Testicular and Epididymal Metastasis from Prostate Carcinoma: A Rare Manifestation of Common Disease
Jayesh Mittal1, L. N. Dorairajan2, R. Manikandan3, Bhawanan A. Bade4, Amit Mishra5
1 Senior Resident, Department of Urology, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, India.
2 Professor and Head, Department of Urology, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, India.
3 Associate Professor, Department of Urology, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, India.
4 Professor and Head, Department of Pathology, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, India.
5 Senior Resident, Department of Urology, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Jayesh Mittal, Senior Resident, Department of Urology, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry-605006, India.
E-mail: dr_mittaljayesh@yahoo.co.in
Carcinoma prostate secondary metastasis to testicle and epididymis is rare. We report a case of metastatic carcinoma prostate in which testicular and epididymal metastasis were diagnosed incidentally in bilateral orchiectomy specimen. Testicular and para testicular structure should be properly evaluated for accurate staging of carcinoma prostate. Epididymis should always be included in bilateral orchidectomy specimen.
Epididymis, Prostate cancer, Testis
Case Report
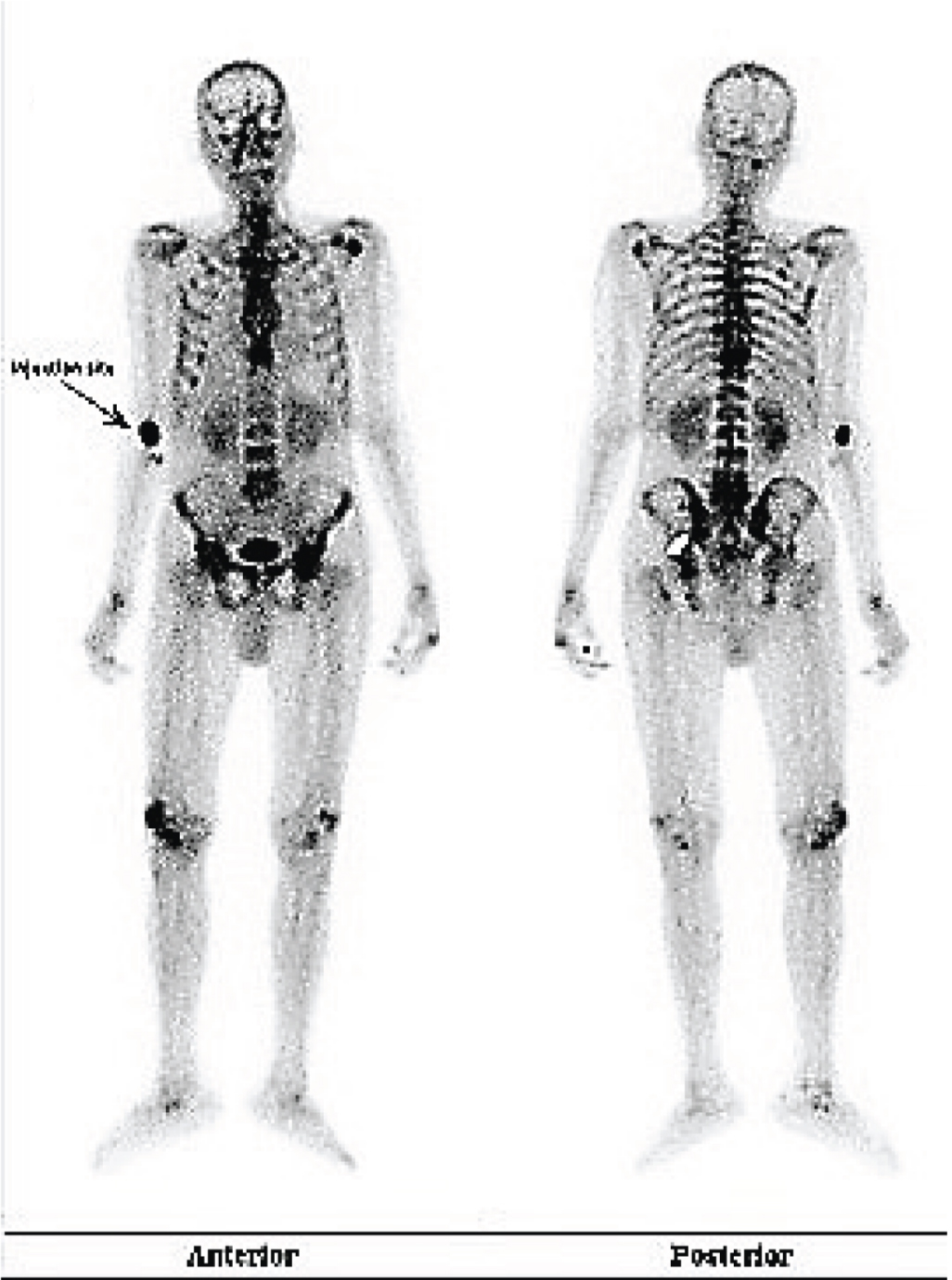
A 75-year-old man presented with lower urinary tract symptoms for three months and oliguria for last 15 days. There were no other complains. Clinical examination revealed normal genitalia with bilateral minimal hydrocele and a hard nodular prostate with fixed rectal mucosa. Transperineal transrectal ultrasound guided core needle biopsy was reported as adenocarcinoma with Gleason score of 5 + 3. His Prostate Specific Antigen (PSA) was >100 ng/ml. Bone scan revealed multiple skeletal metastasis [Table/Fig-1].
Bone scan images showing multiple sites skeletal metastasis.
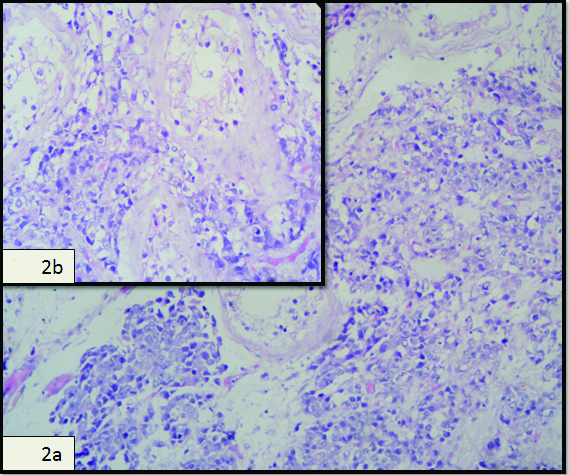
Ultrasound examination of the abdomen and pelvis showed bilateral hydroureteronephrosis. Bilateral orchiectomy was performed to achieve hormonal control as patient was not willing for medical androgen deprivation therapy due to cost affordability. For bone metastasis patient was started on zoledronic acid and calcium supplement. Histopathological examination showed metastatic carcinoma in bilateral testes and epididymis from prostatic adenocarcinoma [Table/Fig-2]. The diagnosis of metastatic prostate cancer was confirmed by immunohistochemical analysis (positive stain for prostate specific antigen and prostate acid phosphatase). On last follow up after one year, patient’s PSA was 0.5 ng/ml and serum testosterone was below 20 ng/dl and patient is asymptomatic for bone metastasis.
a) H&E section at 20x shows sheets of malignant cells enveloping the seminiferous tubules; b) H&E section at 40x shows sheets of round to oval cells with prominent nucleoli in the interstitium.
Discussion
In male population, prostatic adenocarcinoma is one of the most frequently diagnosed tumours. The most common sites of secondary involvement are pelvic lymph nodes, bones and lungs, and rarely bladder, liver and brain. Epididymal involvement is unusual whereas testis is an uncommon site. Further, simultaneous involvement of testis and epididymis is exceptional. Testicular metastasis is uncommon that are present in 0.02 to 2.5% of autopsies, with approximately 200 cases being reported in the literature [1]. Metastasis to epididymis is extremely rare with few case reported in literature. Metastasis of carcinoma of the prostate to the testis is rare and seen only in advanced disease and therefore accompanied by multiple metastasis to other organs. Prostate cancer may spread to the testis by arterial embolism, retrograde venous extension, retrograde lymphatic spread, or direct extension through the vas deferens [2]. We believe that the prostate cancer may have spread to the testis and epididymis by arterial embolism or retrograde venous extension. The incidence rate of testicular metastasis in orchiectomy specimens is about 2-4%, performed for hormonal management of advanced prostate carcinoma [3,4].
There are many case reports on testicular metastasis from carcinoma prostate with varied presentation. But there is only single case report in literature on metastasis to bilateral testis and epididymis from carcinoma prostate to our best knowledge. Johansson JE and Lannes P reported metastasis to the spermatic cord, epididymis and testicles from carcinoma of the prostate [5].
The prognostic significance of testicular localization is still unknown. Nevertheless, it is commonly regarded as a sign of advanced prostate disease. The outcome of patients who harbour testicular metastasis and treated by medical castration is not known. Further, research is required to determine the significance of testicular metastasis in the natural history of prostate adenocarcinoma.
Conclusion
This case highlights the need for proper evaluation of testis and para-testicular structures, for accurate staging of these tumours and to exclude any possible metastasis. Our case highlights the importance of inspection of epididymis during sub-capsular orchiectomy for prostate cancer.
[1]. Dutt N, Bates AW, Baithun SI, Secondary neoplasms of the male genital tract with different patterns of involvement in adults and childrenHistopathology 2000 37:323-31. [Google Scholar]
[2]. Bubendorf L, Schopfer A, Wagner U, Sauter G, Moch H, Willi N, Metastatic patterns of prostate cancer: an autopsy study of 1589 patientsHum Pathol 2000 31:578-83. [Google Scholar]
[3]. Tu SM, Reyes A, Maa A, Pisters LL, Pettaway CA, Lin SH, Prostate carcinoma with testicular or penile metastases. Clinical, pathologic, and immunohistochemical featuresCancer 2002 94:2610-17. [Google Scholar]
[4]. Baykal K, Yildirim S, Inal H, Kalci E, Albayrak S, Cingil H, Metastasis of prostate adenocarcinoma to testisInt J Urol 1997 4:104-05. [Google Scholar]
[5]. Johansson JE, Lannes P, Metastases to the spermatic cord, epididymisand testicles from carcinoma of the prostate–five casesScand J Urol Nephrol 1983 17:249-51. [Google Scholar]