Posterior Dislocation of Subtalar Joint without Associated Fracture: A Case Report and Review of Literature
Sahil Gaba1, Arvind Kumar2, Vivek Trikha3, Saubhik Das4, Prabhat Agrawal5
1 Senior Resident, Department of Orthopaedics, All India Institute of Medical Sciences, Chandigarh, India.
2 Senior Resident, Department of Orthopaedics, All India Institute of Medical Sciences, New Delhi, India.
3 Professor, Department of Orthopaedics, All India Institute of Medical Sciences, New Delhi, India.
4 Senior Resident, Department of Orthopaedics, All India Institute of Medical Sciences, New Delhi, India.
5 Senior Resident, Department of Orthopaedics, All India Institute of Medical Sciences, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sahil Gaba, House Number 165, Sector 33 A, Chandigarh-160020, India.
E-mail: drsahilgaba@gmail.com
Posterior subtalar dislocation is an exceedingly rare entity. Clinically, the appearance of the foot can simulate a complex fracture dislocation. It is important to recognize that not all posterior subtalar dislocations are true posterior dislocations. We report a true posterior subtalar dislocation in a 34-year-old female, managed promptly with closed reduction and resulting in an excellent functional outcome. A chronic dislocation or an irreducible dislocation may need open reduction.
Closed reduction, Posterior subtalar dislocation, Subtalar dislocation
Case Report
A 34-year-old female fell down from a stool and landed on her toes with the ankle in plantarflexion, and developed severe pain and swelling of right foot along with deformity.
On presentation to the Emergency Department two hours after the injury, the foot was in plantarflexed position and a bony bump was palpable anteriorly (talar head). Swelling and bruising was present. Dorsalis pedis pulse could not be palpated but posterior tibial pulse was palpable. There was no tenting of the skin. Distal capillary refill was good and oxygen saturation of 99% was recorded in the toes. There was no sensory loss and active toe movements were present. Any attempt at correcting the plantarflexed position increased the pain. Clinically, an injury involving the tarsal bones was suspected.
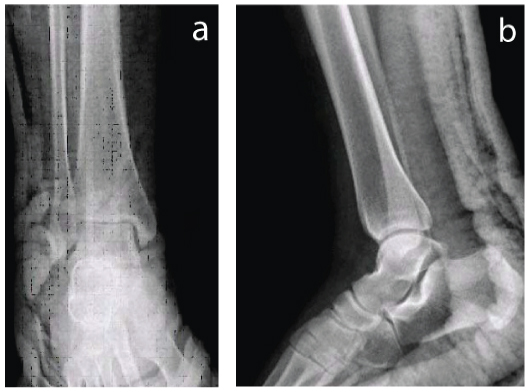
Patient was haemodynamically stable with a Glasgow coma score of 15. Anteroposterior (AP) and lateral radiographs of the ankle [Table/Fig-1] revealed a posterior subtalar dislocation with medial subluxation of the talonavicular joint with no associated fracture. Closed reduction was attempted under conscious sedation and reduction was successful in the first attempt. Reduction was done within two hours of the injury. With the knee flexed (to relax the calf muscles), and foot in plantar flexion, anterior pressure was applied at the heel, with counter-pressure at the head of talus. No attempt was made to forcefully dorsiflex the ankle. Post reduction radiographs [Table/Fig-2] revealed congruent reduction. A below knee Plaster Of Paris (POP) back slab was applied. A CT was done post-reduction to rule out any associated fracture [Table/Fig-3]. Dramatic pain relief occurred post-reduction.
a,b) Anteroposterior view of foot; c) Lateral view of ankle showing posterior subtalar dislocation without any associated fracture. Medial subluxation of the navicular is also seen.

a,b) Post reduction radiographs showing congruent reduction of the subtalar joint.
CT image (sagittal section) showing congruent reduction and absence of any loose bodies in the subtalar joint.

Patient was managed conservatively in a below knee cast for four weeks. Examination at two weeks revealed mild swelling as well as painful range of motion at subtalar joint. Hence, the cast was continued for two more weeks to allow sufficient time for soft tissues to heal. Thereafter, the cast was removed and active assisted range of motion exercises of ankle and foot were begun four weeks after injury. Clinical examination of foot and ankle at this point revealed no laxity or ligamentous injury. Partial weight bearing was allowed, gradually progressing to full weight bearing as per the patient’s tolerance. The patient was able to return to her pre-injury level of activity only after three months. At final follow-up of six months patient was pain free, without any restriction in daily activities, and radiographs did not reveal any evidence of avascular necrosis. Range of motion at subtalar and ankle joints was full and painless.
Discussion
Subtalar dislocation is a type of peritalar dislocation, which involves dislocation of both subtalar (talocalcaneal) and talonavicular joints, without involvement of tibiotalar and calcaneocuboid joints, and without any associated talar neck fracture [1]. The reported incidence of subtalar dislocation is nearly 1% of all dislocations [1]. Most of the literature on this rare injury consists of isolated case reports rather than large case series [Table/Fig-4] [2-9].
Details of previous case reports of isolated posterior subtalar dislocation [2-9].
| Author | Number of cases | Management |
|---|
| Camarda L et al., [7] | 1 | Closed reduction |
| K Bali et al., [4] | 1 | Closed reduction |
| Jungbluth P et al., [6] | 1 | Closed reduction |
| Camarda L et al., [5] | 1 | Closed reduction |
| Krishnan KM et al., [2] | 1 | Closed reduction |
| Inokuchi S et al., [3] | 2 | Closed reduction |
| Pinzur MS et al., [8] | 1 (Open dislocation) | Debridement and open reduction |
| Leitner B [9] | 1 | Closed reduction |
The first literature account of this rare injury dates back to 1803. Four types are recognized based on direction of displacement of calcaneum relative to talus – medial, lateral, anterior, and posterior. The clinical appearance of the foot can mimic a complex fracture dislocation. In most of the cases, associated osseous lesions (fractures of talus, malleoli, or fifth metatarsal) are present; pure dislocations are less common. The anterior and posterior dislocations are exceedingly uncommon injuries [2,3]. The posterior dislocation accounts for 1-2.5% of the subtalar dislocations [2]. We report a case of posterior subtalar dislocation without any associated bony lesion, where closed reduction was followed by an excellent clinical outcome. The mechanism of reduction and the importance of prompt recognition and reduction are also discussed. There are a handful of case reports of posterior subtalar dislocation in the literature.
Forceful inversion and eversion of the foot leads to medial and lateral subtalar dislocations respectively. This is just an oversimplification though, as the exact mechanism is more complex and involves a set pattern of events, finally culminating in a medial or lateral dislocation. Deltoid ligament and interosseus ligament are ruptured in lateral dislocations, whereas calcaneofibular ligament and interosseous ligament are torn in medial dislocation. The mechanism of posterior dislocation is hyper-plantarflexion of the foot [3,4]. Both medial and lateral ligaments, along with interosseus ligament are torn in posterior and anterior dislocations [3,4].
Due to the high rate of associated osseous lesions, a post reduction CT scan is a must to rule out such injuries, as they may be easily overlooked on radiographs. In fact, Bibbo C et al., believe that the reported incidence of associated osseous lesions in the literature is less than it actually is, as CT scan was not performed routinely in all cases [10]. They were of the opinion that the real incidence may be as high as 100% if CT was done in all cases [10]. Specifically in posterior dislocations, incidence of osseous lesions has been reported to be 57.1%.
Closed reduction is usually successful in subtalar dislocation, but occasionally interposed tendons, buttonholing through capsule, or interposed bony fragments may make closed reduction impossible. Most of the reports describing irreducible dislocations have been of medial and lateral dislocations [10]. We came across only one case of irreducible posterior dislocation in the literature [11]. It was caused due to an incarcerated fracture fragment derived from the anterior process of calcaneum, and needed open reduction and fixation of the fragment.
Posterior subtalar dislocation was first described by Luxembourg in 1907 [4]. Inokuchi S et al., suggested that the diagnosis of a posterior subtalar dislocation should be made when the lateral radiograph shows head of talus perched on the navicular, while the AP radiograph reveals absence of any medial or lateral displacement or rotation of calcaneum [3].
Conclusion
Although an exceedingly rare injury, a good functional outcome can be expected with prompt closed reduction. Open reduction is needed only when dislocation is chronic, or unreducible due to an incarcerated bony fragment. A CT scan post reduction is a must to rule out any bony fragments, as these may need surgical removal if located in joint space. Follow-up examinations must include testing for any ligamentous laxity, and to look for avascular necrosis of talus or subtalar arthritis. Forceful attempt at reduction without first confirming the diagnosis should be avoided to avoid iatrogenic fracture of talus or calcaneum.
[1]. Prada-Cañizares A, Auñón-Martín I, y Rico JV, Pretell-Mazzini J, Subtalar dislocation: management and prognosis for an uncommon orthopaedic conditionInternational Orthopaedics 2016 40(5):999-1007. [Google Scholar]
[2]. Krishnan KM, Sinha AK, True posterior dislocation of subtalar joint: a case reportThe Journal of foot and ankle surgery 2003 42(6):363-65. [Google Scholar]
[3]. Inokuchi S, Hashimoto T, Usami N, Posterior subtalar dislocationJournal of Trauma and Acute Care Surgery 1997 42(2):310-13. [Google Scholar]
[4]. Bali K, Kumar V, Bhagwat K, Rawall S, Closed posterior subtalar dislocation without any associated fracture: a case report and review of the literatureFoot and Ankle Surgery 2011 17(3):e40-42. [Google Scholar]
[5]. Camarda L, Martorana U, D’arienzo M, Posterior subtalar dislocationOrthopedics 2009 32(7):530 [Google Scholar]
[6]. Jungbluth P, Wild M, Hakimi M, Gehrmann S, Djurisic M, Windolf J, Isolated subtalar dislocationThe Journal of Bone & Joint Surgery 2010 92(4):890-94. [Google Scholar]
[7]. Camarda L, Abruzzese A, La Gattuta A, Lentini R, D’Arienzo M, Results of closed subtalar dislocationsMusculoskeletal surgery 2016 100(1):63-69. [Google Scholar]
[8]. Pinzur MS, Meyer Jr PR, Complete posterior dislocation of the talus. Case report and discussionClinical orthopaedics and related research 1977 (131):205-09. [Google Scholar]
[9]. Leitner B, Obstacles to reduction in subtalar dislocationsJBJS 1954 36(2):299-306. [Google Scholar]
[10]. Bibbo C, Anderson RB, Davis WH, Injury characteristics and the clinical outcome of subtalar dislocations: a clinical and radiographic analysis of 25 casesFoot & Ankle International 2003 24(2):158-63. [Google Scholar]
[11]. Budd H, Wimhurst J, Davis B, Hutchinson R, Irreducible posterior subtalar dislocation with incarceration of a fracture of the anterior process of the calcaneumBone & Joint Journal 2010 92(7):1025-27. [Google Scholar]