Giving Birth After Fertility Sparing Treatment for a Yolk Sac Tumour: Case Report
Georgios-Marios Makris1, Alexandros Fotiou2, Georgios Chrelias3, Marco-Johannes Battista4, Charalampos Chrelias5
1 Head, Department of Obstetrics and Gynecology, Athens Euroclinic Hospital, Athens, Greece.
2 Resident, Department of Obstetrics and Gynecology, Athens Euroclinic Hospital, Athens, Greece.
3 Resident, Department of Obstetrics and Gynecology, General University Hospital “Attikon”, University of Athens, Athens, Greece.
4 Professor, Department of Gynecology and Obstetrics, University Hospital Mainz, Mainz, Germany.
5 Professor, Department of Obstetrics and Gynecology, General University Hospital “Attikon”, University of Athens, Athens, Greece.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Georgios-Marios Makris, 9, Athanasiadou Street, Athens-11521, Greece.
E-mail: makrismg@hotmail.com
Yolk Sac Tumours (YSTs) of the ovary, also called Endodermal Sinus Tumours (ESTs), are the second most common Malignant Ovarian Germ Cell Tumours (MOGCTs), after dysgerminomas. YSTs occur primarily in children and young women. We present a case report of a 20-year-old woman who had been diagnosed with YST (tumour diameter of 29 cm). The patient underwent fertility sparing surgery and was subsequently treated with adjuvant chemotherapy (four cycles of bleomycin, etoposide and cisplatin). Two years after the diagnosis of YST, she successfully gave birth to a healthy girl (birth weight 3,500 g, Apgar score of 9-10 and a spontaneous vaginal delivery). During pregnancy, she had microscopic hematuria and bilateral nephrolithiasis, was ultrasonographically diagnosed. The conception after fertility sparing treatment of YST is possible and the birth of a healthy child is feasible. There are no current guidelines for surveillance of such patients during pregnancy; however, structured pregnancy surveillance in such survivors seems necessary.
Delivery, Endodermal sinus tumour, Fertility preservation, Germ cell tumours, Ovarian cancer
Case Report
A 20-year-old young woman was admitted to our department due to abdominal pain, abdominal enlargement and progressive flatulence since three months. History of patient revealed that she was a carrier of beta-thalassemia and was not on medication for anything. She was a non-smoker. At the age of 18 years, she had undergone vertical banded gastroplasty in order to control her body weight.
On physical examination, a sizeable mass was detected up to umbilicus. On combined abdominal and transvaginal ultrasound, in the left ovary, a mixed nature mass measuring 130 mm x 100 mm was noted. CT scan revealed a large pelvic cystic mass, diameter of 29 cm without signs of hepatic and pulmonary metastases. The mass showed a distinct margin and contained haemorrhagic elements. Bone scan, mammography and colonoscopy were free of metastasis. Serum levels of Alpha Fetoprotein (AFP) were 1210 ng/ml.
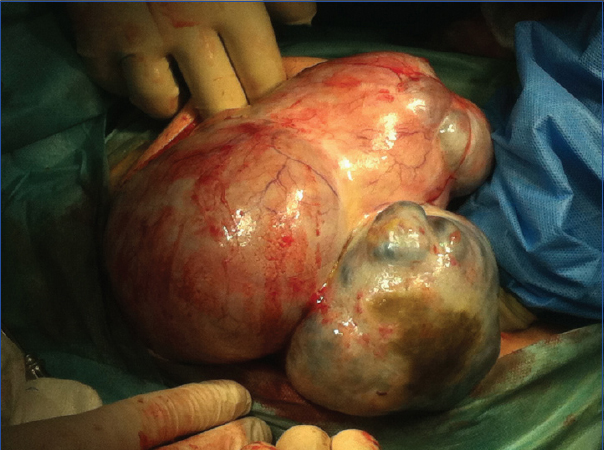
The patient underwent surgical removal of her left ovary [Table/Fig-1], partial removal of the omentum and biopsies of right ovary were negative for malignancy. The cytology examination of peritoneal washing was negative for malignancy. The histological examination revealed a YST with mixed density; the endometrioid component predominated, but myxoid, compact and cystic elements also coexisted. Areas with necrosis were noted and the neoplasm did not invade the ovarian surface.
Yolk sac ovarian tumour in a 20-year-old patient.
After the surgical removal of the tumour, the patient underwent four cycles of adjuvant chemotherapy with bleomycin, etoposide and cisplatin. Approximately one year after the completion of chemotherapy, the woman spontaneously conceived. During the second trimester of pregnancy, microscopic hematuria was detected in urinalysis; the ultrasound examination revealed bilateral nephrolithiasis. No other clinical symptoms occurred till the end of pregnancy. At 39th gestational week, she gave birth to a healthy girl (birth weight 3,500 gm, Apgar score: 9 in first minute and 10 in fifth minute and a spontaneous vaginal delivery). Three months after delivery, the woman is recurrence free and the infant did not show any problems. AFP remained within normal range.
Written informed consent was obtained by the patient for the publication of this case report.
Discussion
MOGCTs are rare, accounting for approximately 5% of all ovarian malignancies [1]. They are derived from primitive germ cells of the embryonic gonad and can undergo germinomatous or embryonic differentiation. YSTs of the ovary, also called ESTs, are the second most common MOGCTs, after dysgerminomas [1]. YST accounts for ~20% of MOGCTs, representing about 1% of all ovarian malignancies [2]. In USA, the age-adjusted incidence rate per 100,000 women is 0.048; they occur primarily in children and young women [1]. Median age of diagnosis is 19 to 22 years, in contrast to perimenopausal or postmenopausal age associated with ovarian epithelial cancer [3,4].
The most common symptom of YST is abdominal bloating. An asymptomatic and palpable abdominal or pelvic mass with abdominal enlargement is also a common first sign that can lead to the discovery of the tumour. Fever can be present in some patients. Secondary to torsion or infection, YST can present with ascites or peritonitis [5]. The duration of the symptoms range from two days to six months, with a median duration of four weeks [5]. Preoperative clinical, biological and radiological findings should help to establish the diagnosis of ovarian YST. CT scan may reveal a large mass of solid, cystic or mixed texture [6]. Elevated serum levels of AFP can be useful [7,8].
Ovarian YSTs are rare malignant ovarian tumours that occur in young age [4]. Because of that, the treatment strategy should ideally be directed to long term survival and fertility preservation. The main treatment consists of excision or complete removal of the tumour, followed by adjuvant chemotherapy.
The use of platinum-based regimens (e.g., BEP) in combination with fertility preservative surgical techniques has dramatically improved survival combining with fertility preservation in women diagnosed with YST. Mitchell PL et al., [9], Nishio S et al., [10], Low JJ et al., [11],
Ayhan A et al., [12] and de La Motte Rouge T et al., [13] examined the numbers of patients experiencing regular menstruation after treatment, the conception rates and the successful pregnancy rates; among patients attempting conception, the rate of successful pregnancies was satisfactory, surpassing 60% [Table/Fig-2].
Successful pregnancy rates in patients after treatment for malignant ovarian germ cell tumours (MOGCT) and yolk sac tumours (YST) of the ovary.
| Studies | Number of patients who experienced regular menstruation after treatment | Number of patients who attempted conception | Number of patients who had a successful pregnancy |
|---|
| Mitchell PL et al., [9] (MOGCT) | 24 of 26 | Not reported | 11 |
| Nishio S et al., [10] (MOGCT) | 28 of 30 | 12 | 8 |
| Low JJ et al., [11] (MOGCT) | 43 of 47 | 20 | 19 |
| Ayhan A et al., [12] (YST) | 10 of 15 | 5 | 3 |
| de La Motte Rouge T et al., [13] (YST) | 38 of 49 | 16 | 12 |
An interesting case was presented by Chanu MM et al., in which a YST was diagnosed in a 20-year-old pregnant woman. Laparotomy as well as a C-section was done and the patient was managed successfully in giving birth to a healthy female baby [14].
Conclusion
YST affects predominantly young age patients. When the ovarian cancer FIGO classification stage permits so (preferably early stage), a fertility sparing option should be provided. Even after proper chemotherapy, a conception is possible and the birth of a healthy child is feasible. These cases should however be appointed as high-risk pregnancies and minor possible post-surgical and post-chemotherapy considerations should be expected. There are no current guidelines for surveillance of such patients during pregnancy, e.g. AFP, beta-hCG and Ca-125 blood levels, abdominal sonography or magnetic resonance imaging. However, the number of affected patients will rise as we understand more about the nature of YSTs and we will be able to offer more frequently the fertility sparing option. The need for structured pregnancy surveillance in cancer survivors is more than necessary. Nonetheless, hysterectomy and contralateral adnexectomy could be considered after family planning completion.
[1]. Smith HO, Berwick M, Verschraegen CF, Wiggins C, Lansing L, Muller CY, Incidence and survival rates for female malignant germ cell tumorsObstet Gynecol 2006 107(5):1075-85. [Google Scholar]
[2]. Dallenbach P, Bonnefoi H, Pelte MF, Vlastos G, Yolk sac tumours of the ovary: an updateEur J Surg Oncol 2006 32(10):1063-75. [Google Scholar]
[3]. Cicin I, Saip P, Guney N, Eralp Y, Ayan I, Kebudi R, Yolk sac tumours of the ovary: Evaluation of clinicopathological features and prognostic factorsEur J Obstet Gynecol Reprod Biol 2009 146(2):210-14. [Google Scholar]
[4]. Shah JP, Kumar S, Bryant CS, Ali-Fehmi R, Malone JM, JrDeppe G, A population-based analysis of 788 cases of yolk sac tumors: A comparison of males and femalesInt J Cancer 2008 123(11):2671-75. [Google Scholar]
[5]. Gershenson DM, Del Junco G, Herson J, Rutledge FN, Endodermal sinus tumor of the ovary: the M. D. Anderson experienceObstet Gynecol 1983 61(2):194-202. [Google Scholar]
[6]. Li YK, Zheng Y, Lin JB, Xu GX, Cai AQ, Zhou XG, CT imaging of ovarian yolk sac tumor with emphasis on differential diagnosisSci Rep 2015 5:11000 [Google Scholar]
[7]. Talerman A, Haije WG, Baggerman L, Serum alphafetoprotein (AFP) in diagnosis and management of endodermal sinus (yolk sac) tumor and mixed germ cell tumor of the ovaryCancer 1978 41(1):272-78. [Google Scholar]
[8]. Talerman A, Haije WG, Baggerman L, Serum alphafetoprotein (AFP) in patients with germ cell tumors of the gonads and extragonadal sites: correlation between endodermal sinus (yolk sac) tumor and raised serum AFPCancer 1980 46(2):380-85. [Google Scholar]
[9]. Mitchell PL, Al-Nasiri N, A’Hern R, Fisher C, Horwich A, Pinkerton CR, Treatment of nondysgerminomatous ovarian germ cell tumors: an analysis of 69 casesCancer 1999 85(10):2232-44. [Google Scholar]
[10]. Nishio S, Ushijima K, Fukui A, Fujiyoshi N, Kawano K, Komai K, Fertility-preserving treatment for patients with malignant germ cell tumors of the ovaryJ Obstet Gynaecol Res 2006 32(4):416-21. [Google Scholar]
[11]. Low JJ, Perrin LC, Crandon AJ, Hacker NF, Conservative surgery to preserve ovarian function in patients with malignant ovarian germ cell tumors. A review of 74 casesCancer 2000 89(2):391-98. [Google Scholar]
[12]. Ayhan A, Taskiran C, Bozdag G, Altinbas S, Altinbas A, Yuce K, Endodermal sinus tumor of the ovary: the Hacettepe University experienceEur J Obstet Gynecol Reprod Biol 2005 123(2):230-34. [Google Scholar]
[13]. de La Motte Rouge T, Pautier P, Duvillard P, Rey A, Morice P, Haie-Meder C, Survival and reproductive function of 52 women treated with surgery and bleomycin, etoposide, cisplatin (BEP) chemotherapy for ovarian yolk sac tumorAnn Oncol 2008 19(8):1435-41. [Google Scholar]
[14]. Chanu MM, Pradhan B, Teherse N, Meitei LT, Singh NN, Yolk sac tumor in pregnancy: a case reportIOSR J Dent Med Sci 2015 14(2):35-37. [Google Scholar]