., [20] who stated that the level of Lp-PLA2 was significantly higher in CD group when compared with periodontally healthy subjects. Losche W et al., also reported that periodontitis led to increase in the plasma Lp-PLA2 [20]. All these studies indicated that CP could increase the level of Lp-PLA2. It is demonstrated that periodontal infection could lead to systemic inflammation which consequently increase the level of Lp-PLA2 [9]. In future, Lp-PLA2 may be considered as an important biomarker in periodontal disease owing toits pathogenesis such as synthesis, attaching to circulating lipoproteins, and some amount remaining free in the circulation.
In our study, we also compared the TC, TG, LDL, HDL and VLDL among the groups. The results showed that the mean levels of TC, HDL and LDL in individuals with periodontitis were higher than those of individuals without periodontitis but were not statistically significant [Table/Fig-7]. This was in accordance with the study done by Ana CP et al. who reported higher levels of TC (192.1 mg/dl ± 40.9) and TG (153.5 mg/dl ± 105.6) in periodontitis subjectswhen compared to healthy controls (186.1 mg/dl ± 35.4 and 117.5 mg/dl ± 68, respectively) and was found to be non-significant [36]. In our study, the level of TG was higher in the severe CP when compared to moderate CP and was found to be significant. This was in accordance with the previous studies done by Taleghani F et al.,[27], Taghavi AM et al.,[37], Morita M et al.,[29] and Cutler CW et al.,[38] who reported an increase in TG levels in subjects with CP subjects. Also, the mean VLDL was found to be highly significant when Group I was compared with Group II and significant when Group II was compared with Group III. In accordance with our study, Kundu M et al., reported VLDL to be significantly higher (p<0.05) in CP when compared to healthy controls [39]. Higher mean HDL-C level was reported by Morita et al., in the healthy group, compared to the diseased group, howeverit was found to be non-significant [29]. This was in accordance with our study where we also found a higher level of HDL in control than diseased group (Group I and Group II), though clinically it was non-significant.
We found Lp-PLA2 and lipid profile levels much higher in periodontitis subjects than healthy controls. Considering the above scenario, periodontal treatment might be a possible way to reduce the risk of CVD for CP subjects. This might provide a mechanism for reducing the cardiovascular risk in CP patients through periodontal treatment.
Limitation
The limitation of this study was that intervention by undergoing scaling and root planning could have been done in CP patients thereby evaluating the level of Lp-PLA2 after treatment. In future, long term interventional studies are required to elucidate the effect of Lp-PLA2 on periodontitis and CVD.
Conclusion
From the results of the present study, it is inferred that Lp-PLA2, TG and VLDL already being a predictor biomarker for atherosclerotic disease can also be an inflammatory marker for periodontitis. This association might provide a mechanism for reducing the risk of CVD in CP patients through periodontal treatment. A combination of periodontal treatment and lipid-lowering therapy may lead to beneficial effects on the atherogenic lipid profile thereby reducing the risk of developing CVD.