Recurrent Vaginal Cuff Dehiscence in a Treated Case of Carcinoma Cervix
Sunesh Kumar1, Seema Singhal2, Yamini Kansal3, Dayanand Sharma4
1 Professor, Department of Obstetrics and Gynaecology, All India Institute of Medical Sciences, New Delhi, India.
2 Assistant Professor, Department of Obstetrics and Gynaecology, All India Institute of Medical Sciences, New Delhi, India.
3 Senior Resident, Department of Obstetrics and Gynaecology, All India Institute of Medical Sciences, New Delhi, India.
4 Professor, Department of Radiation Oncology, All India Institute of Medical Sciences, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Yamini Kansal, Department of Obstetrics and Gynaecology. Room no. 3076, Third floor, Teaching Block, AIIMS, Ansarinagar, New Delhi-110029, India.
E-mail: dryaminikansal@gmail.com
Vaginal Cuff Dehiscence (VCD) is partial or total separation of anterior and posterior vaginal cuff layers. We report a case of recurrent vault cuff dehiscence in a patient of cervical carcinoma. A 60-year-old treated case of carcinoma cervix post surgery and radiotherapy was found to have vault dehiscence and intestinal prolapse second time during a routine speculum examination. She underwent an emergency laparotomy and closure of vault. Vaginal Cuff Dehiscence with Evisceration (VCDE) is a rare but potentially fatal complication following hysterectomy. Postoperative infection, poor technique, hematoma, coitus before healing, radiotherapy, corticosteroid therapy are the risk factors. Radiotherapy leads to progressive obliterative endarteritis and resultant tissue hypoxia. There is paucity of literature regarding the best management of VCD, but early corrective intervention is necessary. Patients and the treating physicians should be made aware of this possibility especially those receiving adjuvant radiation or cases of robotic or laparoscopic hysterectomies.
Hysterectomy, Vaginal brachytherapy, Vaginal dehiscence, Visceral prolapse
Case Report
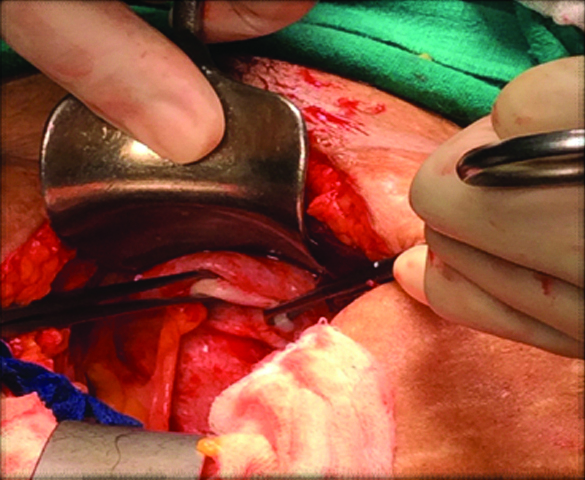
A 60-year-old lady, Gravida 4 Para 3 had come for routine follow up as a treated case of carcinoma cervix. She had undergone total abdominal hysterectomy for abnormal uterine bleeding in a private hospital elsewhere six years back. The initial surgery was inadequate with incomplete surgical staging. The histopathology report revealed high grade squamous cell carcinoma of the cervix. The patient visited the Gynaecology OPD with this report three months after surgery. Details of initial tumor size, nodal status and staging were not available. Clinical examination and imaging at that time revealed residual disease in the vault and the parametria were involved. Pelvic lymph node enlargement was present on imaging. She received adjuvant chemotherapy and radiation (external beam radiation along with vaginal cuff brachytherapy) at the cancer center of the institute. She came for follow up visits irregularly. Two years after the chemoradiation, when she came for a routine check up, vault dehiscence and intestinal prolapse was detected on routine speculum examination. The patient was stable, with no features of bowel obstruction or peritonitis. Emergency laparotomy and closure of vault were done. At the current visit, three years after the vault repair, on inserting the speculum she again developed vault dehiscence with intestinal prolapse. She had no clinical or biochemical signs of peritonitis. Her body mass index was 26 kg/m2. There was no history of steroid intake. There was no history of coitus after radiotherapy. She was immediately taken up for emergency laparotomy. Intra-operatively, inter-bowel adhesions were present and the bowel was adherent to the previous scar site. After adhesiolysis, the bowel was reposited back. Thorough exploration revealed healthy bowel loops without any gangrenous changes. Vault dehiscence of 4 cm length was noted [Table/Fig-1]. Edges of the vault were avascular and fibrosed. There was no evidence of recurrent disease. Closure of vaginal cuff was done via trans-abdominal approach using 1-0 vicryl in a continuous manner. Thorough peritoneal lavage was done. Patient was discharged in a stable condition on fifth post-operative day. She was put on vaginal estrogen cream for the next six months. She remained under follow up and has no complaints six months following the surgery.
Avascular edges of the vault.
Discussion
VCDE following hysterectomy is a rare, but potentially devastating complication with reported incidence being less than 1% after abdominal hysterectomy [1, 2]. If it is not managed rapidly, there are significant chances for morbidity such as peritonitis, bowel injury, gangrene or sepsis and mortality [1]. Many factors are known to result in VCD, namely infection, poor technique, hematoma, coitus before healing, age, radiotherapy, corticosteroid therapy, trauma or rape, previous vaginoplasty, and use of the valsalva maneuver [3].
The incidence of VCD was found to be 0.13% following vaginal hysterectomy, 0.2% with abdominal approach, and 0.64% with laparoscopic route in a study conducted by Uccella S et al [4]. In a recent review involving 20,668 patients, it was found that the incidence of VCD after laparoscopic hysterectomy ranged between 0.64 and 1.35%, while robotic hysterectomy was associated with a risk of approximately 1.64% [5]. Incidence of VCD following abdominal route for hysterectomy has been reported to be as low as 0.03% and is usually below 1% [1,2,6].
The likely predisposing cause for cuff dehiscence in the present case was prior radiotherapy. The pathophysiology behind dehiscence after adjuvant radiotherapy is of progressive obliterative endarteritis, leading to a hypovascular, hypoxic, and hypocellular tissue bed [7]. Spontaneous tissue breakdown may occur in such a vault, especially when exposed to direct trauma as occurred in our case when vault gave way during speculum examination [7]. VCDE triggered by radiotherapy has recently been reported in four cases [6–8]. Three cases were post robotic radical hysterectomy for endometrial carcinoma. VCDE was encountered during brachytherapy cylinder placement [6,8]. The fourth case occurred after radical trans abdominal hysterectomy and adjuvant radiation in FIGO IIA cervical cancer. VCDE developed late, seven years post treatment, similar to the present case [7]. Though, most of the cases have been reported to occur within three months of surgery [9,10].
There is paucity of literature regarding the best management of VCD, but early corrective intervention is necessary and has been followed by most [1]. For the repair of dehiscence any route viz vaginal, abdominal and laparoscopy can be used depending on surgeon’s choice, clinical condition of patient, extent of damage to bowel and ability to evaluate intra-abdominal organs [1]. Whatever route is employed it is necessary to evaluate the bowel for ischaemia or damage and also the surgeon should ensure best tissue approximation and strength of repair [1]. In view of recurrent cuff dehiscence in our patient, trans-abdominal repair was done.
Most incidents occur spontaneously and present with complaints of abdominal pain, vaginal bleeding and discharge [2,11]. Patients and the treating physicians should be made aware of the rare possibility of VCDE especially in those receiving adjuvant radiation or cases of robotic or laparoscopic hysterectomies [11]. In a recent meta-analysis, two effective strategies have been identified in preventing the risk for vaginal cuff dehiscence after minimal access surgeries: the use of barbed suture and the adoption of a transvaginal approach to close vagina [5]. Further, the radiation oncologist should be made wary of the condition, to take steps towards early detection and prevention of this condition. It has been reported that there should be a minimum six weeks interval between surgery and start of radiation to allow for the vault closure to heal well [12]. Apart from this it is advisable to verify the correct placement of cylinders with each application at the time of brachytherapy simulation, and also after therapy cylinder should be inspected for any abnormal fluid [6].
Conclusion
VCDE after radical hysterectomy is a rare complication which may be predisposed by adjuvant radiation because of radiation induced tissue atrophy. Awareness of the condition, early diagnosis and intervention can prevent serious bowel complications. In the era of minimally invasive surgeries, the incidence is ever increasing, and techniques providing greater vaginal cuff strength should be employed.
[1]. Cronin B, Sung VW, Matteson KA, Vaginal cuff dehiscence: risk factors and managementAm J Obstet Gynecol 2012 206:284-8. [Google Scholar]
[2]. Croak AJ, Gebhart JB, Klingele CJ, Schroeder G, Lee RA, Podratz KC, Characteristics of patients with vaginal rupture and eviscerationObstet Gynecol 2004 103:572-6. [Google Scholar]
[3]. Somkuti SG, Vieta PA, Daugherty JF, Hartley LW, Blackmon EB, Transvaginal evisceration after hysterectomy in premenopausal women: a presentation of three casesAm J Obstet Gynecol 1994 171:567-8. [Google Scholar]
[4]. Uccella S, Ceccaroni M, Cromi A, Malzoni M, Berretta R, De Iaco P, Vaginal cuff dehiscence in a series of 12,398 hysterectomies: effect of different types of colpotomy and vaginal closureObstet Gynecol 2012 120:516-23. [Google Scholar]
[5]. Uccella S, Casarin J, Marconi N, Gisone B, Sturla D, Podestà Alluvion C, Incidence and Prevention of Vaginal Cuff Dehiscence Following Laparoscopic and Robotic Hysterectomy: A Systematic Review and Meta-AnalysisJ Minim Invasive Gynecol 2015 22:S40 [Google Scholar]
[6]. Cattaneo R, Bellon M, Elshaikh MA, Vaginal cuff dehiscence after vaginal cuff brachytherapy for uterine cancer. A case reportJ Contemp Brachytherapy 2013 5:164-6. [Google Scholar]
[7]. Kang WD, Kim SM, Choi HS, Vaginal evisceration after radical hysterectomy and adjuvant radiationJ Gynecol Oncol 2009 20:63-4. [Google Scholar]
[8]. Albuquerque K, Shah K, Potkul R, Vaginal cuff dehiscence after intracavitary brachytherapy for endometrial cancerJ Contemp Brachytherapy 2012 4:111-2. [Google Scholar]
[9]. Gujar NN, Choudhari RK, Choudhari GR, Bagali NM, Bendre MB, Adgale SB, Coitus induced vaginal evisceration in a premenopausal woman: a case reportPatient Saf Surg 2011 5:6 [Google Scholar]
[10]. Ceccaroni M, Berretta R, Malzoni M, Scioscia M, Roviglione G, Spagnolo E, Vaginal cuff dehiscence after hysterectomy: a multicenter retrospective studyEur J Obstet Gynecol Reprod Biol 2011 158:308-13. [Google Scholar]
[11]. Nick AM, Lange J, Frumovitz M, Soliman PT, Schmeler KM, Schlumbrecht MP, Rate of Vaginal Cuff Separation Following Laparoscopic or Robotic HysterectomyGynecol Oncol 2011 120:47-51. [Google Scholar]
[12]. Kirsner RS, Eaglstein WH, The wound healing processDermatol Clin 1993 11:629-40. [Google Scholar]