A Diagnostic Surprise For A Right Iliac Fossa Mass – A Perforated Ileal Gastrointestinal Stromal Tumour
J Sanjay Prakash1, Anita Samraj2, G Sabarish Kumar3, R Vijai4
1 Assistant Professor, Department of General Surgery, Saveetha Medical College and Hospital, Chennai, Tamil Nadu, India.
2 Professor, Department of General Surgery, Saveetha Medical College and Hospital, Chennai, Tamil Nadu, India.
3 Senior Resident, Department of General Surgery, Saveetha Medical College and Hospital, Chennai, Tamil Nadu, India.
4 Postgraduate Student, Department of General Surgery, Saveetha Medical College and Hospital, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. J. Sanjay Prakash, 7/21, Sri Labdhi Colony, T.T.K Road, Alwarpet, Chennai-600018, Tamil Nadu, India.
E-mail: sanprinarch@gmail.com
Gastrointestinal Stromal Tumours (GISTs) are tumours of the gut found mostly in stomach and small intestine. The complications are Gastrointestinal (GI) bleeding, obstruction, pain and rarely perforation. We are reporting an abnormal presentation of GIST masquerading as an acute abdomen with Right Iliac Fossa (RIF) mass in 60-year-old lady. Contrast Enhanced Computed Tomography (CECT) of abdomen revealed a peripherally enhancing encapsulated abscess in RIF in close contact with base of caecum and adjacent peritonitis suggesting caecal perforation. On laparotomy, a gangrenous perforated ileal GIST was identified along the antimesenteric border of ileum. Pathological examination confirmed the tumour to be a GIST of spindle cell type, further reiterated by immunohistochemistry. Our case report emphasizes, GIST as a rare and unusual differential diagnosis of RIF mass, and to have high degree of clinical suspicion when a similar situation is encountered in an emergency scenario, keeping in mind the poor outcome due to delay in appropriate management of the disease.
Haematochezia, Intestinal perforation, Laparotomy, Terminal ileum
Case Report
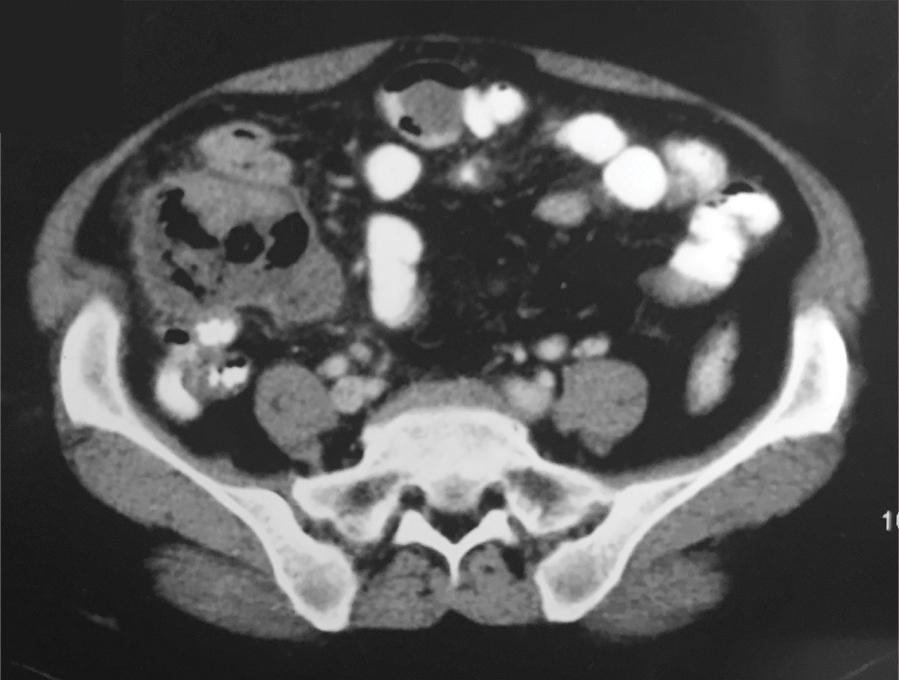
A 60-year-old female presented to the Emergency room with complaints of diffuse lower abdominal pain for one day duration with three episodes of haematochezia over eight hours duration. On examination, she had pallor and tachycardia. On clinical examination of abdomen, there was tenderness, mild guarding, rebound tenderness and an ill defined mass in the right iliac fossa. On rectal examination, blood staining of digit was present. The laboratory tests showed haemoglobin of 8 gm% and leukocytosis 16000 cells/mm3. Chest and abdomen X-rays were normal. Ultrasound abdomen reported an ill defined mass in RIF with minimal free fluid and probe tenderness. CECT of abdomen demonstrated a peripheral enhancing, encapsulated abscess in RIF, in close contact with base of caecum and adjacent peritoneal inflammation, suggesting a sealed caecal perforation [Table/Fig-1].
CECT abdomen showing an encapsulated abscess in RIF in close contact with the base of caecum with adjacent peritoneal inflammation.
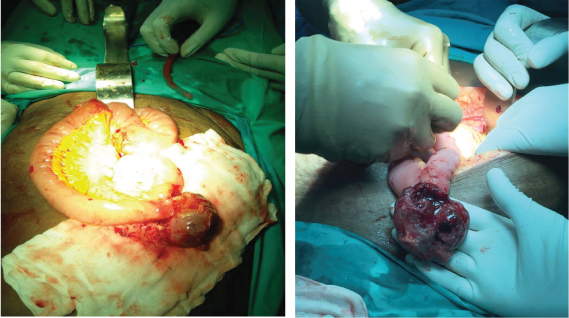
Operative findings: She underwent an emergency exploratory laparotomy which revealed a part of the small bowel and omentum adherent to the caecum and adjacent abdominal wall. Slow separation and blunt dissection of the structures revealed a gangrenous, perforated small bowel tumour of maximum diameter 6 cm-8 cm at the antimesenteric border of the ileum nearly, 80 cm proximal to the ileocecal junction [Table/Fig-2,3]. Rest of the abdomen was normal. She underwent segmental resection of ileum with part of the mesentery and primary anastomosis. The peritoneal cavity was irrigated with copious amount of normal saline and abdomen was closed in layers.
A perforated and gangrenous GIST at the antimesenteric border of ileum.
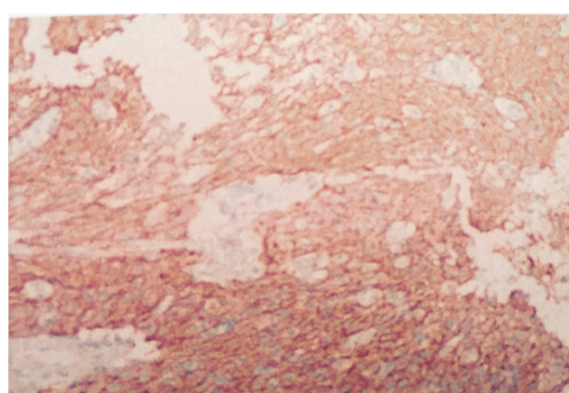
Pathological findings: Pathological examination revealed a 6 cm x 5 cm x 3 cm submucosal mass extending into the antimesenteric border of ileum. Microscopy revealed a low grade, intermediate risk, pT3 pNx GIST of spindle cell type. Immunohistochemistry was positive for CD117 confirming the diagnosis of GIST [Table/Fig-4].
Immunohistochemical staining(IHC 400X) positive for CD117 (c-Kit).
Postoperative course: Her postoperative course was uneventful. She was discharged on the tenth postoperative day after suture removal. She was started on adjuvant imatinib therapy to prevent tumour recurrence.
Discussion
GIST are tumours of mesenchymal origin that arise from interstitial cells of Cajal in GIT. They constitute 0.1%-3% of all Gastrointestinal Tract (GIT) tumors [1]. GISTs typically occur in the elderly around the sixth decade of life [2]. They can occur anywhere in the GIT but mostly observed in the stomach (50%) and small intestine (25%). GISTs generally have an indolent course and are diagnosed incidentally. Small sized tumours remain silent while large sized tumours present as large abdominal masses with clinical features unrelated to the disease, so most metastasize at the time of presentation [2,3]. The complications are GI bleeding (40%), intestinal obstruction, abdominal pain and very rarely perforation [2].
GIST as a content of Meckel’s diverticulum has been reported in seven cases [4] and as abdominal cocoon in a single case [5]. Most common complication of GIST is bleeding [2] but they have also presented rarely as perforation which has been documented in seven cases [6]. There are only two documented cases till now of GIST presenting as RIF mass, one a jejunal GIST masquerading as an appendicular mass [7] and another a cecal GIST presenting as a diffuse swelling in RIF and right lumbar regions [8]. In our case, a perforated terminal ileal GIST presented as a RIF mass with lower GI bleed. This combination of presentation is yet to be reported.
The pathological diagnosis is based on the histological profile of the tumour and immunohistochemical (IHC) staining is required to confirm the diagnosis [9]. The following table shows the IHC staining pattern of GIST [Table/Fig-5] [2,5,10-13].
Positivity rates for various immunohistochemical markers in GIST.
| Marker | Positivity (%) |
|---|
| CD 117 | 94-98 |
| CD 34 | 60-80 |
| SMA | 20-30 |
| S100 | 10 |
| Desmin | <5 |
Recently identified, antibody against DOG1 (discovered on GIST) was reported to be positive in 85%-95% of CD117-positive GISTs and in 30%-36% of CD117–negative GISTs. However, it cannot differentiate between KIT/PDGFRA mutant and wild-type GIST. Hence, DOG1 immunostaining may be helpful to identify tumours which cannot be diagnosed based on c-Kit immunohistochemistry [11].
Fletcher CD et al., proposed a classification system to prognosticate GIST and has been widely accepted and followed today [Table/Fig-6] [14]. The mitotic count is the most vital prognostic factor [10,12].
Classification system by Fletcher et al.
| Risk of malignancy | Size of tumour (cm) | Mitotic counts (/50HPF) |
|---|
| Very low | <2 | <5 / 50 |
| Low | 2–5 | <5 |
| Intermediate | <5 | 6– 10 |
| 5 – 10 | <5 |
| High | >5 | >5 |
| > 10 | Any counts |
| Any size | >10 |
The preferred treatment of choice for GISTs is R0 surgical excision. A lymphadenectomy is usually not performed, as metastasis to lymph nodes is extremely rare. Patients with perforation have a five-year survival rate of only 24%, in contrast to patients with localized or locally advanced tumours where the five-year survival rate is 46%. The reason for this difference may be attributed to peritoneal dissemination [13]. Imatinib, a selective tyrosine kinase inhibitor therapy which has significantly improved the overall survival in patients with advanced disease. Adjuvant therapy should be considered for four years, in patients undergoing R0 resection for primary disease and perforation as well [15].
Conclusion
We presented this case of an acute abdomen with a RIF mass that was incidentally diagnosed to be a perforated GIST arising from the ileum. Apart from the usual causes of RIF mass, a perforated GIST of this kind should also be considered when older patients present with such clinical features. A high degree of clinical suspicion and prompt management is required in view of the high morbidity rates from delayed diagnosis of this disease.
[1]. Connolly EM, Gaffney E, Reynolds JV, Gastrointestinal stromal tumoursBr J Surg 2003 90(10):1178-86. [Google Scholar]
[2]. Miyata S, Bliss DW, A gastrointestinal stromal tumor found in perforated Meckel’s diverticulumSurg case reports. Springer 2016 2(1):67 [Google Scholar]
[3]. DeMatteo RP, Lewis JJ, Leung D, Mudan SS, Woodruff JM, Brennan MF, Two hundred gastrointestinal stromal tumors: recurrence patterns and prognostic factors for survivalAnn Surg 2000 231(1):51-58. [Google Scholar]
[4]. López-Tomassetti Fernández EM, Hernández Hernández JR, Nuñez Jorge V, Usha M, Perforated gastrointestinal stromal tumor in Meckel’s diverticulum treated laparoscopicallyAsian J Endosc Surg 2013 6(2):126-129. [Google Scholar]
[5]. Kumar V, Rau RA, Kamath S, Perforated GIST in Jejunum - A Rare Cause of Abdominal CocoonJ Clin Diagn Res 2014 8:132-133. [Google Scholar]
[6]. Skipworth J, Fanshawe A, West M, Al-Bahrani A, Perforation as a rare presentation of gastric gastrointestinal stromal tumours: a case report and review of the literatureAnn R Coll Surg Engl 2014 96(1):01-05. [Google Scholar]
[7]. Nancharaiah P, Venkateswarlu MC, Aishwarya M, Gist in Rif masquerading as appendicular massIOSR J Dent Med Sci 2016 15:2279-2861. [Google Scholar]
[8]. Sreevathsa MR, Caecal gastrointestinal stromal tumor with perforation and obstructionIndian J Surg Oncol. Springer 2012 3(4):311-313. [Google Scholar]
[9]. Grover S, Ashley SW, Raut CP, Small intestine gastrointestinal stromal tumorsCurr Opin Gastroenterol 2012 28:113-23. [Google Scholar]
[10]. Judson I, Gastrointestinal stromal tumours (GIST): biology and treatmentAnn Oncol 2002 13(Suppl 4):287-89. [Google Scholar]
[11]. Bucher P, Taylor S, Villiger P, Morel P, Brundler MA, Are there any prognostic factors for small intestinal stromal tumors?Am J Surg 2004 187:761-66. [Google Scholar]
[12]. Liegl B, Hornick JL, Corless CL, Fletcher CD, Monoclonal antibody DOG1.1 shows higher sensitivity than kit in the diagnosis of gastrointestinal stromal tumors, including unusual subtypesAm J Surg Pathol 2009 33:437-46. [Google Scholar]
[13]. Crosby JA, Catton CN, Davis A, Couture J, O’Sullivan B, Kandel R, Malignant gastrointestinal stromal tumors of the small intestine: a review of 50 cases from a prospective databaseAnn Surg Oncol 2001 8(1):50-59. [Google Scholar]
[14]. Fletcher CD, Berman JJ, Corless C, Gorstein F, Lasota J, Longley BJ, Diagnosis of gastrointestinal stromal tumors: A consensus approachHum Pathol 2002 33(5):459-465. [Google Scholar]
[15]. Koo DH, Ryu MH, Kim KM, Yang HK, Sawaki A, Hirota S, Asian Consensus Guidelines for the Diagnosis and Management of Gastrointestinal Stromal TumorCancer Res Treat 2016 48(4):1155-66. [Google Scholar]