Giant Pyonephrosis Due to Ureteropelvic Junction Obstruction: A Case Report
Rupesh Gupta1, Sweta Gupta2, Arpan Choudhary3, Supriya Basu4
1 Senior Resident, Department of Urology, Radha Gobinda Kar Medical College, Kolkata, West Bengal, India.
2 Junior Resident, Department of Gynaecology and Obstetrics, Radha Gobinda Kar Medical College, Kolkata, West Bengal, India.
3 Senior Resident, Department of Urology, Radha Gobinda Kar Medical College, Kolkata, West Bengal, India.
4 Professor, Department of Urology, Radha Gobinda Kar Medical College, Kolkata, West Bengal, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rupesh Gupta, Khudiram Bose Sarani, Shyam Bazar, Kolkata-700004, West Bengal, India.
E-mail: drrupesgupta@gmail.com
Pyonephrosis is a suppurative infection of upper urinary tract due to obstruction of the ureter. It is usually associated with suppurative damage of renal parenchyma and renal function loss. Patients are mostly symptomatic but may remain asymptomatic in 15% of cases. Severe infection in pyonephrosis may lead to urosepsis and may endangered life, if timely not treated with surgical intervention. We hereby report a rare case of Giant Pyonephrosis (GP), contained 11 liters of pus, due to Ureteropelvic Junction (UPJ) obstruction presented with haematuria. The patient was treated with open nephrectomy. The aetiology, clinical features, diagnosis and management of pyonephrosis with the review of literature of GP in the background of a rare case report have been discussed here.
Haematuria, Nephrectomy, Urinary tract infection
Case Report
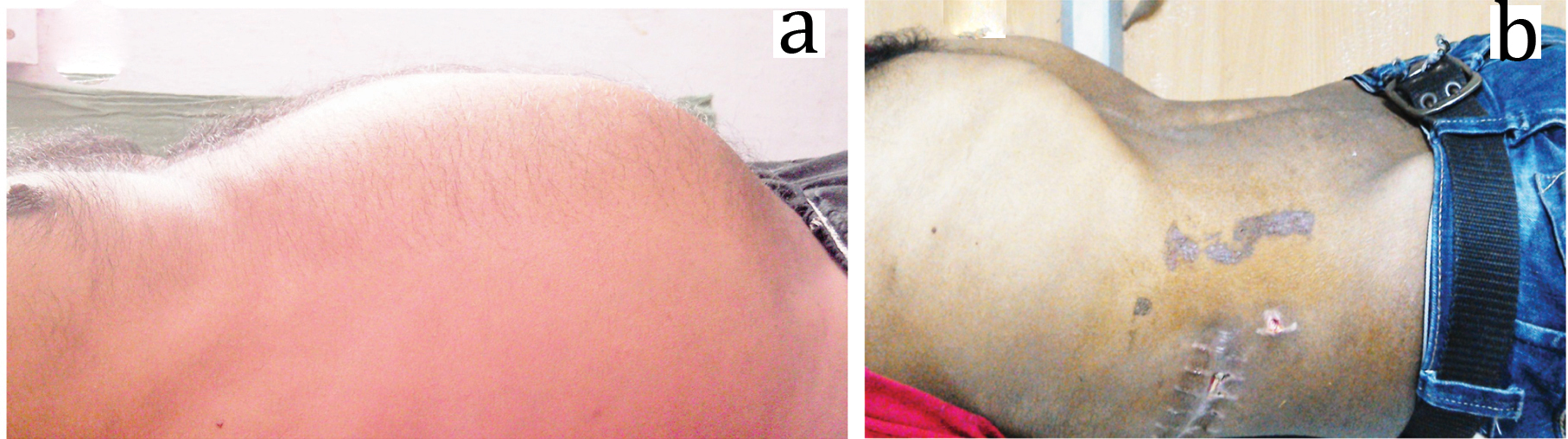
A 32-year-old male patient presented with complaints of gross haematuria for last two days and gradual distension of abdomen for last seven years. There was no history of fever, abdominal pain, any previous surgery, trauma, significant weight loss or stone disease. Haematuria subsided with conservative treatment after two days. General examination was essentially normal. On local examination, the right renal lump had crossed midline and occupied the almost whole of the abdomen [Table/Fig-1a,b]. Lump was nontender on palpation, with the smooth surface and tense cystic inconsistency. Urine for culture showed E.coli growth. In blood biochemistry haemoglobin was 11.2 gm%, total leucocytes count was 10200 cells/mm3. Blood level of urea and creatinine was 32 mg and 1.2 mg/dl respectively.
Patient’s abdomen picture in lateral view before and after operation respectively. Girth of the abdomen markedly reduced.
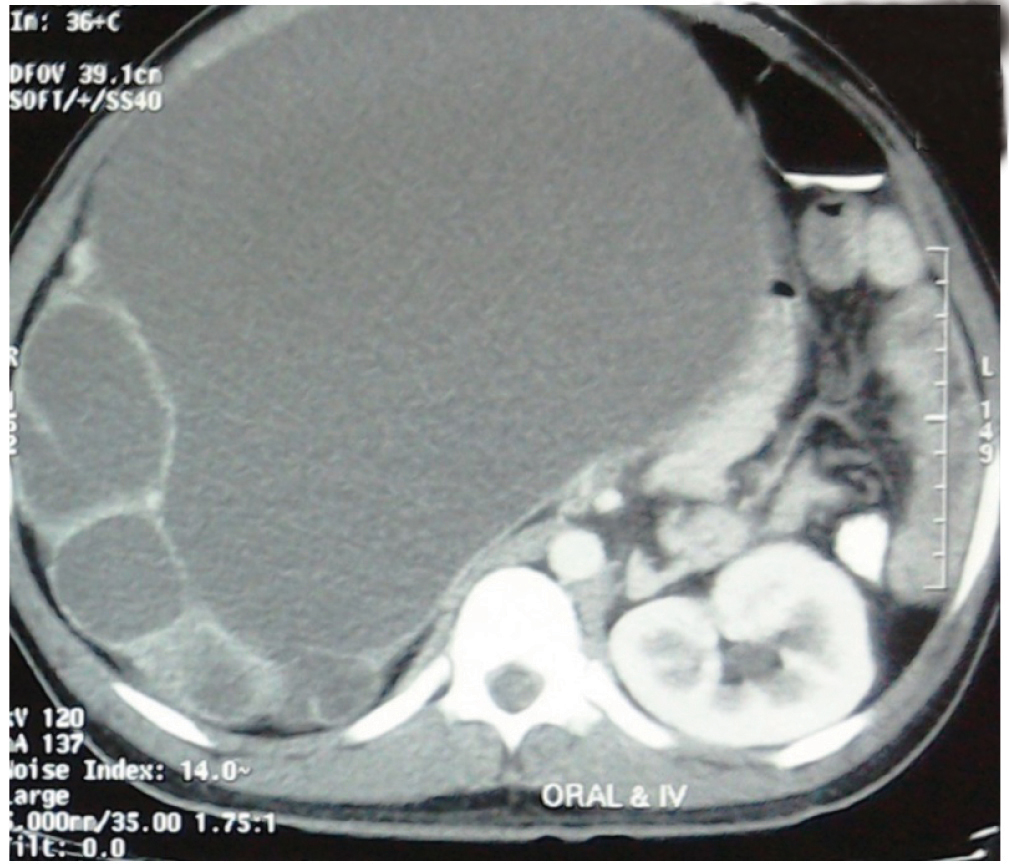
USG showed right sided large cystic kidney swelling with multiple thin septa occupying the whole of the abdomen from epigastrium to pelvis and left kidney was normal. Contrast Enhanced Computed Tomography (CECT) of Kidney, Ureter, Bladder (KUB) showed gross hydronephrotic kidney (30 cm x 26 cm x 20 cm) with multiple thin septa and thinned out parenchyma without any excretion [Table/Fig-2]. Left kidney was excreting well. CT report was suggestive of right-sided UPJ obstruction.
CECT KUB transverse section showing huge cystic swelling of right sided kidney containing clear fluid with multiple thin septa and thinned out parenchyma.
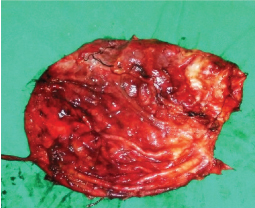
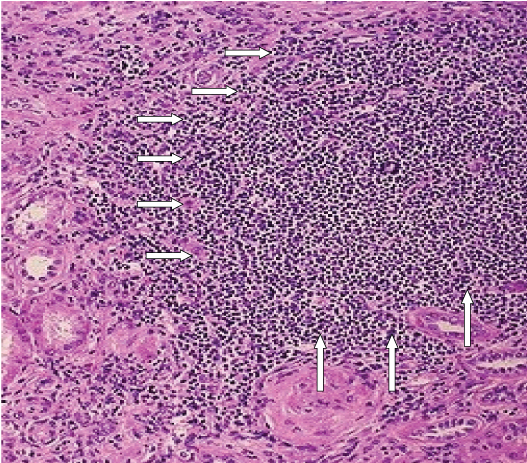
So, the provisional diagnosis was right sided giant hydronephrosis with non functioning kidney due to UPJ obstruction and right sided simple nephrectomy was planned. Open retroperitoneal approach was chosen because of large size swelling. Right sided subcoastal flank incision of about 12 cm was made. Abdominal layers and Gerota’s fascia had been opened and then cystic swelling was opened by small controlled incision. After opening, about 11 liters of frank pus sucked out and sample sent for culture [Table/Fig-3]. There was a moderate adhesion present, meticulous dissection was made in the perinephric plane, hilar vessels were controlled and kidney specimen has been removed [Table/Fig-4]. Culture from pus showed E.coli infection. Histology of the specimen was suggestive of chronic pyelonephritis [Table/Fig-5]. Postoperative recovery was uneventful. He was doing well in five months of follow up.
Containers filled with pus (11 liters of pus was drained out).

Macroscopic picture of right kidney specimen after simple nephrectomy. Reddish orange in colour, hydronephrotic kidney of 1230 gm with dimensions of 26 cm × 24 cm × 12 cm.
A low (10X) magnification image showing features of chronic pyelonephritic kidney with infiltration of chronic inflammatory cells (marked with arrows).
Discussion
Pyonephrosis is a suppurative infection of the upper urinary system which differs from infected hydronephrosis by the presence of frank pus. It is usually associated with parenchymal damage, chronic pyelonephritis and subsequent loss of kidney function [1]. Basically, main anatomical factor for pyonephrosis is the ureteric obstruction. Stone is the most common cause at least in 70% of pyonephrosis patients [2]. Obstructive causes can be divided into intrinsic (stone, fungal ball, papillary necrosis, clot, UPJ obstruction, upper urinary tract malignancy) or extrinsic (bladder tumour, prostate cancer, retroperitoneal tumour or lymph nodes, crossing lower pole vessels) [3]. The usual organism causing pyonephrosis are E.coli, Enterococcus, Klebsiella, Proteus and Pseudomonas [1]. E.coli was the culprit organism in our case.
Pyonephrosis most commonly present with flank pain, fever or chills [2]. Haematuria and abdominal lump are the uncommon presentations. A total of 15% of patients may remain asymptomatic. Infection in obstructed system may lead to fulminant infection like urosepsis especially in immunocompromised patients [3]. So, timely and effective intervention is very essential. Our patient presented with haematuria which expected to have due to trivial trauma or infection and surprisingly, there was no fever or pain present.
Diagnosis of pyonephrosis was made on clinical presentation, urine examination and radiological imaging. Radiological investigations usually helpful are USG, CT scan or MRI. CECT scan is very sensitive for diagnosis of pyonephrosis, to find out causative factor, to assess renal function, to assess perinephric inflammations and complications like the perinephric abscess, emphysematous pyelonephritis [1,3,4]. Percutaneous nephrostomy is used for both diagnostic and therapeutic purpose for pyonephrosis [1].
Treatment options of pyonephrosis include percutaneous drainage, retrograde ureteral stenting, pyeloplasty in a case of UPJ obstruction, stone management for urolithiasis and nephrectomy. Conservative treatment with antibiotics is not effective in pyonephrosis, surgical intervention usually required [5]. Percutaneous Nephrostomy (PCN) is usually initial treatment to drain obstructed system and to measure ipsilateral urine output, especially in septic patients because it is minimally invasive and effective method to drain Pelvicalyceal System (PCS) [1]. Ureteric stent is also an alternative to PCN for drainage in selective patients [5]. Nephrectomy is usually reserved for a patient with the non functioning kidney that is usually expected in long standing pyonephrosis [1]. In our case as right kidney was non functioning and opposite kidney was normal, so simple nephrectomy was performed.
More than 50% of the cases of giant distension of PCS had not diagnosed preoperatively. Differential diagnosis includes ascites, cystic ovarian mass (in female), mesenteric cyst and cystic retroperitoneal tumour. Erol A et al., had reported an almost similar case of giant pyonephrosis of size 13 cm x 24 cm x 34 cm (7 liters of pus) due to obstructed stone and they have done simple nephrectomy through large midline incision [6]. We have made a comparative smaller flank incision and used retroperitoneal approach. The kidney was decompressed in control way to achieve removal of large cystic mass through it. Hasigov A et al., recently reported a case of GP of size 23 cm x 30 cm x 27.9 cm due to urolithiasis and diabetes which was treated with open nephrectomy [7]. Although there is number of reported cases of giant hydronephrosis with more than 11 liters size [8] but giant pyonephrosis of such size is uncommon [6,7,9].
Conclusion
Pyonephrosis is an uncommon suppurative infection of the kidney due to ureteric blockage which may lead to renal insufficiency, septic shock and death. So, timely appropriate surgical intervention required to manage it. Open retroperitoneal approach is safe and effective for nephrectomy in GP patient.
[1]. Scarneciu I, Constantina A, Grigorescu D, Maxim L, Pyonephrosis: diagnosis and treatment: report of 65 casesJournal of Molecular Biology 2015 2:122-25. [Google Scholar]
[2]. Rabii R, Joual A, Rais H, Pyonephrosis: diagnosis and treatment: a review of 14 casesAnnales d’Urologie 2000 34(3):161-64. [Google Scholar]
[3]. Schaeffer AJ, Schaeffer EM, Wein A.J, Kavoussi L.R, Infections of the Urinary TractCampbell-Walsh Urology 2007 9th edPhiladelphiaSaunders Elsevier:223-96. [Google Scholar]
[4]. Fultz PJ, Hampton WR, Totterman SMS, Computed tomography of pyonephrosisAbdominal Imaging 1993 18(1):82-87. [Google Scholar]
[5]. Flukes S, Hayne D, Kuan M, Wallace M, McMillan K, Rukin NJ, Retrograde ureteric stent insertion in the management of infected obstructed kidneysBJU Int 2015 115(Suppl 5):31-34. [Google Scholar]
[6]. Erol A, Çoban S, Tekin A, A giant case of pyonephrosis resulting from nephrolithiasisCase Reports in Urology 2014 3:161640 [Google Scholar]
[7]. Hasigov A, Engbang JPN, Fidarov F, Giant pyonephrosis due to urolithiasis and diabetes: a case reportOpen Journal of Urology 2016 6:122-25. [Google Scholar]
[8]. Wang QF, Zeng G, Zhong L, Li QL, Che XY, Jiang T, Giant hydronephrosis due to ureteropelvic junction obstruction: A rare case report, and a review of the literatureMolecular and Clinical Oncology 2016 5(1):19-22. [Google Scholar]
[9]. Takashi M, Murase T, Sobajima T, Shimoji T, Miyake K, Mitsuya H, A case of malignant fibrous histiocytoma occurring in the retroperitoneum with giant pyonephrosisHinyokiko Kiyo 1983 29(8):911-19. [Google Scholar]