Case Report
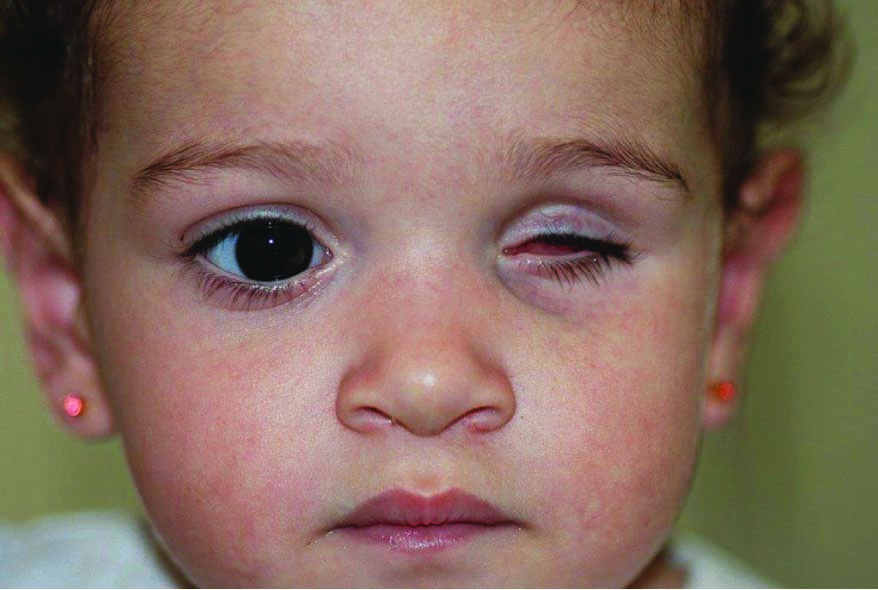
A two-month-old female patient underwent surgery for left eyeball enucleation due to a household accident and was referred to Araçatuba Dental School for rehabilitation with ocular prosthesis.
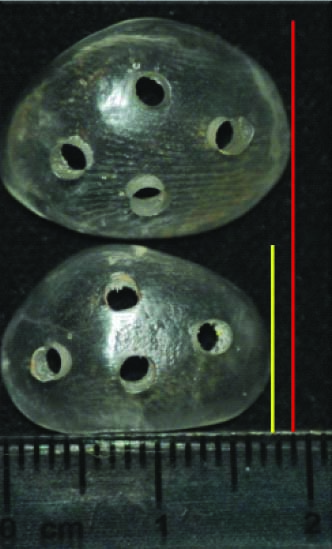
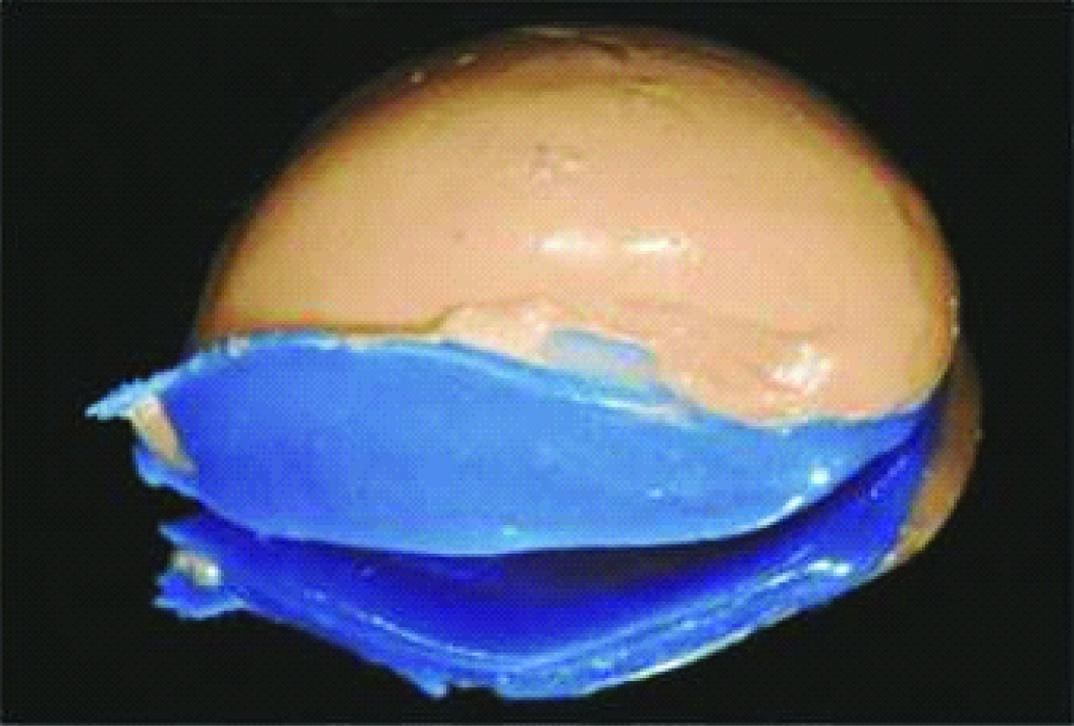
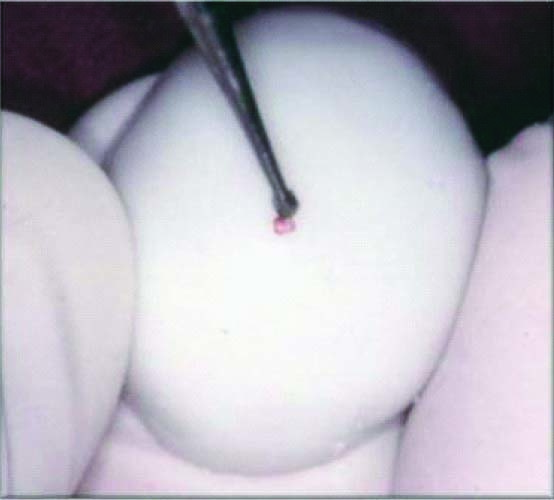
The anophthalmic socket of the patient was examined and an atresic cavity was observed [Table/Fig-1], requiring gradual increase with an acrylic expander, also named as progressive conformer. For this, the anophthalmic socket impression was obtained using dense silicon (Express; 3M ESPE, St. Paul, Minn, USA) [Table/Fig-2]. Topical anaesthesia was not administered in this procedure. The child was kindly held by the social assistant who was responsible for her at that moment. Graduate and Postgraduate students who were present at impression also helped in child cooperation. The mold was inserted into a flask for acrylization with colourless acrylic resin. After polymerization, the expander prosthesis was submitted to finishing and polishing and initially presented the same volume and size of the cavity [Table/Fig-3]. After two weeks, the patient returned with a more elastic cavity, allowing increase on the expander volume. The expander was relined with pink wax, covering its whole anterior area, favouring a higher vertical and horizontal opening of the eyelids. Following relining and acrylization, the expander prosthesis with new dimensions (from approximately 17 mm to 19 mm in length) was installed [Table/Fig-4]. Four months later, the patient exhibited satisfactory anophthalmic cavity dimensions, similar to the healthy eye, which allowed proceeding with ocular prosthesis fabrication [Table/Fig-5].
Atresia anophthalmic socket after eye loss.
Anophthalmic socket impression using dense silicon.

Anophthalmic socket rehabilitated with the initial expander prosthesis, with the same volume and size of the cavity.

Expander prosthesis with new dimensions.
Satisfactory anophthalmilc socket dimensions after using expander.

The impression for fabricating the ocular prosthesis was performed according to Goiato MC et al., [1]. The impression was performed in two steps. Firstly, a portion of Vinylpolysiloxane (VPS) impression material hand-mixed putty (Express; 3M ESPE, St. Paul, Minn, USA), was manipulated and adapted to the patient’s anophthalmic socket until obtaining a superior and inferior palpebral outline similar to contralateral eye. For the second step, low-density VPS was injected onto the internal part of the existing impression [Table/Fig-6]. The fitting was removed and the impression precision was verified. The mold was placed into a flask with stone plaster. After plaster crystallization, the flask was opened and the mold removed.
Two-step socket impression using putty and low-density VPS.
Then, the thermopolymerizable acrylic resin for artificial sclera (Artigos Odontológicos Clássico, SãoPaulo, Brazil), was manipulated, inserted into the flask and polymerized in a microwave oven for 10 minutes. After polymerization, artificial sclera was subjected to finishing and polishing. The sclera try-in was conducted and pupillary center was determined, using a marker pen, based on patient’s contralateral eye [Table/Fig-7].
Determination of pupillary center.
The artificial iris was made of black cardboard disk, painted with oil paint in the same colour of healthy eye and was bonded with white glue on sclera center. The pupil painted in the center of the disk matched the pupil center previously marked on artificial sclera. Sclera characterization was performed with specific pigments and red woolen wires in order to mimic the ocular blood vessels. The prosthesis was finalized with colourless acrylic resin (Artigos Odontológicos Clássico, São Paulo, Brazil) placed over iris painting, submitted to finishing and polishing and subsequently installed.
After 10 months, the one-year-old patient returned with an unsatisfactory prosthesis size and then a new prosthesis was fabricated, fitting the current size of anophthalmic socket [Table/Fig-8]. Today, the patient is more than three-years-old and since the first prosthesis was installed, around five replacements have been made. Ocular prostheses have been changed periodically in order to monitor the patient’s facial growth.

Discussion
The absent eyeball in children leads to loss of stimuli and function, affecting the development of the orbital region and the growth of maxilla, maxillary sinus and mandible [2], which could create a craniofacial hemiatrophy appearance. Therefore, the anophthalmia brings physical, functional, aesthetic and psychological imbalance [3,4].
The primary purpose of treatment for paediatric patients is stimulating tissue growth, to get enough palpebral and conjunctival tissue for supporting the future ocular prosthesis [5] which restores the orbital volume, promoting socket and facial development [6]. Several studies have mentioned different treatments to stimulate orbital volume and soft tissue growth, such as tension wire expanders, pressure conformers and progressive-sized conformers, among others [7,8]. The first two methods often induce harmful scarring by forcing the socket to conform to the shape of the pressure template, while progressively-sized conformers provides gradual stepwise socket expansion, which has been favoured [9].
There is no consensus about the best treatment, however, the most simple and traditional method for rehabilitating these cases is the earlier use of acrylic expander prostheses with periodic changes for successive increases, until obtaining adequate dimension and volume to allow an ocular prostheses installing [4,10]. The ocular prosthesis is an excellent alternative of rehabilitation since it may restore normal functions, such as blinking and even directing tears flow [11].
Although, expander prostheses are the standard mode of ocular prosthetic rehabilitation for paediatric patients, it is very important to reiterate the necessity of progressively rehabilitate children who have lost their eyeballs, once the ocular rehabilitation needs to accompany children’s growth.
The understanding of child’s eye physiology and orbital development is very important to treat anophthalmic paediatric patients [4], since the absent eyeball in childhood leads to a deficiency in orbital growth [3]. According to Chen D and Heher K [5] and Gundlach KK et al., the normal paediatric eye is about 70% of its adult size and grows faster during the first year of life [5,10]. Between 4 and 7 years of age, the eyes can reach up to 90% of their final dimensions, ceasing their growth at 14, while the orbit grows up to 11 years for women and up to 15 for men [10].
Anophthalmic children need to be treated in two stages to recover orbital and palpebral symmetry. Firstly, the treatment should be initiated using an expander device to prevent other disorders in orbital region [4]. Then, the manufacturing of ocular prosthesis must offer the child a normal appearance. Treatment with expander prosthesis is not difficult to conduct, does not cause pain and is well accepted by children [3]. These expanders are generally made up of rigid devices used to expand and increase the conjunctival sac having no effect over the orbit [5].
According to Mazzoli RA et al., the mechanism behind eye expansion with progressive sized conformers is the following [2]: while the lids are expanded via anteriorly directed pressure, the conjunctiva and fornix are expanded via posterior and radially directed pressure and therein lies several rubs: each conformer has to be incrementally larger than the previous, but not so much larger that it is painful or impossible to place in the cul-de-sac. However, if it is too easily placed, it may be too small to have dramatic effect on lid dimensions. At the same time, the conformer has to be bulky enough to exert sufficient posterior pressure to induce conjunctival expansion, but not so bulky as to extrude from socket, while still exerting enough anterior pressure to effect lid growth.
Now-a-days, hydrophilic expanders have also being used [2]. In the beginning, this hydrophilic substance has a hard consistency and is placed in their dry, contracted states. By taking up water, it expands gradually to their full size via osmosis of surrounding tissue fluid, with up to a tenfold increase in volume [9]. The amount and rate of expansion can be engineered and very precisely controlled (Mazzoli RA).
Most authors report that early use of expanders for treating micro/anophthalmic patients brings satisfactory aesthetic results [3]. For this, periodic controls should be performed to assess the progress [5]. According to Hou Z et al., the acrylic expander must present the following characteristics: be easily positioned on a small cavity [7]; gradually increase in a relatively short time and be well tolerated in long-term; avoid uncomfortable peaks of increase; resist to infection, extrusion or complications resulting from increase; and require minor interventions, manipulations or revisions.
After reaching the proper dimensions of anophthalmic cavity with expander prosthesis, it is possible to install the conventional ocular prosthesis, as has been described before on the current case reported. Besides reconstructing face aesthetics, the ocular prosthesis also restores muscle tone, reduces eyelids atresia and clears tear ducts, restoring the motor facial functional normality [11]. Mattos BS et al., state that the conventional ocular prosthesis in children also requires periodic exchanges with successive increases and that it is necessary to determine an exact period for prosthesis exchanges throughout the craniofacial growth to reduce possible discrepancies between the affected and the healthy sides, thus contributing to the harmonious balance of facial development [4].
Conclusion
It is concluded that the use of expander devices is of utmost importance for facial development, besides being easily performed, which makes it a viable and satisfactory measure in cases of early anophthalmia. Yet, the early installing of ocular prosthesis provides an invaluable psychological and social contribution to the physical benefit in overall rehabilitation.
[1]. Goiato MC, Dos Santos DM, Moreno A, Filie Haddad M, Turcio KH, An alternate impression technique for ocular prosthesesJ Prosthodont 2013 22(4):338-40. [Google Scholar]
[2]. Mazzoli RA, Raymond WRt, Ainbinder DJ, Hansen EA, Use of self-expanding, hydrophilic osmotic expanders (hydrogel) in the reconstruction of congenital clinical anophthalmosCurr Opin Ophthalmol 2004 15(5):426-31. [Google Scholar]
[3]. Oberhansli C, Charles-Messance D, Munier F, Spahn B, Management of microphthalmos and anophthalmos: prosthetic experienceKlin Monbl Augenheilkd 2003 220(3):134-37. [Google Scholar]
[4]. Mattos BS, Montagna MC, Fernandes Cda S, Saboia AC, The paediatric patient at a maxillofacial service: Eye ProsthesisBraz Oral Res 2006 20(3):247-51. [Google Scholar]
[5]. Chen D, Heher K, Management of the anophthalmic socket in paediatric patientsCurr Opin Ophthalmol 2004 15(5):449-53. [Google Scholar]
[6]. Clauser L, Sarti E, Dallera V, Galie M, Integrated reconstructive strategies for treating the anophthalmic orbitJ Craniomaxillofac Surg 2004 32(5):279-90. [Google Scholar]
[7]. Hou Z, Yang Q, Chen T, Hao L, Li Y, Li D, The use of self-inflating hydrogel expanders in paediatric patients with congenital microphthalmia in ChinaJ aapos 2012 16(5):458-63. [Google Scholar]
[8]. Krastinova D, Kelly MB, Mihaylova M, Surgical management of the anophthalmic orbit, part 1: congenitalPlast Reconstr Surg 2001 108(4):817-26. [Google Scholar]
[9]. El Essawy RA, Abdelbaky SH, Successful conjunctival socket expansion in anophthalmic patients until the age of 2 years: an outpatient procedureClin Ophthalmol 2016 10:1743-48. [Google Scholar]
[10]. Gundlach KK, Guthoff RF, Hingst VH, Schittkowski MP, Bier UC, Expansion of the socket and orbit for congenital clinical anophthalmiaPlast Reconstr Surg 2005 116(5):1214-22. [Google Scholar]
[11]. Andreotti AM, Goiato MC, Pellizzer EP, Pesqueira AA, Guiotti AM, Gennari-Filho H, Phantom eye syndrome: a review of the literatureScientific World Journal 2014 2014:686493 [Google Scholar]