Large Vulvar Haematoma of Traumatic Origin
Dimitrios Papoutsis1, Hope K Haefner2
1 Research Fellow, Department of Obstetrics and Gynaecology, Shrewsbury and Telford Hospital NHS Trust, United Kingdom.
2 Professor, Department of Obstetrics and Gynaecology, University of Michigan Center for Vulvar Diseases, Michigan Medicine, Ann Arbor, Michigan, United States of America.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Dimitrios Papoutsis, Research Fellow, Department of Obstetrics and Gynaecology, Shrewsbury and Telford Hospital NHS Trust, Apley Castle, Telford TF1 6TF, United Kingdom.
E-mail: dimitrios.papoutsis@nhs.net
Conservative, Female, Genitalia, Injury
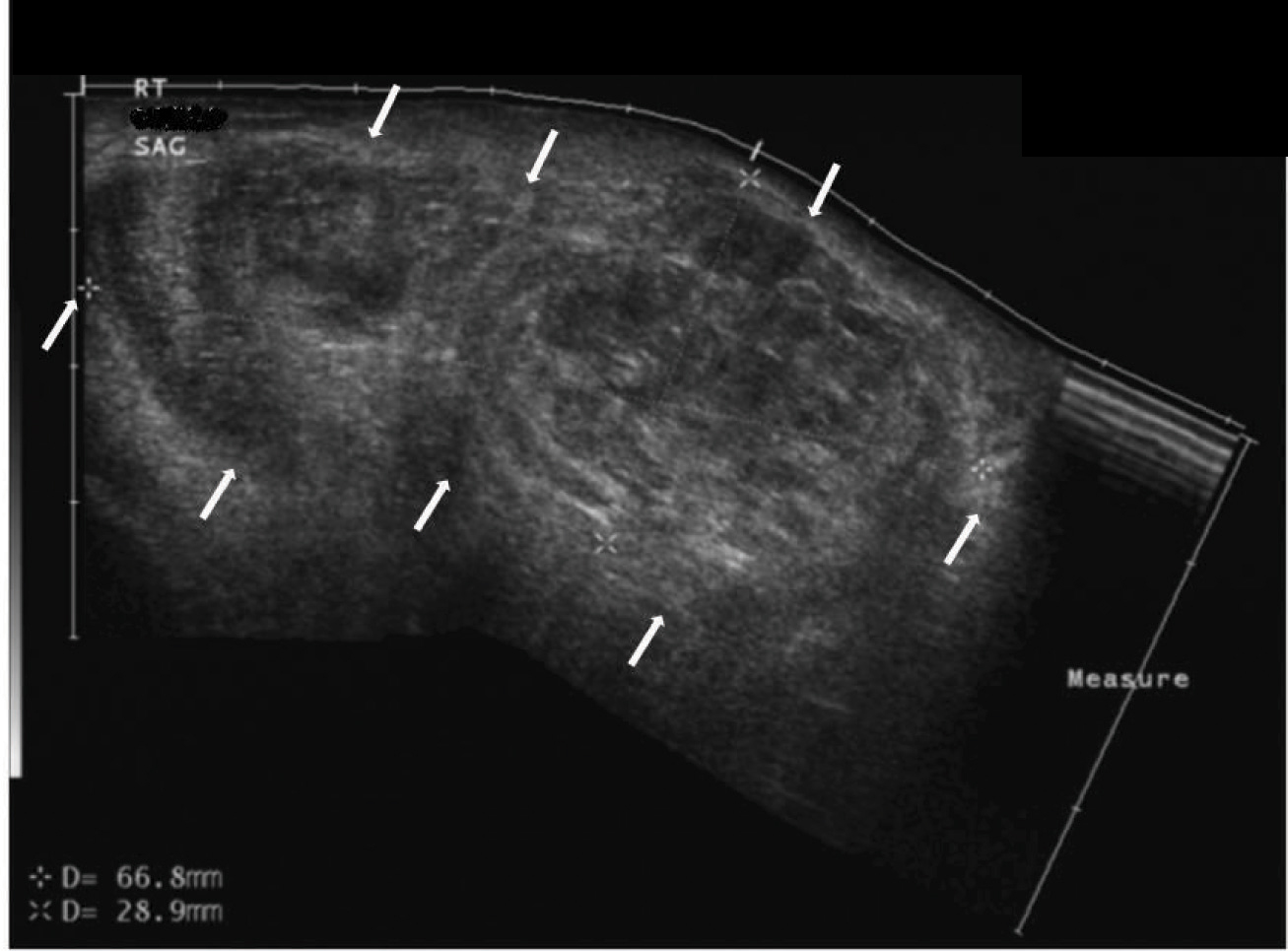
A 40-year-old woman presented to the Emergency room at the University of Michigan Hospital with a large vulvar haematoma following an accidental fall in a squatting position onto the corner of a wooden object after alcohol intoxication. A tense large haematoma, with the majority occurring on the right labium majus was present [Table/Fig-1]. There was tenderness to touch. An ultrasound was performed to investigate the size, site and expansion of the haematoma. A localized 6.7 cm x 2.9 cm x 3 cm heterogeneous hypoechoic lesion compatible with a non-expanding haematoma was noted, with no discrete fluid collection amenable to drainage [Table/Fig-2]. The patient was managed conservatively with systemic pain relief with oxycodone 5 mg tablets orally every four to six hours as needed for pain. The patient was also advised to perform warm water soaks to improve the local circulation and assist in the reabsorption of this haematoma. The patient was discharged and was advised to be seen either by her primary care physician or in the emergency room if she noted any worsening in swelling of her labial haematoma, or symptoms such as new fever or bleeding. The patient was lost on follow up and there is no further information as to how many days it took for the haematoma to regress.
Significantly distorted anatomy due to the tense large haematoma on the right labium majus.

Ultrasound imaging of the right labium majus in the sagittal plane that demonstrates a heterogeneous hypoechoic lesion (white arrows) with an appearance compatible with a haematoma. It measures approximately 6.7 cm x 2.9 cm x 3 cm.
Vulvar haematomas in non-obstetric women are rare and not extensively reported in the literature [1]. The reported incidence is 3.7% [2] and they constitute up to 0.8% of all gynaecologic admissions [3]. They often result from direct perineal trauma that crushes the vulvar tissue against the pelvic bones causing vascular injury such as in cases of straddle type injuries, forceful coitus or sexual assault [1]. Though perineal trauma has been regarded as the main cause, there have also been cases reported of spontaneous vessel rupture that have resulted in a vulvar haematoma in non-obstetric settings [4].
Different imaging modalities have been used to investigate the size, location and expansion of the haematoma. Perineal ultrasound has been reported to provide an easy and objective bedside assessment of the extent of the haematoma [5]. Other more complex and expensive imaging modalities involve Computed Tomography (CT) and Magnetic Resonance Imaging (MRI). They both allow for a more specific and detailed mapping of the vulvar haematoma with the capacity to exclude a possible retroperitoneal involvement and to detect any bleeding vessels [6,7].
There are no consensus management guidelines and a paucity of literature exists [1]. The majority of vulvar haematomas are managed conservatively, however if the haematoma continues to grow surgical intervention may be required [8]. Blood clot evacuation, ligation of the bleeding points, and primary closure of the haematoma cavity have been reported as a means of surgical treatment [4,8]. Selective arterial embolization has also been reported as an alternative to traditional surgical exploration [1].
In the presented case, the haematoma was stable and non expanding and therefore was managed conservatively with the use of systemic pain medication and warm water soaks.
[1]. Ernest A, Knapp G, Severe traumatic vulva hematoma in teenage girlClin Case Rep 2015 3:975-78. [Google Scholar]
[2]. Habek D, Kulas T, Non obstetric vulvovaginal injuries: mechanism and outcomeArch Gynecol Obstet 2007 275:93-97. [Google Scholar]
[3]. Rabinerson D, Fradin Z, Zeidman A, Horowitz E, Vulvar hematoma after cunnilingus in a teenager with essential thrombocythemia: a case reportJ Reprod Med 2007 52:458-59. [Google Scholar]
[4]. Hong HR, Hwang KR, Kim SA, Kwon JE, Jeon HW, Choi JE, A case of vulvar hematoma with rupture of pseudoaneurysm of pudendal arteryObstet Gynecol Sci 2014 57:168-71. [Google Scholar]
[5]. Sherer DM, Stimphil R, Hellmann M, Abdelmalek E, Zinn H, Abulafia O, Transperineal sonography of a large vulvar hematoma following blunt perineal traumaJ Clin Ultrasound 2006 34:309-12. [Google Scholar]
[6]. Butori N, Coulange L, Filipuzzi L, Krause D, Loffroy R, Pseudoaneurysm of the uterine artery after cesarean delivery: management with superselective arterial embolizationObstet Gynecol 2009 113:540-43. [Google Scholar]
[7]. Guerriero S, Ajossa S, Bargellini R, Amucano G, Marongiu D, Melis GB, Puerperal vulvovaginal hematoma: sonographic findings with MRI correlationJ Clin Ultrasound 2004 32:415-18. [Google Scholar]
[8]. Takagi K, Akashi K, Horiuchi I, Nakamura E, Samejima K, Ushijima J, Managing vulvovaginal hematoma by arterial embolization as first-line hemostatic therapyTaiwan J Obstet Gynecol 2017 56:224-26. [Google Scholar]