Bilateral Persistent Hyperplastic Primary Vitreous - A Rare Case Report
Rashmi Kumari1, Bhawesh Chandra Saha2
1 Senior Resident, Department of Ophthalmology, Indira Gandhi Institute of Medical Sciences, Patna, Bihar, India.
2 Senior Resident, Department of Ophthalmology, All India Institutes of Medical Sciences, Patna, Bihar, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rashmi kumari, House No. O/13 Ashiana Nagar phase 1, Patna-800025, Bihar, India.
E-mail: dr.rchandras08@gmail.com
Persistent Hyperplastic Primary Vitreous (PHPV), now-a-days referred to as Persistent Fetal Vasculature (PFV), is a rare congenital anomaly of the eye that typically presents unilaterally with white pupillary reflex and microphthalmia without systemic associations. Bilateral presentations are rare. Here we report a case of 15-year-old male with bilateral PFV without leucokoria who was misdiagnosed as congenital esotropia with amblyopia, treated for refractive errors and referred to higher centre for squint corrections. The diagnosis of PFV was made easily on slit lamp examination with dilated pupil due to media clarity. Findings were confirmed by colour doppler ultrasonography of the eyes. This case warrants essential screening of the posterior segment of all children with deviated eyes to ensure earliest detection of such pathologies.
Leucokoria, Microphthalmus, Persistent fetal vasculature
CASE REPORT
A 15-year-old male child presented in our tertiary eye care centre with complaints of defective vision with inward deviation and abnormal movements in both eyes for last six to eight years. The symptoms were progressive in nature. He was diagnosed as congenital esotropia and treated for refractive errors with assurance of squint corrections at later age by the treating doctors. The child was born at full-term by normal vaginal delivery. On examination, visual acuity was counting fingures-1 mt and 2 mt in right and left eyes respectively. There was a wide angle convergent squint with preferential fixation with left eye [Table/Fig-1].
Wide angle convergent squint.
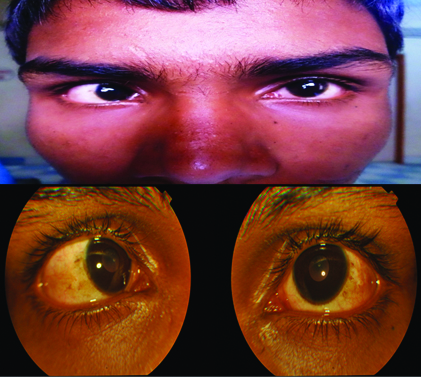
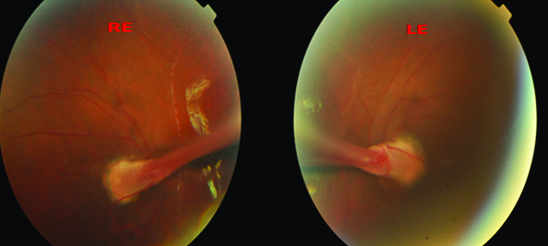
The size of the cornea looked smaller with corneal diameter (horizontal/vertical) of 11.5/11 mm in both eyes. Pupil was round regular and reacting normal to light .Slit lamp examination with dilated pupil showed a fibrous band attached on posterior surface of the lens capsule in both eyes [Table/Fig-2a]. The posterior segment examination showed a falciform fold arising from the optic disc [Table/Fig-2b].
Slit lamp examination with dilated pupil showing fibrous band attached on the posterior surface of the lens capsules in both eyes.

Posterior segment examination showed a falciform fold arising from the optic disc in both eyes.
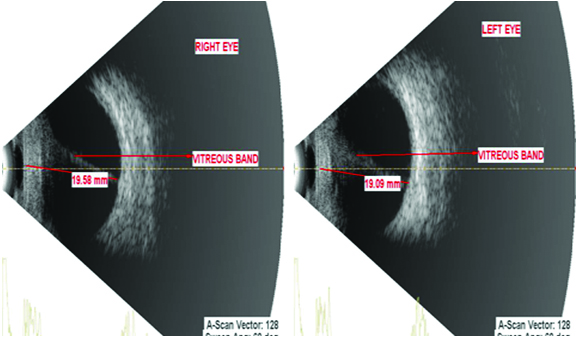
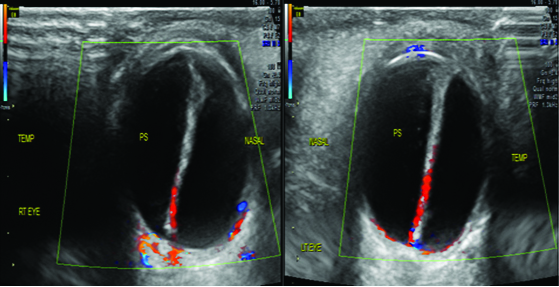
Ocular ultrasound revealed thick echogenic membrane like structure extending from posterior surface of the lens to optic nerve head. Axial lengths of right eye (19.58 mm) and left eye (19.09 mm) suggested microphthalmia [Table/Fig-3]. Colour doppler supplementation showed vascularity [Table/Fig-4].
Ocular ultrasound showing thick echogenic membrane like structure extending from posterior surface of the lens to optic nerve head. Axial lengths of Right Eye (RE) (19.58 mm) and Left Eye (LE) (19.09 mm) suggested microphthalmia.
Colour doppler ultrasonography showing vascularity in the echogenic band extending from posterior capsule of lens to the optic nerve head.
Based on the above findings, a diagnosis of bilateral PFV was made. There was no systemic abnormality. Subjective and objective refraction were done under cycloplegia but visual acuity did not improve with glasses suggesting stimulation deprivation amblyopia. Visual prognosis was explained to the parents. Patient was advised for cosmetic correction of squint but parents refused surgery under guarded visual prognosis.
Discussion
PHPV is an uncommon congenital developmental anomaly of the eye first described in detail by Reese AB in 1955 [1]. It was renamed by Goldberg M as Persistent Fetal Vasculature Syndrome (PFVS) in 1997 which refers to the persistence of embryonic primary vitreous and fetal hyloid vasculature due to arrest in the process of their normal involution by the stipulated time [2]. This can lead to a wide spectrum of ocular complication as a sequale to its subsequent contraction and opacification like shallow anterior chamber, cataracts, angle closure glaucoma, elongated ciliary processes, retrolental mass, microphthalmos, and retinal detachment eventually lead to phthisis bulbi and intractable glaucoma [3]. Depending upon the part and extent of involvement they are classified as anterior, posterior or mixed variety [4].
Patient of PHPV most commonly presents unilaterally with white pupillary reflex and microphthalmia without associated systemic finding [5]. Bilateral presentations are rare and are known have systemic and syndromic associations such as trisomy 13, 15, or 18, Norrie’s disease, Warburg’s syndrome [6]. The case discussed here differed from the typical presentation in being bilateral but without any systemic association. Moreover, it presented with deviated eyes without any white pupillary reflex although there was microphthalmus. Presence of white reflex makes the condition noticeable to the parents and timely diagnosis with early intervention enables preserving some productive vision [7]. Though, the patient was taken to many to local doctors since infancy for poor vision and progressively deviating eyes complete examination including dilated fundoscopy was never attempted as there was no alarming sign like leucocoria except mild deviation which are quite common in normal infants. Moreover, it would have needed general anaesthesia or sedation. Since PHPV is a congenital anomaly, proper examination of suspected children with pupillary dilatation is must. Though, in our patient media was sufficiently clear to visualise the complete vitreous band on simple pupillary dilatation, many a times opaque media due to cataract or retrolental mass warrants additional radiological investigations like ultrasonography or CT scan [8]. It not only diagnoses PHPV but also classifies it into anterior, posterior or mixed variety essential to plan further line of management. Nevertheless it rules out retinoblastoma, one of the important differentials with life threatening potentials [9]. Although visual prognosis of PFV is generally poor, but timing of intervention and amblyopia management are the most important determinants for final visual prognosis [10]. Our patient presented very late as the eyes were already amblyopic. Though, he had mixed variety of PHPV, there was only focal opacification of the lens at the anterior stalk, not sufficient enough to cause white pupillary reflex but since it was involving the visual axis it caused marked visual loss. Absence of the white reflex, as in our case, let it undiagnosed till the mid-teens when it was too late. The child went blind due to improper screening of the posterior segment on initial consultation.
Conclusion
PHPV is essentially a disease of newborns. Every child presenting with squint and nystagmus should undergo detailed posterior segment evaluation even if it needs examination under anaesthesia/sedation which can sometimes be very crucial. Although visual prognosis of PFV is poor, but by early intervention and amblyopia management we can at least preserve some productive vision to the child.
[1]. Reese AB, Persistent hyperplastic primary vitreousAm J Ophthalmol 1955 30:317-31. [Google Scholar]
[2]. Goldberg M, Persistent fetal vasculature syndrome (PFV): an integrated interpretation of signs and symptoms associated with persistent hyperplastic primary vitreous (PHPV). LIV Edward Jackson Memorial LectureAm J Ophthalmol 1997 124:587-626. [Google Scholar]
[3]. Mafee MF, Goldberg MF, Persistent hyperplastic primary vitreous: role of computed tomography and magnetic resonanceRadiol Clin North Am 1987 25:683-92. [Google Scholar]
[4]. Larsen WJ, Development of the eyesHuman Embryology 1993 New YorkChurchill Livingstone:341-51. [Google Scholar]
[5]. Jain T, Bilateral persistent hyperplastic primary vitreousIndian J Ophthalmol 2009 57:53-54. [Google Scholar]
[6]. Galhotra R, Gupta K, Kaur S, Singh P, Bilateral persistent hyperplastic primary vitreous: A rare entityOman J Ophthalmol 2012 5(1):58-60. [Google Scholar]
[7]. Sanghvi DA, Sanghvi CA, Purandare NC, Bilateral persistent hyperplastic primary vitreousAustralas Radiol 2005 49:72-74. [Google Scholar]
[8]. Pollard ZF, Persistent hyperplastic primary vitreous: diagnosis, treatment and resultsTrans Am Ophthalmol Soc 1997 95:487-549. [Google Scholar]
[9]. Rizvi SW, Siddiqui MA, Khan AA, Ahmad I, Ullah E, Sukul RR, Bilateral persistent hyperplastic primary vitreous: a close mimic of retinoblastomaSemin Ophthalmol 2013 28(1):25-27. [Google Scholar]
[10]. Haddad R, Font RL, Reeser F, Persistent hyperplastic primary vitreous: A clinicopathologic study of 62 cases and review of the literatureSurv Ophthalmol 1978 23:123-34. [Google Scholar]