Autologous fat transfer is used for aesthetic and reconstructive surgeries like post traumatic defects, involutional disorders like hemifacial microsomia, facial atrophy, post radiotherapy sequalae, facial aging, wrinkles etc., are the few indications for fat transfer [1].
Neuber F was the first person to describe free autologous fat graft for soft-tissue augmentation [2]. Hollander performed fat infiltration for facial lipoatrophy in 1912 [3]. Miller published his experience with fat infiltration in 1926 [4].
The factors such as Rate of fat reabsorption, predictability and consistency related to this fat grafting procedure have been questioned time and again. One of the study reports 70% rate of resorption [5]. Lyndon Peer’s Cell survival theory says number of viable adipocytes transplanted correlates with the volume of the grafted fat that survives [6]. Pu LL et al., used different laboratory assays to know the viability. They were colorimetric assays, adipocyte- specific enzyme assays, histological examinations etc. The in-vitro studies by Pu LL et al., looked at fat grafts taken by excision, fat graft harvest and transfer device, conventional liposuction, Coleman technique. The results of their study favoured the Coleman technique as greater no of viable adipocytes are harvested and cells maintain a more optimal level of function [7,8].
However, there remains uncertainty regarding the viability of transferred fat. The lack of objective measurements of fat graft viability may be one of the reasons [9].
In this prospective study we studied the use of adipose cells in various procedures of plastic surgery, the role of High Resolution Ultrasound (HRUS) in estimating the volume of the grafted fat. Also, to compare the effectiveness of free fat transfer at contour irregularity areas depending on the site of free fat harvest (Donor areas – abdomen, buttock, thigh, and groin), the effectiveness of derma fat over free fat graft.
Materials and Methods
A prospective study was done from May 2012 till November 2013 at the Department of Plastic surgery, King George Medical University, Lucknow, Uttar Pradesh, India. The study was given clearance by the Ethical Committee. Patients who were planned for fat grafting procedure under local or general anaesthesia during above-mentioned period were selected. Clinical diagnosis was made after clinical history and physical examination.
Inclusion criteria: Patients with congenital abnormalities like hemifacial atrophy and microsomia, post traumatic, post scaring contour deformity in the craniofacial region, extremities, neck and trunk, asymmetry of the breasts, web space atrophy following nerve palsies due to leprosy (Hansen’s).
Exclusion criteria: Disorders of fat metabolism and systemic diseases affecting fat metabolism.
Fat grafting procedure: A written informed consent was taken before enrolling a total of 34 patients for the study. Patient demographic details, date of admission, history and duration of disease, mode of onset, progression, previous treatments, clinical examination, general examination, local examination-contour deformities and its dimensions, measurements in the form of longest and shortest-dimensions of the contour irregularity were noted. Baseline haematological parameters were checked.
For the surgery, abdomen/buttocks/thighs was prepared and draped. Under local anaesthesia through tiny incision in the umbilicus for abdominal fat, posterior hip iliac crest region for buttock fat, infiltrating solution was infiltrated in the intended subcutaneous areas of fat harvest. Fat was harvested using liposuction cannulas connected to 10, 20, 50 cc Luer lock syringes by applying vacuum mechanical way. Fat was stored in a sterile 20 cc syringes and were centrifuged at 3000 rpm for three minute. Donor site dressing was done and abdomen was strapped by dynaplast which stayed till two week time to prevent seroma.
Derma fat was harvested using no 15 blade in the groin crease and elliptical chunk of derma fat harvested. Epithelium was removed using no 15 blade. Wound closed in two layers using 4-0 vicryl and 4-0 nylon and was strapped with dynaplast.
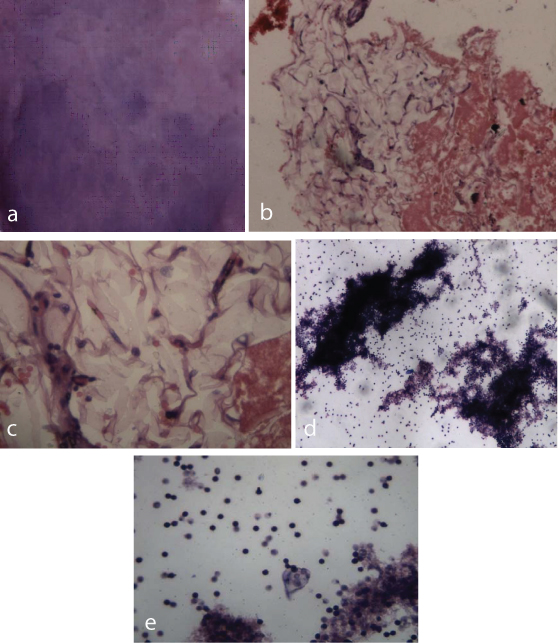
The middle layer in the centrifuged sample [Table/Fig-1b,c] was used for fat grafting and injected into the fat deficient areas in tiny aliquots by withdrawing the Coleman infiltration cannulas through tiny incisions. High power examination (HPE 10X, 20X and 40X) of the topmost and lowermost layer of the centrifuge sample is shown in [Table/Fig-1].
a) HPE (10X) of the top most layer of the centrifuged sample. Geimsa staining of the oil supernatant showing eosinophilic acellular staining; b) HPE (20X) of the middle fat layer H&E staining 20X view showing adipose cells admixed with haemorrhage; c) High power view (40X) of the H&E staining of the middle layer (fat) showing adipocytes (cells with agranular cytoplasm with nucleus pushed to the periphery). Also, seen is the blood vessel with RBC’s; d) HPE of the H&E staining lowermost serum layer (4X magnification) showing lymphoid cells and RBCs interspersed; e) HPE (40X) of the H&E staining of the lowermost serum layer mixed with blood (40X) showing leucocytes (majority of them being lymphocytes) and RBC’s interspersed.
Postoperatively patients were observed for two to four hours in the postoperative ward. They were started on normal diet after the procedure in case of local anaesthesia and after six hours in cases of general anaesthesia and discharged on the second day. General anaesthesia was used in patients who had to undergo secondary procedures in addition to fat grafting and required a high volume fat grafting. Abdominal binder/strapping with dynaplast was done for the donor abdominal site for two–six weeks’ time. Donor site wounds (in case of dermafat from the groin) were dressed after 48 hours and then every alternative day till the sutures were removed between 8-10 days.
Follow up: The patients were photographed immediately after the procedure, six months and at one year. Postoperative course, complications at donor and recipient site and follow up details were recorded. The volume estimation of the grafted fat using the high resolution ultrasound was done at six months and at one year interval.
HRUS was done with 10 and 12 MHz short focus high frequency linear transducers through direct contact scanning technique on Toshiba Neimo 30 ultrasound machine. Probe was put gently on site of fat graft with inert ultrasound gel. Scanning was done in transverse, longitudinal, antero- posterior planes. Grafted fat was found to be more echogenic than normal fat because of densely packed cells and it looks bright echogenic with homogenous consistency, can be easily differentiated from normal fat.
HRUS is a modality with a high sensitivity and specificity and has interobserver variations just like normal ultrasound. The intra observer variation was also eliminated by keeping the ultrasound probe gently over the grafted fat which did not allow the fat to get displaced and result in the alteration of the dimensions (in three planes) of the measured fat. The fatty infiltration in the surrounding areas of the fat grafted site such as in the atrophied muscles near the web spaces of hand, glands (parotid, submandibular etc.,) in the craniofacial region appears heterogeneous, fat appears hyper echoic, patchy density is seen as fat found is mixed with adjacent muscle/parenchyma. The injected fat appears well defined, uniformly homogenous with peripheral slight halo echo pattern with no intervening muscle/parenchymal echo pattern.
Statistical Analysis
The SPSS 17.0, was used for the analysis of the data and Microsoft word and Excel have been used to generate graphs, tables etc.
Results
The age range was between 10 and 50 years (distribution as shown in the [Table/Fig-2]. The mean age was 28.8 years. In this study there was a preponderance of male patients [18 (52.9 %) over female 16 (47.1%)].
| Age in years (mean-28.8 years) | No | % |
|---|
| 1-10 | 1 | 0.029 |
| 11-20 | 4 | 11.7 |
| 21-30 | 19 | 55.8 |
| 31-40 | 5 | 14.7 |
| 41-50 | 5 | 14.7 |
| Total | 34 | 100 |
The main driving reason for opting fat grafting was cosmesis in all the cases. The distribution of donor site for free fat graft is shown in the [Table/Fig-3].
Donor site for free graft.
| Abdomen | 19 | 55.8% |
| Thigh | 4 | 11.7% |
| Buttocks | 6 | 17.6% |
| Dermagraft | 5 | 14.7% |
Different anatomical areas where fat grafting was done are shown in [Table/Fig-4].
Anatomical sites – extremities and craniofacial where fat grafting was done.
| Parameters | Frequency | Percent (%) |
|---|
| Extremities |
| Web spaces | 15 | 44.1 |
| Elbow | 1 | 2.9 |
| Right thumb | 1 | 2.9 |
| Craniofacial |
| Cheek region | 4 | 11.8 |
| infra orbital region | 2 | 5.9 |
| Romberg’s syndrome | 1 | 2.9 |
| Hemifacial microsomia | 1 | 2.9 |
| Mandibular region | 4 | 11.8 |
| Neck | 1 | 2.9 |
| Temporo parietal region | 1 | 2.9 |
| Temporo parietal +cheek region | 1 | 2.9 |
| Poland’s syndrome | 1 | 2.9 |
| Lip | 1 | 2.9 |
| Total | 34 | 100.0 |
The largest sized defect was 8 x 6.6 cm in greatest dimensions in case of left hemifacial microsomia. The smallest sized defect was 3 x 2.8 cm in case of malar hypoplasia.
A total of 32 cases were operated under local anaesthesia and two cases were operated under general anaesthesia.
The mean volume of fat injected after centrifugation was 11.45 cc with range between 6-66 cc. The mean volume of excess correction was 3.23 cc with range between 2-20 cc [Table/Fig-5]. The mean duration time of surgery was 48 minute with range between 35–90 minute.
Duration of surgery, amount of injected fat and duration of stay.
| Parameters | Minimum | Maximum | Mean |
|---|
| Duration of surgery time donor site | 43 minutes Groin | 54 minutes Buttock | 48 minutes |
| Amount of injected fat amount donor site | 6 cc buttock | 66 cc Abdomen | 11.45 cc |
| Duration of stay | 2 hours | 48 hours | 4hours |
Fat atrophy was seen in all 34 cases. Nodularity was seen in one case of Poland’s syndrome. Unevenness was seen in one case of hemifacial microsomia. In one case of fat grafting done in the Poland’s syndrome unevenness at the donor site was seen and seroma was seen in the donor region of two patients who underwent derma fat graft for web space atrophy.
The mean percentage of retained free fat in the fat grafted area, when the donor was abdomen, was 57.9% at the end of 12 months. The mean percentage of retained free fat in the fat grafted area, when the donor was thigh, was 50.9% at the end of 12 months. The mean percentage of retained free fat in the fat grafted area, when the donor was buttock, was 66.7% at the end of 12 months. The mean percentage of retained derma fat was 80.9% at the end of 12 months of the estimated volume at six months. The mean percentage of the retained free fat was 70% at the end of the 12 months of the estimated volume at six months.
The retained fat volume at the end of 12 months in case of derma fat was 75% compared to a similar case of free fat where the retained fat at the end of 12 months was 45%.
Comparison between free fat grafting done in the extremities and craniofacial region immediately, at six months and at one year has been shown in [Table/Fig-6].
Comparison between free fat grafting done in the extremities (all volumes added up) and the free fat grafting done in the craniofacial region (all volumes added up).
| Parameters | Variables | N | Vol(in ml) | Mean | Percentage of fat (HRUS estimation) |
|---|
| Volume of fat injected | Extremities | 12 | 114 | 9.5 | 100% |
| Cranio facial | 14 | 145 | 10.3 | 100% |
| HRUS at six months | Extremities | 12 | 83.9 | 6.9 | 73.5% |
| Cranio facial | 14 | 92.1 | 6.5 | 63.5% |
| HRUS at one year | Extremities | 12 | 65.5 | 5.4 | 57.4% |
| Cranio facial | 14 | 60.1 | 4.2 | 41.4% |
Donor site complications included unevenness and seroma where derma fat graft was harvested in two cases. The unevenness in the anterior abdominal wall gradually decreased after constant use of pressure garment and massage. Seroma at the groin site was drained from the suture site and pressure dressing done. Recipient site complications included fat reabsorption in all cases, unevenness and nodularity in two cases. Slight bruising and swelling were not taken into account as complications. Slight bruising and oedema resolved in 7-14 days’ time.
Discussion
In this prospective study, a total of 34 patients were evaluated. Male patients were more compared to the female patients probably because many male patients had web space atrophy. The female patients opted for fat grafting mostly in craniofacial region for cosmesis.
The abdomen was the first choice for free fat as it is easy to harvest, the scar remains hidden and abdomen and has sufficient amount of fat. Dermafat was harvested from groin in five cases to compare it with free fat. about 57.4% of free fat was retained (53 cc) and 42.6% of free fat got reabsorbed (41 cc) at the end of 12 months in web space grafting patients. Free fat reabsorption was at the rate of 3.41 cc per month all cases put together. A total of 40.8% of free fat was retained and 59.2% of fat got reabsorbed at the end of 12 months in fat grafting patients done in craniofacial region.
In case of fat grafting done for Poland’s syndrome (Case Profile [Table/Fig-7] 42.4% of the fat was retained of the injected fat (66cc) and 57.6% of fat got reabsorbed.
a) Pre operative showing right breast hypoplasia (side view); b) Pre operative showing left breast hypoplasia; c) Intra operative (showing fat harvest); d) Immediate post operative; e) A six months post operative; f) A six months post operative; g) A one year post operative; h) A one year post operative (side view) i) HRUS at six months; j) HRUS at one year.
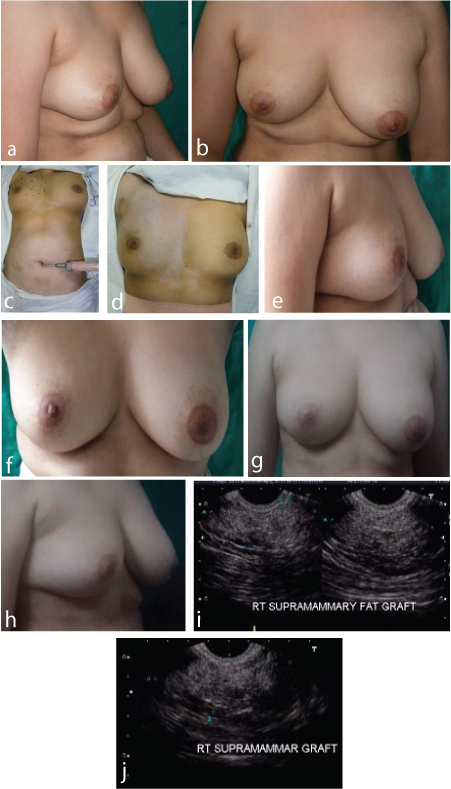
Free fat reabsorption was at the rate of 2.6 cc per month. In case of fat grafting done for contour defect in the elbow region 46.9% of the fat was retained of the injected fat (17cc) and 53.1% of the fat got reabsorbed. Free fat reabsorption was at the rate of 0.66 cc per month.
The mean percentage of retained free fat at the end of 12 months as estimated on HRUS was 57.9%, 50.9%, 66.7% when donor area was abdomen, thigh and buttock respectively.
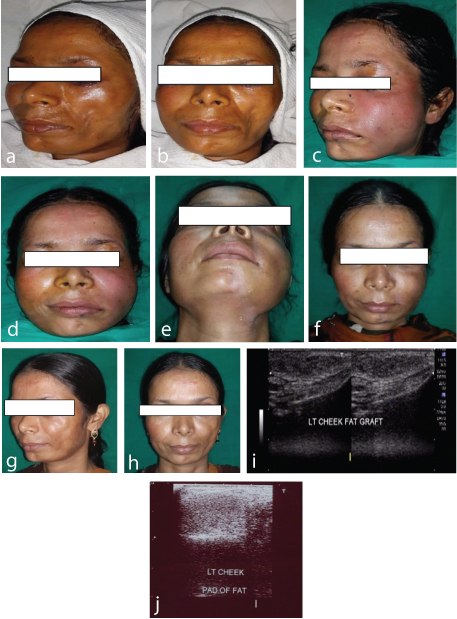
An observation was made that the grafted fat in the craniofacial region reabsorbed (atrophied) faster than in cases where fat grafting was done in the extremities but no statistical significance found on analysis.
The reason probably is the effect of the muscle contractions (which bring about facial expressions) (Case profile [Table/Fig-8] which is in action for most of the time.
a) Pre operative showing left cheek hypoplasia (side view); b) Pre operative left cheek hypoplasia; c) Immediate post operative (side view); d) Immediate post operative; e) A six months post operative; f) A six months post operative; g) A one year post operative (side view); h) A one year post operative; i) HRUS six months; j) HRUS at one year.
The patients were followed up till one year for photography and documentation. A total of 31 patients visited regularly till the end of one year.
In our case series, fat grafting was performed only once in all the cases of contour deformity be it in craniofacial or extremities. It was a conscious decision to do fat grafting procedure only once. The second procedure in a short interval will also bring some variation in the accurate analysis of volume estimation. seven patients out of 34 were found to require one more sitting of fat grafting procedure at the end of 12 months [Table/Fig-9].
Comparison between our and other similar studies on various parameters.
| Variables | Our study | Other studies |
|---|
| Age range | 10-50 years | 20-40 years [10] |
| Male/females | 18/16 | 19/64 [10] |
| Fat grafting | 15 cases of web spaces and 15 cases of craniofacial | 64 cases craniofacial region [11] |
| Dermafat grafting | Used in webspace atrophy and lip defects | Used for aesthetic correction [12,13] |
| Main driving reason for fat grafting | Cosmesis | Cosmesis [10] |
| Donor site for harvest | Abdomen, thigh, buttock and thighs | Extremities, trochanteric area, inner knee, dorsocervical fat pad, abdominal and flank [12] |
| Anaesthesia | Local anaesthesia - 32 General anaesthesia -2 | Majority local anaesthesia [12] |
| Mean duration of surgery | 52 minutes | 60 minutes [10] |
| Volume at the end of 12 months | Average- 45% | Average - 40% [14] |
| Volume estimation of grafted fat | High resolution ultrasound | 3D photography [14] Computed tomography [9] |
| Follow up | Photography immediate post operative, one month, six months, twelve months | Every three months for 26 months [12] |
| No of sittings | Seven out of 34 needed second sitting at the end of 12 months | Majority need 1-3 sittings at 3-6 months [10] |
Overall, graft volume loss, via reabsorption or necrosis, is the primary cause of poor results. Initial over correction can often compensate for this outcome [15]. Overall uptake rate of fat grafting ranges from about 50%-90%, additional procedures are always necessary to achieve an optimal result [16]. However, there is no study, which has addressed the timing of subsequent fat grafting. Both Coleman [17] and Perez [18] have noted six-month longevity with fat transfer to the hands, but one to three touch-up procedures were required for better cosmesis. Also, study of fat filling in the face revealed that cigarette smoking causes low fat survival rates and impairs the improvement of skin quality, successful results can be obtained with facial lipofilling in the smokers [19]. Survival rate varied from 34% to 82% in breast and 30%–83% in the facial area. Nude mice were studied to investigate human fat grafting survival rate (38.3%–52.5% after 15 weeks) [20].
A study conclude low-pressure liposuction and minimal centrifugation should be used to gently extract and purify the adipose tissue with minimal trauma. Even and diffuse reinjection of the fat increases graft-to-recipient interface, reduces interstitial fluid pressure and increases fat survival [21].
In the present study, donor site complications included unevenness and seroma where derma fat graft was harvested in two cases. The unevenness in the anterior abdominal wall gradually decreased due to constant pressure from garments and massage. Seroma at the groin site was drained from the suture site and pressure dressing done. Recipient site complications included fat reabsorption in all cases, unevenness and nodularity in two cases. Slight bruising and swelling were not taken into account as complications, which got resolved in 7-14 days time. Guijarro-Martínez R et al., also reported in their article the complications regarding the donor and recipient sites comparable to our study [11].
Other area where fat grafting is utilized is irradiated skin. Study revealed fat grafting resulted in decreased dermal thickness, decreased collagen content, and increased vascular density in irradiated skin. CT analysis revealed significantly decreased fat graft survival in the irradiated group when compared to the non-irradiated group. Study concluded although fat graft retention rates are significantly lower in irradiated than non-irradiated tissue, the quality of retained fat between the groups is similar [22].
Fat grafting has been utilized in a study as a novel therapeutic option in the delaying the progress of the Raynaud phenomenon in the hands. The study concluded that preliminary results of fat grafting to the hands of patients with Raynaud phenomenon revealed improved symptomatology with evidence suggestive of measurably increased perfusion in some cases [23].
Limitation
The sample size was not sufficient to validate the advantages of fat grafting procedure. There are inherent limitations of HRUS. Also, the follow up duration was less.
Conclusion
Autologous fat transfer is a good option for contour corrections at various anatomical sites.
Most of the times fat grafting procedures can be done under local anaesthesia. Fat atrophy/reabsorption and seroma (donor site) is the most common complication. Significant difference in the fat atrophy between the cases of free fat and derma fat. Volume of fat is maintained for a longer time in cases of derma fat. Grafted fat in the craniofacial region is reabsorbed early. Thus, autologous fat transfer is a safe procedure however the biggest disadvantage is, the fat reabsorption needs multiple corrections.
HRUS for volume estimation is a handy, non-invasive, multi planar modality, does not require any preparation, and easily done outdoor procedure. Follow up is a practical proposition.